Abstract
The Palatal Rugae are considered a useful human identification marker for both orthodontists and forensic personnel. The principal aim of the present study was to evaluate the stability of palatal rugae with a 3D-3D superimposition procedure following Slow Maxillary Expansion (SME), in order to assess whether they kept their uniqueness and validity for human identification, even after a specific dental treatment. For this purpose, a sample of 27 digital dental models - belonging to growing patients (13 males and 14 females), aged between 8.5 and 15 years, who underwent SME therapy - was retrospectively studied and compared with a control group of 27 untreated subjects - (13 males and 14 females). Digital dental models were obtained pre-treatment and at device removal; both were processed by means of an intraoral scanner. A superimposition procedure was thus performed to reach the minimum point-to-point distance between two models of palatal rugae. Intra- and inter-observer differences were statistically analyzed by paired Wilcoxon test and Intra-class Correlation coefficient (ICC), showing values larger than 0.93. There was no difference in Root-Mean-Square (RMS) values between untreated control subjects and subjects treated with Leaf Expander (p = 0.062). A RMS value of 0.43 was the threshold to distinguish the pooled group (“Untreated” and “Leaf”) from any mismatch. According to the obtained results, this study failed to reject the null hypothesis and presented no differences between the RMS values of the Test group and the RMS values of the untreated control group. This work highlighted the usefulness of 3D superimposition procedure for purposes of human identification, in subjects undergoing dental treatment. However, keeping in sight the forensic use of this technique as a helpful probation element in court, further studies should be performed to confirm these findings.
Similar content being viewed by others
Introduction
The analysis of Palatal Rugae, also known as Plicae Palatinae Transversae and Rugae Palatinae, is one of the most reliable methods for human identification, mostly in cases of corpses that lack valuable dental information during major disasters1,2,3. Due to its uniqueness, stability throughout the whole life and their resistance to diseases and several extraoral environmental damages - such as the action of high temperatures and maceration- the palatal rugae have been widely studied in the last decades in order to verify their validity as an identification marker4,5,6.
In the last decades, few researches have been carried out to analyze the changes in the palatal rugae morphology submitted to some orthodontic treatments such as, for example, the Palatal Expansion7,8,9. Applying this type of orthopedic forces to the maxillary arch to expand itself in growing subjects during the correction of malocclusions, could cause significant morphological changes to the rugae10,11,12,13. There are many types of maxillary expansion methods and various recommended expansion rates, which can result in Rapid Maxillary Expansion (RME hereafter)12,13 or Slow Maxillary Expansion (SME hereafter)14. According to the literature15, in case of SME, skeletal transversal width is present but reported to be lower than dento-alveolar expansion. Unfortunately, evidence on changes of the palatal rugae following SME is inconclusive16,17.
In children, growth is expected to occur in the rugae region, affecting both palatal depth and surface area. Therefore, verifying the palatal rugae stability in growing subjects could be even more challenging18,19,20.
In this study, the effects of SME on the palatal rugae patterns and stability were assessed in a sample of 3D digital dental models of Italian growing subjects for the first time. The advantages of digital study models include easy and fast storage, transfer of data, immediate access and virtual simulation21,22. In addition, the accuracy of direct digital models added the plug-and-play capability of an automatic exchange of information21.
Although the validity of these models has been widely studied for human identification, a method for superimposing pre- and post-treatment digital dental models is still under evaluation. Some previous studies showed that the medial 2/3 of the third rugae, and the regional palatal vault dorsal to the third rugae, are stable regions that can be used for 3D digital model superimposition23,24. In another research25, the morphological characteristics of the palatal rugae were examined in a Korean sample of 343 adult subjects. The results indicated that the numbers of the palatal rugae varied greatly among individuals and this could affect the antero-posterior position of the third primary ruga. More recently, a metrical assessment of point-to-point differences between two three-dimensional (3D) models of the upper dental arch was used to test the discriminating potential of 3D image of palatal rugae26. The authors showed that the palatal rugae are unique and stable, and that 3D image acquisition systems could contribute to the morphological and metrical assessment of these particular structures. Finally, the “Identity Base” (IB) system was introduced to develop a complex information system and a personal identification protocol by means of three-dimensional palatal scans in digital format27.
The present study aimed to evaluate the stability of palatal rugae with a 3D-3D superimposition procedure following SME to determine if they can be used as an appropriate reference area for human identification in forensic context. Thus, the null hypothesis (H0) presented no differences between the RMS values of the Test group and the RMS values of the untreated control group needed to be assessed.
Material and Methods
Sample
A retrospective study was carried out, in which digital dental casts of orthodontically treated growing patients were evaluated at two different intervals: before and after treatment. The subjects sample were collected from the database of the UOC Chirurgia Maxillo Facciale e Odontostomatologia - Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico - Department of Biomedical Surgical and Dental Sciences University of Milan (Italy). Informed consent was obtained, before dental treatment, from the parents and/or legal guardians of all subjects who were younger than 18 years for study participation.
Digital dental models were obtained pre-treatment and at device removal, and processed by means of an intraoral scanner: 3Shape D250 (3Shape, Copenhagen, Denmark). The validity and precision of the scanner are both of ±0.05 mm.
Subjects were selected according to the following eligible criteria: Early or mid-mixed dentition, with both primary and second molars (E + E hereafter) preserved, Cervical Vertebral Stage 1 through 3 (CVS methods 1–3), Angle Class I or Class II malocclusion, no previous orthodontic treatments and maxillary arch constriction. The exclusion criteria were as follows: The presence of craniofacial abnormalities, previous extraction or surgical treatment, Angle Class III malocclusion, Temporomandibular Joint (TMJ hereafter) dysfunctions or caries of E. Test group consisted of 27 subjects (13 males - 14 females), mean age of 8.5 ± 1.5 years old, who underwent SME (Leaf Expander) therapy. The devices were banded by the same operator on the primary second molars.
The expanders presented the same type of screw (6 mm – 450 g) with an anterior arm up to the canines; no subsequent orthodontic treatment was to either the maxilla nor the mandible. The expander was activated following the protocol previously described24. All the expanders were removed after a period of 9 to 11 months. The specific amount of expansion in each single case was not evaluated, although the expansion was clinically achieved in all the subjects treated.
The Control group consisted of 27 subjects with maxillary arch constriction (13 males and 14 females), mean age of 8.5 ± 1.5 years, and whom had not received any treatment for at least 10 months. The control selection criterion was the same to the criteria of the experimental group selection.
Among all the possible combinations, 35 mismatches were randomly selected in order to compare the results with the matching groups (untreated Control and Leaf). The “Mismatches” group is represented by the overlap of different subjects.
Superimposition
Only one superimposition procedure was performed to study the differences between the pre and post-treatment models in the palatal rugae area. According to literature24, this area is relatively stable during an individuals’ whole life.
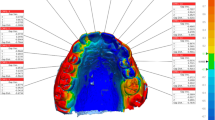
During the first step, the palatal area including the rugae were manually selected and then isolated from both pre and post-treatment models (Fig. 1A). Then, the models of the two obtained palatal areas were automatically superimposed by VAM software (VECTRA Analysis Module, version 3.7.6, Fairfield, New Jersey), through a best-fit algorithm, in order to reach the best match between them. In this case, since an automatic best-fit superimposition method was used, fiduciary maxillary stable structures or reference points were not considered.
(A) Example of a 3D-scanned digital model of the palatal area; (B) Chromatic representation of differences between two superimposed models in “Untreated Control” subjects; (C) Chromatic representation of differences between two superimposed models in “Leaf” subjects before and after SME; (D) Chromatic representation of differences between two superimposed models in case of mismatches. Green means perfect match whereas yellow and red mean areas of discordances between the two digital models.
After the two areas were registered, the software was requested to provide the point-to-point distance between the entire registered surfaces. The superimposition results were illustrated in a difference map, in which discrepancies (in mm) are represented through a color-coded scale: The green meant perfectly matching surface, the red meant test model surface was positively positioned - relative to reference model - and the blue meant test model surface was negatively positioned, relative to reference model.
Statistical analysis
Sample size was calculated a priori, based on a primary outcome Root Mean Square (RMS hereafter), as continuous outcome to obtain a statistical power of the study greater than 0.85, using the mean values and standard deviations of RMS found by Gibelli et al.26. RMS is the square root of the arithmetic mean of the squares of the point-to-point distance between the areas with an identical coordinate system, while the achieved errors are measured in the same units as the obtained response. Based on these parameters, the sample size required was 25 patients in each group.
To determine the error of method, RMS calculation was repeated 7 days after the first measurement was performed on 15 randomly selected casts, by the same observer (FR) and by a second observer (GC) - two senior orthodontists with varying levels of experience. The individual observer’s analyses were not disclosed to the other observer.
Intra and inter-observer differences were statistically analyzed by paired Wilcoxon test. In addition, the Intra-class Correlation coefficients (ICC) were calculated.
Shapiro-Wilk’s test showed that RMS data were normally distributed, therefore parametric statistics were thus applied. Descriptive statistics, median value, standard deviation and 95% Confidence Interval (CI) were calculated. Differences between groups were computed with an ANOVA test and post-hoc Bonferroni tests. Probabilities of less than 0.05 were accepted as significant in all statistical analyses (except for the Bonferroni test for which the accepted probability was 0.017). All statistical analyses were performed using IBM SPSS Statistics ver. 21.0 software (IBM, Armonk, NY, USA), with significance level set at p < 0.05.
Compliance with Ethical standards
This study has been approved by the Local Ethic Committee, Fondazione IRCCS Ospedale Maggiore Policlinico, Milan, Italy (Prot. n° 421, 09/03/2016). The study was carried out in accordance with the ethical standards laid down by the Declaration of Helsinki (Finland).
Results
The ICC values for the intra- and inter-observer agreement were 0.955 (95% CI: 0.931–0.980; p < 0.001) and 0.936 (95% CI: 0.918–0.975; p < 0.001). Overall, the method error was considered negligible.
Most of the superimposed surfaces were green, which indicates that the reference model and the test model had corresponded with each other. Cross-bites and traversal maxillary discrepancies were corrected at the end of the active expansion phase in 100% of the subjects treated with the Leaf expander. The RMS threshold was found to be statistically different in the three analyzed groups. Two subjects for each group were excluded due to inaccurate scans in the palatal area. The final sample consisted of 25 subjects for the test group (12 boys and 13 girls) and 25 subjects for the control group (13 boys and 12 girls).
Subjects in the “Untreated Control” group reported an average RMS of 0.28 (95% CI 0.24–0.35); the “Leaf” group reported a comparable value to the normal RMS group of 0.34 (95% CI 0.31–0.43). These two groups represented the overlap of the same subject and there was no difference in mean RMS values between untreated subjects and those treated with Leaf Expander (p = 0.062). The “Mismatches” group is represented by the overlap of different subjects and the RMS value is statistically higher (0.71, 95% CI 0.58–0.81) compared to the “Untreated Control” group (p < 0.001) and “Leaf” (p < 0.001). In no case the values of the groups “Untreated Control” and “Leaf” were superimposed with those of the “Mismatches” group (Fig. 1B–D, and Table 1): RMS value of 0.43 was the threshold to distinguish the pooled group (“Untreated Control” and “Leaf”) from the Mismatches (Fig. 2).
Discussion
Method
Rugae patterns had previously been studied as anatomical structures and identification markers in several cases: between different subjects and ethnicity, in cases of edentulous subjects and for subjects following orthodontic treatment (expansion or extractions). Different methodologies were also applied to evaluate their anatomical uniqueness and overall stability: intraoral inspection, impressions, plaster casts, digital models, digital photography and stereophotogrammetry28,29,30. 3D models have been proven to be an effective tool and as an alternative method for evaluating palatal rugae patterns in human identification28,29,30. In addition, superimposing 3D digital models is a practical, user-friendly and relatively quick and inexpensive method that could be suitable for specific forensic scenarios, in which identification of an individual is needed.
This study is the first to thoroughly test the effect of SME on superimposition of serial 3D digital dental models obtained by using intraoral scans in a sample of growing subjects aged between 8.5 and 15 years, submitted to this kind of treatment.
Best-fit Superimposition Procedure (i.e. the search for maximum correspondence between two models) is more precise and requires a greater calculation effort of the computer since the procedure is repeated until the difference between the surfaces is minimized. In this case, the RMS and SD values of the distance between the two models indicate how accurate the process is, once the images have been superimposed on the centroid.
It has been widely demonstrated that intraoral scanning may be more accurate, compared to digital models generated by desktop-scanning of conventional impression/plaster models31. In fact, direct digitization by means of the intraoral scanner had less systematic errors than the physical model fabrication step with a milling machine from an intraoral scan. In general, the main advantages of intraoral scanners are the following: (1) increased adoption in clinical practices worldwide; (2) different models of portable cart-free systems with a single USB cable - that can be plugged into any workstation - can be developed; (3) improved accuracy of the directly obtained digital models; (4) lost devices could easily be refabricated using the digital files from a database in the “Cloud”21; (5) they consume less time and reduce patient exposure to unnecessary radiation, thus being very useful in forensic contexts.
Patients
Patients younger than 15 years were recruited because of the growth activity of the palatal suture had been reported to reduce around 14 years of age32. In fact, the optimal age for SME or RME would be below 13 to 15 years of age, when growth of the mid-palatal suture typically have ceased11,12.
To date, although possible modifications of the palatal rugae have been widely discussed as a consequence of some dental treatments, they have not been properly treated in the forensic literature8,33. According to published studies8,34,35, the shape of the palatine rugae remained consistent with different orthodontic treatment modalities and very limited changes have been observed in their orientation. However, based on certain orthodontic procedures related to maxillary expansion and front tooth restoration treatments, length of palatal rugae has been shown to vary such as: significant increases in the third rugae length during RME, or significant reductions in the second and third rugae length after the extraction treatment.
Results
The obtained results pointed out that this study failed to reject the Null hypothesis (H0): there were no differences between the RMS values of the Test group and the RMS values of the untreated control group. A small RMS value implied that the estimated mean was close to the true mean, indicating in turn that the estimated SD was close to RMS and the best-fit superposition was accurate and precise (see Table 1). Therefore, this study showed that the use of orthodontic treatments, specifically SME, did not significantly alter the pattern of the palatal rugae in the growing subjects. This is consistent with the findings of previous studies26,36. When a comparison is carried out, both the RME and SME were able to produce some changes, but RME generated greater orthopedic changes. In general, the maxillary expansion caused more dento-alveolar and buccal tipping than skeletal expansion36.
Forensics
Eventually, in regards to the intra and inter-observer errors, they were considerably negligible showing that this method is precise and highly reproducible. In the forensic field, reproducible means that, with known probability, different examiners obtain the same result when analyzing the same samples37. On the other side, precision refers to the closeness of a value to the real one35,38. Therefore, a strong system must be capable of giving consistent measurements, regardless of who is operating it and with what37,39.
This study proved that rugoscopy has potential to contribute to human identification, despite certain orthodontic treatment modalities affecting the anteroposterior or transverse dimensions of the palate. This work also highlighted its validity as an additional tool, along with the dentition and genetic analyses, for assessing the identity of an individual in several forensic contexts or when identification by routine methods such as fingerprints analysis is not possible. In fact, the palate is resistant to the action of fire and maceration because of its fibrous structure (keratinized tissue) and anatomically protected position2.
It means that the 3D comparison of palatal rugae area can be applied reliably to support positive identifications in court because uniqueness and stability guarantee that a subject examined postmortem can be linked exclusively to the same area (from a missing person) examined antemortem.
Some limitations should be highlighted when interpreting the data of the present research. Although the palatal rugae area are relatively stable during an individual’s whole life24, the sample of this study was mainly limited to Italian growing subjects aged between 8.5 and 15 years, and the morphological changes of palatal rugae area, over a longer period, were not analyzed. Future studies with a longitudinal sample should be performed to evaluate if significant differences are observed in the palatal area because of changes that the palatal mucosa endure over a couple of years to longer term40.
Keeping in mind the forensic use of this technique as a helpful probation element in court2,30,37,39,41, further studies - using increased number of observers with different levels of experience, larger sample size, different dental treatment such as the Rapid Maxillary Expansion (RME) and various patient groups - are recommended to confirm and generalize the accuracy of these findings. Extended training of an operator is also necessary and should be focused on the quality and quantity of the material available and its impact on the uniqueness of this type of forensic evidence. Finally, various samples from different countries should be considered in order to compare these findings with other populations42.
Conclusions
For the first time, within the limitations of this study, it has been demonstrated that the 3D anatomical morphology of the palatal rugae area is not affected by specific dental treatments, thus indicating that it can maintain its morphological patterns of individuality even after undergoing SME. The superimposition process is highly reproducible and provides, in a simple and inexpensive way, accurate results. The lack of differences statistically significant between the pre- and post-treatment models supports and gives reliability for the forensic applications based on the comparison of the morphology of palatal rugae.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author, on a reasonable request.
References
Hauser, G., Daponte, A. & Roberts, M. J. Palatal rugae. J. Anat. 165, 237–249 (1989).
Caldas, I. M., Magalhães, T. & Afonso, A. Establishing identity using cheiloscopy and palatoscopy. Forensic. Sci. Int. 165, 1–9 (2007).
Adisa, A., Kolude, B. & Ogunrinde, T. J. Palatal rugae as a tool for human identification. Niger J. Clin. Pract. 17(5), 641–643 (2014).
Bing, L., Wu, X. P., Feng, Y., Wang, Y. J. & Liu, H. C. Palatal rugae for the construction of forensic identification. Int. J. Morphol. 32(2), 546–550 (2014).
Hermosilla Venegas, V., San Pedro Valenzuela, J., Cantín López, M. & Suazo Galdames, I. C. Palatal rugae: systematic analysis of its shape and dimensions for use in human identification. Int. J. Morphol. 27(3), 819–825 (2009).
Pretty, I. A. Forensic dentistry: 1. Identification of human remains. Dent. Update. 34(10), 621–22, 624–6, 629–30 passim (2007).
Pateria, A. H. & Thakkar, K. Palatal rugae a stable landmark-a comparison between pre and post orthodontic patients. Int. J. Dent. Clin. 3(4), 9–12 (2011).
Batool, A., Shaikh, A. & Mubassar, F. Stability of Palatal Rugae as a Forensic Marker in Orthodontically Treated Cases. J. Forensic Sci. 61(5), 1351–1355 (2016).
Damstra, J., Mistry, D., Cruz, C. & Ren, Y. Antero-posterior and transverse changes in the positions of palatal rugae after rapid maxillary expansion. Eur. J. Orthod. 31(3), 327–332 (2009).
Kapoor, P. & Miglani, R. Transverse changes in lateral and medial aspects of palatal rugae after mid palatal expansion: A pilot study. J. Forensic Dent. Sci. 7(1), 8–13 (2015).
Saadeh, M., Macari, A., Haddad, R. & Ghafari, J. Instability of palatal rugae following rapid maxillary expansion. Eur. J. Orthod. 39(5), 474–481 (2017).
Bucci, R. et al. Dental and skeletal effects of palatal expansion techniques: a systematic review of the current evidence from systematic reviews and meta-analyses. J. Oral. Rehabil. 43, 543–564 (2016).
Di Ventura, A. et al. Three-dimensional evaluation of rapid maxillary expansion anchored to primary molars: direct effects on maxillary arch and spontaneous mandibular response. Eur. J. Paediatr. Dent. 20(1), 38–42 (2019).
Cossellu, G., Biagi, R., Faggioni, G. & Farronato, G. Orthodontic Treatment of Binder Syndrome: A Case Report with 5 Years of Follow-up. Cleft Palate Craniofac. J. 52(4), 484–8 (2015).
Maspero, C., Galbiati, G., Giannini, L. & Farronato, G. Sagittal and vertical effects of transverse sagittal maxillary expander (TSME) in three different malocclusion groups. Prog. Orthod. 25(16), 6 (2015).
Zhou, Y. et al. The effectiveness of non-surgical maxillary expansion: a meta-analysis. Eur. J. Orthod. 2, 233–242 (2014).
Lagravère, M. O., Major, P. W. & Flores-Mir, C. Skeletal and dental changes with fixed slow maxillary expansion treatment: a systematic review. J. Am. Dent. Assoc. 136(2), 194–199 (2005).
Hicks, E. P. Slow maxillary expansion: a clinical study of the skeletal versus dental response to low-magnitude force. Am. J. Orthod. 73(2), 121–141 (1978).
Corbridge, J. K., Campbell, P. M., Taylor, R., Ceen, R. F. & Buschang, P. H. Transverse dentoalveolar changes after slow maxillary expansion. Am. J. Orthod. Dentofacial. Orthop. 140(3), 317–325 (2011).
Kim, H. K., Moon, S. C., Lee, S. J. & Park, Y. S. Three-dimensional biometric study of palatine rugae in children with a mixed-model analysis: a 9-year longitudinal study. Am. J. Orthod. Dentofacial. Orthop. 141, 590–597 (2012).
Taneva, E., Kusnoto, B. & Evans, C. A. 3D Scanning, Imaging, and Printing in Orthodontics, Issues in Contemporary Orthodontics, Farid Bourzgui, Available from: https://www.intechopen.com/books/issues-in-contemporary-orthodontics/3d-scanning-imaging-and-printing-in-orthodontics (IntechOpen, 2015).
Akyalcin, S., Cozad, B. E., English, J. D., Colville, C. D. & Laman, S. Diagnostic accuracy of impression-free digital models. Am. J. Orthod. Dentofacial. Orthop. 144(6), 916–922 (2013).
Chen, G. et al. Stable region for maxillary dental cast superimposition in adults, studied with the aid of stable miniscrews. Orthod. Craniof. Res. 14, 70–79 (2011).
Vasilakos, G., Schilling, R., Halazonetis, D. & Gkantidis, N. Assessment of different techniques for 3D superimposition of serial digital maxillary dental casts on palatal structures. Sci. Rep. 7(1), 5838 (2017).
Choi, S. H., Kyongmin, K., Kee-Joon, L., Chung-Ju, H. & Jung-Yul, C. Analysis of the Morphological Characteristics of the Palatal Rugae for Three-Dimensional Superimposition of Digital Models in Korean Subjects. Biomed Res. Int. https://doi.org/10.1155/2018/3936918.
Gibelli, D. et al. Application of 3D models of palatal rugae to personal identification: hints at identification from 3D-3D superimposition techniques. Int. J. Legal Med. 132, 1241–1245 (2018).
Pacifici, A., Gargari, M. & Pacifici, L. 3D software scanning, processing and archiving palatal rugae: “identity base” technology. J. Biol. Regul. Homeost. Agents 32(5), 1291–1294 (2018).
De Angelis, D., Riboli, F., Gibelli, D., Cappella, A. & Cattaneo, C. Palatal rugae as an individualising marker: reliability for forensic odontology and personal identification. Sci. Justice 52(3), 181–184 (2012).
Muthusubramanian, M., Limson, K. S. & Julian, R. Analysis of rugae in burn victims and cadavers to simulate rugae identification in cases of incineration and decomposition. J. Forensic Odontostomat. 23(1), 26–29 (2005).
Limson, K. S. & Julian, R. Computerized recording of the palatal rugae pattern and an evaluation of its application in forensic identification. J. Forensic Odontostomatol. 22(1), 1–14 (2004).
Tomita, Y. et al. Accuracy of digital models generated by conventional impression/plaster-model methods and intraoral scanning. Dent. Mater. J. 37(4), 628–633 (2018).
Melsen, B. Palatal growth studied on human autopsy material A histologic microradiographic study. Am. J. Orthod. 68, 42–54 (1975).
Sivaraj, A. Significance of palatal rugae in orthodontics. J. Orofac. Res. 3(3), 202–209 (2013).
Li, B. et al. Model analysis of anatomical morphology changes of palatal rugae before and after orthodontic treatment. Int. J. Morphol. 35(4), 1224–1229 (2017).
Mustafa, A. G., Allouh, M. Z. & Alshehab, R. M. Morphological changes in palatal rugae patterns following orthodontic treatment. J. Forensic. Leg. Med. 31, 19–22 (2015).
Barbieri, A. A. et al. The evidence of the rugoscopy effectiveness as a human identification method in patients submitted to rapid palatal expansion. J. Forensic Sci. 58(Suppl 1), S235–238 (2012).
Saks, M. J. & Khoeher, J. J. The individualization fallacy in forensic science evidence. Vand. L. Rev. 61(1), 199–219 (2008).
Patil, M. S., Patil, S. B. & Acharya, A. B. Palatine rugae and their significance in clinical dentistry: a review of the literature. J. Am. Dent. Assoc. 139(11), 1471e8 (2008).
Murphy, E. The new forensics: criminal justice, false certainty, and the second generation of scientific evidence. Cal. L. Rev. 95, 721–797 (2007).
Taneva, E. D., Johnson, A., Viana, G. & Evans, C. A. 3D evaluation of palatal rugae for human identification using digital study models. J. Forensic Dent. Sci. 7(3), 244–252 (2015).
Strom, K. & Hickman, M. Unanalyzed evidence in law enforcement agencies: a national examination of forensic processing in police departments. Criminol. Public. Pol. 9, 381–404 (2010).
Lanteri, V. et al. Comparison between RME, SME and Leaf Expander in growing patients: a retrospective postero-anterior cephalometric study. Eur. J. Paediatr. Dent. 19(3), 199–204 (2018).
Acknowledgements
The authors would like to thank Ms. Jannet Ly for her diligent proofreading of this paper.
Author information
Authors and Affiliations
Contributions
V.L. conception and design of the work, interpretation of data, drafting the work; G.C. conception and design of the work, interpretation of data, drafting the work; A.U. analysis of data and drafting the work; M.F. contributions to the conception and revised it critically; R.L. conception of the work and revised it critically; F.R. the acquisition of data and drafting the word; S.D. interpretation of data and drafting the work; R.B. design of the study and revised it critically; C.M. design of the study and revising it critically. All authors read and approved the final manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lanteri, V., Cossellu, G., Farronato, M. et al. Assessment of the Stability of the Palatal Rugae in a 3D-3D Superimposition Technique Following Slow Maxillary Expansion (SME). Sci Rep 10, 2676 (2020). https://doi.org/10.1038/s41598-020-59637-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-59637-5
- Springer Nature Limited
This article is cited by
-
Digital matching of palatal rugae patterns for forensic identification in edentulous denture wearers
Forensic Science, Medicine and Pathology (2024)
-
Effect of light-emitting photobiomodulation therapy on the rate of orthodontic tooth movement
Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie (2023)
-
Distal extension of palatal rugae as a limitation for donor soft tissue grafts in a Jordanian population: A cross-sectional study
BMC Oral Health (2021)
-
Genetic variants in bone morphogenetic proteins signaling pathway might be involved in palatal rugae phenotype in humans
Scientific Reports (2021)