Abstract
Background
Because of the individuality of the palatal rugae, they are applicable for human identification purposes the same as the fingerprints. Therefore, it is important to assess the effect of different factors on rugae characteristics. We assessed the characteristic changes of the palatal rugae following extraction and expansion during orthodontic treatments. Before and after orthodontic treatment dental casts of 30 patients were scanned by 3Shape Trios 3D intraoral scanner, and superimposed in Geomagic X 2018 software. Displacement of 13 reference points was analyzed in three dimensions. The length of the palatal rugae was also measured. SPSS version 22.0 was applied for data analysis, using independent t test, sample t test, and chi-square test.
Results
The alterations in the mean palatal rugae length were significant in the first right and third right ridges after extraction, and right and left second ridges after expansion treatment (P < 0.05). Changes in coordinates in the X, Y, and Z axes were significant at 8 points on the rugae after extraction, and 5 points after expansion treatment (P < 0.05). The changes in the sum of means of displacements were significant at all 13 points after extraction and expansion treatments (P < 0.05).
Conclusions
The palatal rugae do not remain stable during expansion and extraction orthodontic treatments. Some changes occurred in length, and the most medial and most lateral points on each ridge were displaced. The length of the incisive papilla did not change during treatment; thus, it can serve as a stable landmark. If we consider palatal rugae as an individual landmark, we can refer the patients after orthodontic treatment for scanning of their palatal rugae to document their post treatment pattern; but it should be noted that treatment relapse may change it again.
Similar content being viewed by others
Background
Palatal rugae, also known as the transverse palatine fold or plica palatine, are three to five irregular fibrous connective tissue elevations located in the anterior aspect of the hard palate mucosa at each side of the median palatal raphe and behind the incisive papilla; they never cross the mid-palatal raphe (Almeida et al. 1995; Shetty et al. 2013; Sivaraj 2013).
The palatal rugae start to form in the 12th to 14th weeks of prenatal life because the connective tissue core is embedded deeply between the stratum reticulum of the palate and the submucosal fatty tissue (Patil et al. 2008). The palatal rugae are well formed at birth, and have a typical orientation pattern. They reach their final characteristic shape during the adolescence, and remain stable throughout life (Carrea 1937; Yamazaki 1962).
The palatal rugae comprise a small part of the oral cavity, and are often protected against high temperatures and trauma because of their specific location. They play a role in deglutition, and enhance the contact of taste receptors and food in the tongue dorsal surface. They are also involved in speech and sucking in children (Bushtova 2003; Ohtani et al. 2008; Shukla et al. 2011; Thomas 1972). Due to the stability and individuality of palatal rugae, they are applicable as reference on diagnostic casts in orthodontic treatment, and their orientation pattern may also be used for identification purposes in forensic medicine when fingerprints or DNA analysis are not available. Moreover, the palatal rugae resists postmortem decomposition alterations for seven days following death, and is able to resist massive thermal damages, like third-degree burns (Caldas et al. 2007; Sweet and DiZinno 1996). The palatal rugae can be used for sex identification (Malekzadeh et al. 2018; Pakshir et al. 2019).
Palatoscopy or palate rugoscopy is the study of the palatal rugae to establish the identity of the individuals (Patil et al. 2008; Thomas et al. 1986). Palatal rugae are permanent and unique in each individual and thus, they are applicable to identify purposes (Patil et al. 2008; Shetty et al. 2013). However, some studies disagree with this statement, and explain that identification cannot be done only according to the palatal rugae. Also, there is a controversy regarding the stability of the qualitative and quantitative features of the palatal rugae in the process of growth and development, orthodontic treatment, and some surgical procedures (Deepak et al. 2014; Graber et al. 2017; Johal et al. 2007).
The Palatal Rugae Comparison Software was designed and tested by Hemanth et al, in 2010 who showed that the palatal rugae had an accuracy of 99% for identification and individualization purposes (Hemanth et al. 2010).
Considering the increasing prevalence and severity of some of the malocclusions, demand for orthodontic treatment has increased for esthetic and functional purposes (Brin et al. 1998). During fixed orthodontic treatment for space discrepancies, extraction or non-extraction protocols may be adopted based on the esthetic and functional considerations. The non-extraction fixed orthodontic treatment is based on the arch expansion, while the extraction orthodontic treatment is based on extractions of the premolar teeth.
Several studies compared the palatal rugae pre- and post-orthodontic treatment and identified the stable points and ridges of the rugae; however, the selected points and ridges were not the same across different studies (Abdel Aziz and Sabet 2001; Bailey et al. 1996; Damstra et al. 2009; Kapoor and Miglani 2015; Shukla et al. 2011). Thus, rugoscopy appears to have the potential to identify an individual even after orthodontic treatment (Pateria and Thakkar 2011).
In 2015, Mustafa et al. claimed that the palatal rugae are special for each person both before and after orthodontic treatment, but alterations in the characteristics of rugae and their displacement can complicate their application for identification purposes (Mustafa et al. 2015). However, another study claimed that the rugae pattern and morphology would remain stable during orthodontic treatment and throughout life (Bansode and Kulkarni 2009).
Another study assessed the uniqueness of the palatal rugae for personal identification by a 3D software (Gibelli et al. 2018). However, most studies that compared the palatal rugae in pre and post-orthodontic treatment cases assessed them two-dimensionally; they mostly compared the changes by defining some points on the palatal rugae and measuring the distance between them by a caliper or ruler (Abdel Aziz and Sabet 2001; Bailey et al. 1996; Damstra et al. 2009; Shukla et al. 2011). Nonetheless, another study claimed that 2D assessment of the palatal rugae is insufficient, and their 3D assessment is necessary (Taneva et al. 2015).
A more recent study assessed the changes in the palatal rugae during orthodontic treatment by superimposition of palatal rugae images by a Digital Image Recognition System (Wu et al. 2017) and also by 3D superimposition technique (Gujar and Rani 2016). Therefore, it was possible to study the points only in two dimensions. Accordingly, the authors of the present study aimed to find reference points that remain constant during both extraction and non-extraction orthodontic treatments for later use in forensic identification. Based on previous studies, the authors decided to scan the casts by a 3D scanner and compare the points in three dimensions by a digital software to find possible changes in shape and dimensions of the palatal rugae by 3D superimposition. Given that some points are found to remain stable during fixed orthodontic treatment, the palatal rugae can be scanned and saved as an identification document in the profile of every individual. Moreover, they can be as useful as fingerprints, and may be suitable for use as an alternative since fingerprints may vanish over time. Thus, we assessed the characteristic changes of the palatal rugae following extraction and expansion orthodontic treatments. Our hypothesis is that both types of fixed orthodontic treatments can change the orientation of palatal rugae points in three plans.
Methods
Records of 30 patients with available pre-orthodontic and post-orthodontic dental casts were prepared from the archives of the Department of Orthodontics, School of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran.
Fifteen cases had been treated by fixed orthodontic treatment with palatal expansion without any extraction and the remaining 15 ones had been treated with fixed orthodontic treatment and extraction of the first premolars without any expansions.
The inclusion criteria were as follow; absence of air bubbles or voids in the anterior one-third of the palate in the casts, no history of skull or jaw trauma, permanent dentition, no missing teeth before starting the orthodontic treatment, and duration of fixed orthodontic treatment to be over 12 months.
The exclusion criteria were as follows: congenital anomalies, palatal deformity, active lesions, scars or trauma in the oral cavity, history of cleft lip and/or palate, history of wearing a maxillary denture, and smoking.
The ethic committee of Shiraz University of Medical Sciences approved the study (IR.SUMS.DENTAL.REC.1398.79).
Initial impressions of orthodontic cases were taken by alginate impression material, and the casts were poured with dental stone. The study casts were scanned by 3Shape Trios 3D intraoral scanner (TRIOS Color-P13 Shade, 3Shape Dental Systems, Denmark), and the output scanned information was kept in Standard Triangulation Language (STL) format.
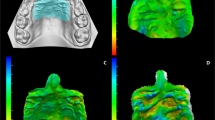
The casts were analyzed by the Geomagic® Control X™ version 2018, (Geomagic Inc., Morrisville, NC, USA), a 3D analysis software. The Geomagic Control X 2018 is a 3D precision measurement instrument for metrology and quality control that can be applied to analyze the differences between two 3D designed meshes for quality control of produced parts. Thus, it was applied to evaluate the tissue changes after orthodontic treatment by comparing the pre-treatment and post-treatment dental casts. For this purpose, first the before and after-treatment casts were superimposed in the software. The Geomagic Control X 2018 has a unique analysis pattern. First, we used the transform alignment tool to choose the stable reference points on the mid-palatal raphe on each cast, and performed the primary superimposition by using these points. Next, we used the best fit alignment tool to increase the quality of the superimpositions. Then, we used the 3D compare tool for assessment of differences between the two meshes which reveals the changes in tissues by color scale.
For more precise comparison of the points, they were numbered and measured by a vector and then the measurements were analyzed. The points were defined according to a study by Taneva et al (Taneva et al. 2015).
Two adequately trained examiners (a biomedical engineer with a PhD and a senior dental student) selected the references points (the posterior point of the IP and the most medial and lateral end points of the palatal rugae [R1MR, R1ML, R1LR, R1LL, R2MR, R2ML, R2LR, R2LL, R3MR, R3ML, R3LR, and R3LL] under the supervision of an orthodontist by consensus. These landmarks have been marked following a previous study (Taneva et al. 2015).
The patients may have three to seven pairs of rugae ridges, but each cast had to have at least three pairs of rugae ridges; thus, we only analyzed the points on the first, second, and third rugae ridges.
The coordinates of these points were identified and compared based on the displacement of each point as follows (Fig. 1):
-
X axis: medial-lateral
-
Y axis: superior-inferior
-
Z axis: anterior-posterior
In the next step, the length of the rugae was recorded from the starting point at the mid-palatine raphe to the endpoint of rugae transversely. In circular shapes, the maximum diameter was measured. The length was also measured by Geomagic Control X 2018 using its measure distance tool that can measure a linear distance between two entities. The values were all reported in millimeters (mm).
After 1 week, the examiners repeated the superimposition and point selection for 20 casts randomly (10 before treatment and 10 after treatment casts). Also, length measurement was done and intraclass correlation coefficient (ICC) was calculated to assess the intra-examiner’s reliability.
The data were exported to IBM SPSS version 22.0 for further analysis. Independent t test, sample t test, and chi-square test were applied for comparison of the mean values and analyzing the correlation between the variables.
Results
Comparison of pre- and post-treatment rugae length (in mm) between the extraction and expansion groups
The mean length change of each rugae after treatment was measured and compared (Table 1). In the extraction group, the variation in length before and after treatment was statistically significant in the first right rugae ridge and third right rugae ridge (p < 0.05). The differences in length pre- and post-treatment were not significant for the right second rugae ridge, first, second, and third left rugae ridges, and also the incisive papilla (p > 0.05).
In the expansion group, the variations in length before and after treatment were statistically significant in the right second rugae ridge and left second rugae ridge (p < 0.05) and not significant for the first and third rugae ridges at each side and also for the incisive papilla (p > 0.05).
Comparison of changes in coordinates of palatal rugae landmarks after treatment in extraction and expansion groups
The mean change in 3D position of the end points at each side of the palate after treatment was assessed. There were 52 variables related to the positional changes of the most medial as well as most lateral points of each rugae ridge in three dimensions of X (medial-lateral direction), Z (anterior-posterior direction) axes, and Y (superior-inferior direction) and the sum of vectors in all three dimensions.
In the extraction group (Table 2), the mean displacement of R3MR, R1ML, R2LL, and R3LL in X axis, R3MR, R1LL, R2LL, R3ML and R3LL in Y axis, and R2MR, R3MR, R3LR, R1LL, R2LL, R2ML, R3LL, R3ML in Z axis was significant (P < 0.05). But, the mean displacement of IP, R1MR, R1LR, R2MR, R2LR, R3LR, R1LL, R2ML, and R3ML in X axis, IP, R1MR, R1LR, R2MR, R2LR, R3LR, R1ML, and R2ML in Y axis, and IP, R1MR, R1LR, R2LR, and R1ML in Z axis was not significant (P > 0.05)
The mean displacement of IP, R1MR, R1LR, R1ML, R1LL, R2MR, R2ML, R3LR, R3MR, R3ML, and R3LL in X axis, IP, R1MR, R1LR, R2MR, R3MR, R3LR, R1LL, R2LL, R2ML and R3ML in Y axis, and IP and all rugae ridges except R1LR in Z axis was not significant (P > 0.05); however, the mean displacement of R2LR and R2LL in X axis, R1ML, R2LR, and R2LL in Y axis and R1LR in Z axis was significant (P < 0.05) in the expansion group (Table 3). The scan before and after orthodontic treatment in one of the samples of this group and their superimposition are shown in Fig. 2.
The mean sum of displacement of all the studied points on rugae and the incisive papilla was statistically significant in both extraction and expansion groups (P < 0.05).
The difference in the mean displacement of R1ML, R2LL, R3MR, and R3LL in X axis, R1MR, R2LL, and R3MR in Y axis, and R2ML, R3ML, and R3LL in Z axis was significant between the extraction and expansion groups (P < 0.05). However, the differences in IP, R1LR, R1MR, R1LL, R2LR, R2MR, R2ML, R3LR, and R3ML in X axis, IP, R1LR, R1ML, R1LL, R2LR, R2MR, R2ML, R3LR, R3ML, and R3LL in Y axis, and IP, R1LR, R1MR, R1ML, R1LL, R2LR, R2MR, R2LL, R3LR, and R3MR in Z axis were not significant between both groups (P > 0.05).
A significant difference was found in the mean sum of displacement of R1LR, R2LR, R3LR, R2LL, and R3LL between the expansion and extraction groups (P < 0.05) (Table 4).
The ICC value was computed for all repeated measurements. In all cases, all ICC values were greater than 0.80 and significant. Therefore, acceptable level of reliability was observed for the measurements.
Discussion
This observational before-after study was performed to evaluate the stability of palatal rugae following fixed orthodontic treatment with extraction of first premolars without expansion and fixed orthodontic treatment with palatal expansion without extraction. The stability and individuality of the palatal rugae has been widely assessed (Bansode and Kulkarni 2009; De Angelis et al. 2012; Saraf et al. 2011; Thomas and van Wyk 1988), and the pattern of rugae with respect to sex and race, and their potentials as an identification tool been evaluated. (Bansode and Kulkarni 2009; Kalia 2005; Kallianpur et al. 2011; Malekzadeh et al. 2018; Pakshir et al. 2019).
It has been reported that the palatal rugae remain stable during one’s life (Patil et al. 2008), and their morphological pattern is applicable for identification purposes as a replacement for fingerprints due to their individuality and stability (Limson and Julian 2004; Muthusubramanian et al. 2005). Nonetheless, some others claimed that external factors such as orthodontic treatment may cause changes in shape, length, number and location of rugae ridges and points (Damstra et al. 2009; Kapoor and Miglani 2015; Mustafa et al. 2015).
Different methods are available for rugoscopy. Previous studies assessed the palatal rugae changes in two dimensions, and mostly considered the transverse and anteroposterior changes between the points of palatal rugae (Abdel Aziz and Sabet 2001; Pateria and Thakkar 2011). This classic length measurement ignores the changes in the vertical (superior-inferior) axis. Moreover, external factors such as orthodontic treatment were studied by several investigators to find the stable points or patterns to aid in forensic identification (Bailey et al. 1996; Shetty et al. 2013; Shukla et al. 2011).
The positional changes of the reference points that were three-dimensionally evaluated in the present study were statistically significant in both extraction and expansion groups, regardless of the measurement axis. The most posterior site of the incisive papilla was not significantly displaced in any axis, but the sum of its displacement was significant. It has been reported that changes in the most posterior site of the incisive papilla may occur during orthodontic treatment. Positional changes of this point may be caused by the movement of incisors or inflammation or edema due to gingivitis or gingival overgrowth following orthodontic treatment (Taneva et al. 2015).
In total, the sum of changes of the palatal rugae in the extraction group in different axes was more than that in the expansion group, and it appears that the palatal rugae experienced a greater change in the process of extraction during orthodontic treatment than the expansion.
In the extraction group, the results indicated that the third ridge was not stable at all, and the first and second rugae ridges partly remained the same but they were more stable than the third ridge, which was in contrast to a study that introduced the third rugae ridge as a stable landmark (Abdel Aziz and Sabet 2001). The impact of tooth movement on the palatal rugae cannot be neglected as mentioned in previous studies (Almeida et al. 1995; Bailey et al. 1996). Bailey et al, and Peavy and Kendrick reported that extraction of first premolars can create a large areas for distal retraction of maxillary anterior teeth, affecting the position of the first rugae ridge lateral points and change the transverse distance between them, which can be confirmed by the present results in 3D evaluation of the landmarks (Bailey et al. 1996; Hoggan and Sadowsky 2001; Lysell 1955; Peavy Jr and Kendrick 1967). Our findings are in agreement with those of Hausser reporting that the lateral points of the rugae moved forward following the teeth movement in extraction cases, however, the medial rugae points were not affected (Hausser 1951; Hoggan and Sadowsky 2001). Another group of studies reported that the medial parts of the third palatal rugae ridge showed the most appropriate and stable reference points to assess anteroposterior tooth movement in orthodontic treatments (Almeida et al. 1995; Hoggan and Sadowsky 2001; Shukla et al. 2011). However, Bansode and Kulkarni claimed that skeletal changes may occur during orthodontic treatment but they did not affect the palatal rugae (Bansode and Kulkarni 2009). Contrary to our results, Taneva et al. showed that all the reference points that did not change significantly except for the most posterior site of the incisive papilla could be used for human identification (Taneva et al. 2015). In our research, the stability of landmarks was higher in the expansion group compared to the extraction group, and no point experienced the alterations in all three dimensions.
Regarding the length of rugae, the mean changes in both the right and left second rugae ridges were significant in the expansion group. The alterations in length were significant for the first and second right rugae ridges in the extraction group. Therefore, it may be concluded that the length of the first, second and third left rugae ridges and second right rugae ridges was stable during fixed orthodontic treatment using extraction of first premolars, and the length of first and third rugae ridges remained stable after fixed orthodontic treatment with palatal expansion, when merely relying on 2D measurements. The length of the incisive papilla did not change significantly; thus, the length of the incisive papilla may be used as a stable landmark. There was some asymmetry in the results between the right and left sides. Some changes in the rugae length were shown by Deepak et al. after orthodontic treatment. They reported an increase in rugae length in palatal expansion and non-extraction cases in the right side; no difference was observed in this group in the left side (Deepak et al. 2014). In our research, the changes in the second rugae length were symmetrical in the expansion group.
Wu et al. analyzed the palatal rugae images by MATLAB software and reported the accuracy of superimposition of palatal rugae patterns for forensic identification to be 100%. The accuracy of the digital image recognition system used for superimposition of palatal rugae patterns prior to and following orthodontic treatment was 95.67%. They claimed that the resolution of palatal rugae images directly affected the accuracy of identification (Wu et al. 2017). This accuracy differences in orthodontic cases could be the result of changes in palatal rugae landmarks. It should be put in consideration that we used the Geomagic software with an accuracy of 0.0001 mm; thus, the chance of finding significant differences increased. Therefore, it can be recommended that a highly accurate software is a better option for such assessments in forensic medicine. However, the limitation of our study was the small sample size which we suggest a larger sample size for the future studies.
Conclusions
Based on this 3D study, we could conclude that the palatal rugae do not remain stable during orthodontic treatments. Changes occurred in length, and the most lateral and medial points on each rugae were displaced.
The changes in the length and displacement of points were not correlated, and they changed independently. Thus, they could not be reliable as stable landmarks for identification purposes for those who had fixed orthodontic treatments. The length of the incisive papilla did not change during orthodontic treatment; thus, it may serve as a stable landmark. If we consider the palatal rugae as an individual landmark, we can refer the patients after orthodontic treatment for scanning of their palatal rugae to document their pattern; but it should be noted that treatment relapse may change the palatal rugae pattern again which should be investigated in the future studies.
Availability of data and materials
The dataset used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICC:
-
Intraclass correlation coefficient
References
Abdel Aziz H, Sabet N (2001) Palatal rugae area: a landmark for analysis of pre-and post-orthodontically treated adult Egyptian patients. East Mediterr Health J 7(1-2):60–66
Almeida MA, Phillips C, Kula K, Tulloch C (1995) Stability of the palatal rugae as landmarks for analysis of dental casts. Angle Orthod 65(1):43–48
Bailey LTJ, Esmailnejad A, Almeida MA (1996) Stability of the palatal rugae as landmarks for analysis of dental casts in extraction and nonextraction cases. Angle Orthod 66(1):73–78
Bansode SC, Kulkarni MM (2009) Importance of palatal rugae in individual identification. J Forensic Dent Sci 1(2):77
Brin L, Zwilling-Sellam O, Harari D, Koyoumdjisky-Kaye E, Ben-Bassat Y (1998) Does a secular trend exist in the distribution of occlusal patterns? Angle Orthod 68(1):81–84
Bushtova M (2003) The development of palatal rugae in the European pine vole, Microtus subterraneus (Arvicolidae, Rodentia). Folia Zoo 52:127–136
Caldas IM, Magalhaes T, Afonso A (2007) Establishing identity using cheiloscopy and palatoscopy. Foren Sci Int 165(1):1–9
Carrea JU (1937) La Identificacion humana por las rugosidades palatinas: Las Ciencias
Damstra J, Mistry D, Cruz C, Ren Y (2009) Antero-posterior and transverse changes in the positions of palatal rugae after rapid maxillary expansion. Eur J Orthod 31(3):327–332
De Angelis D, Riboli F, Gibelli D, Cappella A, Cattaneo C (2012) Palatal rugae as an individualising marker: reliability for forensic odontology and personal identification. Sci Justice 52(3):181–184
Deepak V, Malgaonkar NI, Shah NK, Nasser AS, Dagrus K, Bassle T (2014) Palatal rugae patterns in orthodontically treated cases, are they a reliable forensic marker? J Int Oral Health 6(5):89–95
Gibelli D, De Angelis D, Pucciarelli V, Riboli F, Ferrario VF, Dolci C, Cattaneo C (2018) Application of 3D models of palatal rugae to personal identification: hints at identification from 3D-3D superimposition techniques. Int J Legal Med 132(4):1241–1245
Graber LW, Vanarsdall RL, Vig KWL, Huang GJ (2017) Orthodontics : current principles and techniques
Gujar A, Rani M (2016) Three-dimensional assessment of the palatal contour changes in orthodontically treated cases: A scanned maxillary cast analysis. J Indian Orthod Soc 50(3):145–149
Hausser E (1951) The palatal ridges in man; their significances and their modifications. Stoma 4(1):3–26
Hemanth M, Vidya M, Shetty N, Karkera BV (2010) Identification of individuals using palatal rugae: Computerized method. J Foren Dent Sci 2(2):86–90
Hoggan BR, Sadowsky C (2001) The use of palatal rugae for the assessment of anteroposterior tooth movements. Am J Orthod Dentofac Orthop 119(5):482–488
Johal A, Cheung M, Marcenes W (2007) The impact of two different malocclusion traits on quality of life. Br Dent J 202(2):E2
Kalia KP (2005) Palatal rugae pattern in Mysorean and Tibetan populations. J Dent Res 16(2):51–55
Kallianpur S, Desai A, Kasetty S, Sudheendra U, Joshi P (2011) An anthropometric analysis of facial height, arch length, and palatal rugae in the Indian and Nepalese population. J Forensic Dent Sci 3(1):33–37
Kapoor P, Miglani R (2015) Transverse changes in lateral and medial aspects of palatal rugae after mid palatal expansion: a pilot study. J Forensic Dent Sci 7(1):8–13
Limson K, Julian R (2004) Computerized recording of the palatal rugae pattern and an evaluation of its application in forensic identification. J Forensic Odontostomatol 22(1):1–4
Lysell L (1955) Plicae palatinae transversae and papilla incisiva in man; a morphologic and genetic study. Acta Odontol Scand 13(Suppl. 18):5–137
Malekzadeh AR, Pakshir HR, Ajami S, Pakshir F (2018) The Application of Palatal Rugae for Sex Discrimination in Forensic Medicine in a Selected Iranian Population. Iran J Med Sci 43(6):612–622
Mustafa AG, Allouh MZ, Alshehab RM (2015) Morphological changes in palatal rugae patterns following orthodontic treatment. J Forensic Legal Med 31:19–22
Muthusubramanian M, Limson K, Julian R (2005) Analysis of rugae in burn victims and cadavers to simulate rugae identification in cases of incineration and decomposition. J Forensic Odontostomatol 23(1):26–29
Ohtani M, Nishida N, Chiba T, Fukuda M, Miyamoto Y, Yoshioka N (2008) Indication and limitations of using palatal rugae for personal identification in edentulous cases. Forensic Sci Int 176(2-3):178–182
Pakshir F, Ajami S, Pakshir HR, Malekzadeh AR (2019) Characteristics of palatal rugae patterns as a potential tool for sex discrimination in a sample of iranian children. J Dent (Shiraz) 20(1):1–9
Pateria A, Thakkar K (2011) Palatal rugae a stable landmark-A comparison between pre and post orthodontic patients. Int J Dent Clinics 3(4):9–12
Patil MS, Patil SB, Acharya AB (2008) Palatine rugae and their significance in clinical dentistry: a review of the literature. J Am Dent Assoc 139(11):1471–1478
Peavy DC Jr, Kendrick GS (1967) The effects of tooth movement on the palatine rugae. J Prosthet Dentist 18(6):536–542
Saraf A, Bedia S, Indurkar A, Degwekar S, Bhowate R (2011) Rugae patterns as an adjunct to sex differentiation in forensic identification. J Forensic Odontostomatol 29(1):14–19
Shetty D, Juneja A, Jain A, Khanna KS, Pruthi N, Gupta A, Chowdhary M (2013) Assessment of palatal rugae pattern and their reproducibility for application in forensic analysis. J Forensic Dent Sci 5(2):106–109
Shukla D, Chowdhry A, Bablani D, Jain P, Thapar R (2011) Establishing the reliability of palatal rugae pattern in individual identification (following orthodontic treatment). J Forensic Odontostomatol 29(1):20–29
Sivaraj A (2013) Significance of palatal rugae in orthodontics. J Orofac Res 3(3):202–209
Sweet D, DiZinno J (1996) Personal identification through dental evidence--tooth fragments to DNA. J Calif Dent Assoc 24(5):35–42
Taneva ED, Johnson A, Viana G, Evans CA (2015) 3D evaluation of palatal rugae for human identification using digital study models. J Forensic Dent Sci 7(3):244–252
Thomas C (1972) Incidence of primary O rugae in Bushman juveniles. J Dent Res 51(2):676–676
Thomas C, Kotze T, Nash J (1986) The palatal ruga pattern in possible paternity determination. J Forensic Sci 31(1):288–292
Thomas CJ, van Wyk CW (1988) The palatal rugae in an identification. J Forensic Odontostomatol 6(1):21–27
Wu X-P, Han J-N, Fen P, Wan Y-J, Bing L, Xiu-Ping W, Li B (2017) Analysis of palatal rugae morphology before and after orthodontic treatment by a digital image recognition system. Int J Morphol 35(2):420–424
Yamazaki Y (1962) Cross-sectional study of plicae palatinae transversae in the Japanese. Anthropol Rep Niigata 34:59–76
Acknowledgements
This manuscript is based on the thesis by Dr. Nazanin Ziar. The authors thank Dr. Vosoughi of the center for research improvement of the school of Dentistry for the statistical analysis.
Funding
The authors thank the Vice-Chancellory of Shiraz University of Medical science for supporting this research (Grant No.: 19764).
Author information
Authors and Affiliations
Contributions
Conceptualization: ShA. Methodology: HP. Formal analysis: NZ. Writing—original draft preparation: NZ. Writing—review and editing: YA. Visualization: ShA. Supervision: HP. Project administration: ShA. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The trial was approved by the local ethical committee of Shiraz University of medical science. (No: IR.SUMS.DENTAL.REC.1398.79) Informed consent form was obtained from those individuals participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ziar, N., Pakshir, H.R., Alamdarloo, Y. et al. Characteristic changes of the palatal rugae following orthodontic treatment. Egypt J Forensic Sci 13, 14 (2023). https://doi.org/10.1186/s41935-023-00334-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41935-023-00334-5