Abstract
Aim
To explore the existing salivary, gingival crevicular fluid (GCF), blood, and serum biomarkers associated with grade C molar-incisor pattern (C/MIP) periodontitis in systemically healthy children and young adults.
Materials and methods
Cross-sectional, case–control, and cohort studies on stage III grade C periodontitis or former equivalent diagnosis with analysis of molecular biomarkers in saliva, GCF, blood, or serum were retrieved from six databases and screened based on the eligibility criteria. The risk of bias in included studies was evaluated. Meta-analysis was planned for biomarkers assessed using the same detection methods and sample type in at least two papers.
Results
Out of 5621 studies identified at initial screening, 28 papers were included in the qualitative analysis of which 2 were eligible for meta-analysis for IgG in serum samples. Eighty-seven biomarkers were assessed with the majority being higher in cases than in controls. Only the meta-analysis of total serum IgG with low heterogeneity value revealed a significant increase in its levels in C/MIPs compared to controls (standardised mean difference: 1.08; 95% CI: 0.76, 1.40).
Conclusion
There is a paucity of data on biomarkers associated with molar-incisor pattern periodontitis. Although serum IgG levels are raised, other more specific biomarkers in saliva, GCF, and blood/serum may be promising but require further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stage III grade C molar-incisor pattern (C/MIP) was formerly known as localised juvenile periodontitis (LJP), and then later as localised aggressive periodontitis (LAgP) [1, 2]. C/MIP is a chronic progressive inflammatory disease of the periodontium characterised by rapid destruction of the soft and hard tissue at an early age resulting in clinical attachment loss and bone resorption leading to tooth loss and functional impairments [3,4,5,6]. It affects the incisors and molars at first; thus, it was identified as a molar-incisor pattern (MIP) in the 2017 classification of periodontal diseases [3,4,5,6,7].
Unlike other periodontal diseases linked to plaque accumulation and poor oral hygiene over time, C/MIP is believed to have a strong genetic predisposition [8]. However, a better understanding of causative factors and specific pathogenic mechanisms still needs to be achieved. Systemically healthy and medically compromised children and young adults with familial aggregation can develop C/MIP at an early age [9, 10]. This condition increases the risk of premature tooth loss that negatively impacts individuals physically, psychologically, and aesthetically [11]. Therefore, early detection and treatment are of great importance [12].
Periodontal diagnosis is a crucial step in the oral examination as it affects the treatment plan and prognosis and influences the quality of life if not detected earlier [13]. Biomarkers in saliva, gingival crevicular fluid (GCF), peripheral blood, and serum might be used as indicators to diagnose periodontal diseases [13,14,15]. A previous systematic review/analysis study has confirmed the diagnostic accuracy of biomarkers in the detection of periodontitis, which may reflect their usefulness in the early detection or assessment of the risk of developing this pathology [16].
Saliva and GCF samples can be collected non-invasively and easily while GCF flow is collected and measured using sterile strips and a Periotron micro-moisture meter [15]. Saliva and GCF have different compositions and harbour host-derived markers [17]. In the presence of inflammation, saliva tends to have a higher concentration of defence factors such as immunoglobulin A (IgA), immunoglobulin G (IgG), and immunoglobulin M (IgM) [18], and the GCF flow increases as a host defence to eliminate the pathogens [19]. Moreover, some promising biomarkers of periodontitis were suggested, such as matrix metalloproteinase-8 (MMP-8), matrix metalloproteinase-9 (MMP-9), interleukin 1 beta (IL1β), and interleukin 6 (IL6) [2, 16, 20].
Peripheral blood and serum samples could also potentially be used as a source of biomarkers [21, 22]. Studies have shown a higher neutrophil–lymphocyte ratio (NLR), a lower lymphocyte-monocyte ratio (LMR) [14], increased levels of proinflammatory cytokines such as interleukin 17 (IL‐17) [21, 23], C-reactive protein (CRP), and fibrinogen in patients with periodontitis compared to healthy controls [24, 25]. Thus, these were considered potential biomarkers that need further affirmation [23].
However, to our knowledge, there are no studies that systematically evaluate biomarkers specifically associated with C/MIP. Discovering specific biomarkers for this condition might help in screening and identifying affected individuals at an early age, and it might help clarify pathogenic mechanisms. Therefore, the present systematic review aimed to explore the existing salivary, GCF, blood, and serum biomarkers used to diagnose C/MIP periodontitis in systemically healthy children and young adults.
Materials and methods
The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with ID no. CRD42022312530. This systematic review and meta-analysis were designed based on the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy and Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). The checklist can be found in the appendix (Appendix 1).
PECOS question
The research question is “In subjects with stage III grade c with molar incisor pattern periodontitis, do the biomarker levels in body fluids differ compared to subjects with healthy periodontium?”.
The population (P), exposure (E), comparison (C), outcome (O), and study design (S) were as follows:
-
P: systemically healthy children and young adults (≤ 25 years of age)
-
E: stage III grade C with molar incisor pattern periodontitis or previous equivalent definitions
-
C: healthy periodontium
-
O: levels of salivary, GCF, peripheral blood, and serum biomarkers
-
S: case–control studies, cross-sectional studies, cohort studies
Eligibility criteria
Studies were included or excluded based on the following criteria.
Inclusion criteria
-
Types of studies: cross-sectional, case–control, and cohort studies with analysis of molecular biomarkers
-
Participants: a minimum of 10 systemically healthy children and young adults aged 25 years and younger in the case group
-
Target condition: according to the 2017 classification of periodontal diseases, the target condition is stage III grade C periodontitis with molar incisor pattern or previous equivalent definitions, including early-onset periodontitis (EOP), aggressive periodontitis (AgP), juvenile periodontitis (JP), and rapidly progressive periodontitis (RPP) in both extents generalised and localised
-
Case reference standard: stage III grade C is clinically defined as clinical attachment loss (CAL) ≥ 5, radiographic bone loss (RBL) extending to the middle third of root and beyond, ≤ 4 tooth loss due to periodontitis, in addition to probing depth (PD) ≥ 6 mm, vertical bone loss ≥ 3 mm, furcation involvement class II or III, and/or moderate ridge defects, progression of CAL or RBL of ≥ 2 mm over 5 years, percentage of bone loss by age is > 1 and tissue destruction exceeding the expectations given biofilm deposits [7]
-
Control condition: healthy periodontium
-
Control reference standard: no clinical evidence of periodontal disease
-
Samples: saliva, GCF, blood, and/or serum
-
Index test: molecular biomarkers identified in the samples of interest
Exclusion criteria
-
Types of studies: cross-sectional, case–control, or cohort studies with genetic or microbiology profiles, randomised clinical trials (RCTs), case reports, reviews, non-clinical, in vitro, animal, and retracted/withdrawn studies were excluded
-
Participants: subjects with systemic conditions, older than 25 years of age or with an unclear age range, recruited less than ten subjects in the case group, pregnant and lactating females, and smokers
-
Definitions: non-C/MIP periodontitis
-
Samples: swabs, gingival tissues, mouthwash, and plaque
Search methods for identification of studies
Search strategy
The following databases were electronically searched from their oldest records until 08 February 2023: Embase (via Ovid), PubMed (MEDLINE), Web of Sciences (WoS), Scopus, and Virtual Health Library. Additionally, peer-reviewed digital dissertations (searched via UMI Proquest) were searched. The search was not restricted to papers in English, and no filters were applied.
The search strings were formulated to include the target condition, index test, type of samples, and population (Appendix 2).
Data collection and analysis
Selection of studies
The papers retrieved from the six databases were de-duplicated following the Bramer et al. method [26]. Two reviewers (authors MA and GNA) independently screened the titles and abstracts of studies to identify articles that potentially meet the inclusion criteria. A pilot screening of 50 studies was done, and the results were compared to ensure consistency between reviewers. The full text of the potentially eligible studies and those abstracts that do not provide sufficient information to allow decision-making regarding inclusion or exclusion were retrieved, and the full texts were screened independently by GNA and MA. Any differences between the two reviewers were settled by consensus after consulting a third review author (LN).
Data extraction and management
Relevant data from the included studies were independently extracted by MA and GNA using a specifically designed extraction Excel form.
The following data were recorded for each study: study characteristics (author(s), year of publication, title, country, study design, setting, funding), demographics in cases and controls (number of periodontal disease cases and non-periodontal disease controls in the beginning and at the end, age, gender, ethnicity, and smoking status), definitions (periodontitis classification in the study, stage III grade C, and health periodontium), types of samples (saliva, GCF, peripheral blood, serum), biomarker detection methods, assessed biomarkers (name, class, biomarker levels—mean and standard deviation—and concentration units).
In longitudinal studies, only baseline data which is the first determination of the levels of biomarkers before treatment were collected and analysed. The mean and standard deviation were calculated if it was not reported. The mean was calculated by dividing the sum of values by the number of values and the standard deviation by multiplying the SE/SEM by the square root of N. In case 2SEM was given, SD was calculated by dividing 2SEM by 2 and then multiplying it by the square root of N.
Assessment of methodological quality
Two tools were used independently by MA and GNA to assess the risk of bias in the included studies: the Newcastle Ottawa Quality Assessment tool (NOS) for case–control and cohort studies and the modified version for cross-sectional studies. Results were compared for consistency, and variations were discussed and agreed on.
Statistical analysis and data synthesis
Meta-analysis was planned for biomarkers assessed using the same detection methods and sample types in at least two papers. The free software environment R (version 4.2.2) was used to analyse and create the meta-analysis (MA) models. Two types of models were run: models with a single standardised mean difference for each paper and models that included 2 or more standardised mean differences from the same paper [27, 28]. In the latter, the raw data from the same paper can be pooled, but to mitigate the risk of a unit-of-analysis error and to avoid “double counting” in the MA, it was necessary to pool the raw data with the dmetar package [29]. The meta package [30] was then used to obtain the random effects models and their p-value, the forest plots, and all statistics related to the between-study heterogeneity (Q-test, I2, H2, Tau2, Tau) of the 34 models obtained (18 non-pooled models and 16 pooled models). The restricted maximum likelihood (“REML”) [31] method was used in all models to calculate TAU2. The Hedges method was used in the MA models to estimate the standardised mean difference, thus avoiding overestimation bias due to the small number of studies included here.
Results
The total number of references retrieved after the removal of duplicates was 5621. Based on the title and abstract screening, 437 articles were eligible for full-text screening. Four hundred and nine articles were excluded for the reasons mentioned in the appendix 3, and 28 studies were included in the current review (Fig. 1). The kappa score and percentage of agreement for the abstract screening were respectively 0.766 and 98.7% and 0.813 and 97.2% for the full-text screening.
Characteristics of included studies
The majority of studies had a case–control design (71.4%), while 14.3% were cohort and 14.3% were cross-sectional studies. Publication years ranged from 1974 to 2022, and most studies were conducted in the USA (n = 15), while others were conducted in Turkey (n = 4), Argentina (n = 2), and one study in each of the following countries: Brazil, Czech Republic, Finland, Germany, Norway, Sweden, UK, and India. The age of included patients ranged from 5 to 25 years old. The study sample size ranged from 10 to 79 in the cases and 5 to 103 in the controls. The definition of periodontal disease was based on clinical examination and/or radiographs to determine the presence/absence of CAL, PD, and RBL. Most of the definitions were based on the presence of bone loss (n = 16), CAL ≥ 2 and PD ≥ 5 (n = 5), CAL ≥ 3 (n = 3), PD ≥ 6 (n = 1), PD ≥ 4 (n = 1), PD ≥ 3 (n = 1), while one did not report a definition but it was included because they referred to C/MIP as “localized juvenile periodontitis” and used clinical indices: plaque index (PI), gingival index (GI), and probing depth (PD) to determine that condition of the periodontium. Definitions of periodontal health were based on not having evidence of bone loss, no bleeding on probing except one study stated that < 10% was accepted, and PD thresholds varied: PD < 4 (n = 2), PD ≤ 3 (n = 3), PD ≤ 2 (n = 3), and some did not specify a measurement (n = 20). Most studies focused on biomarkers in serum (n = 13) and GCF (n = 9), some in saliva (n = 5), and a few in blood (n = 3) and plasma (n = 3). Assays used included ELISA (n = 8), radial immunodiffusion (RID) (n = 5), Luminex multiplex immunoassay (n = 4), fluorometric immunoassay (n = 3), chromogenic immunoassay (n = 2), and the remaining studies used one of the following: checkerboard immunoblotting, electroimmunoassay, electroimmunodiffusion, indirect and direct immunofluorescence, luminol-dependent chemiluminescence immunoassay, lysis inhibition, and gamma spectroscopy, and radioimmunoassay, Table 1.
Data extraction
In the screening phase, some abstracts had missing full text, so the authors were contacted to request the articles and review them against eligibility criteria. Similarly, when extracting the means and standard deviations for each biomarker, some papers presented their results in graphs/plots/charts without giving numerical values, so the dataset was requested from the authors. Not all authors were able to provide the requested datasets. None of the papers reported the sensitivity and specificity of the assessed biomarkers, and only one study gave the contingency tables.
Biomarkers analysed
When grouping the studies by analysed biomarkers, some focused on cytokines such as interleukins IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p40, IL-12p70, and IL-17, interferons: interferon-gamma (IFN-γ) and interferon γ-induced protein 10 kDa (IP-10), chemokines: monocyte chemoattractant protein-1 (MCP-1), eotaxin, macrophage inflammatory protein-1 alfa (MIP-1α), tumour necrosis factor-alfa (TNF-α), granulocyte colony-stimulating factor (G-CSF), and granulocyte–macrophage colony-stimulating factor (GM-CSF), others on tissue degradation markers such as matrix metalloproteinase MMP-1, MMP-2, MMP-3, MMP-8, MMP-9, MMP-12, and MMP-13, while others on serum immunoglobulins such as IgG, IgA, and IgM and immunoglobulins to specific pathogens. Additionally, blood cells, tumour markers, enzymes, proteins, antibodies, and some other molecules were assessed as listed in Table 1.
Characteristics of studies in saliva
The following 10 salivary biomarkers were assessed in 5 case–control studies [32,33,34,35,36] from Turkey, the USA, Argentina, and the UK: β2-microglobulin, lactoferrin, iron, reactive oxygen species (ROS), total radical-trapping antioxidant potential (TRAP), thiobarbituric acid-reactive substances (TBARs), mucin, amylase, protein, and IgA. They were all higher in cases than in controls including the biomarkers without numerical data presented except for lactoferrin and iron. They were assessed in two groups of patients, one with Aggregatibacter actinomycetemcomitans and one without, and were followed over time to observe the development of the disease. Both lactoferrin and iron were lower in Aa-positive LAP subjects than in Aa-negative and positive healthy subjects. A meta-analysis was not possible due to the different salivary biomarkers used in the different studies.
Characteristics of studies in GCF
Nine studies (three cohorts, four case-controls, and two cross-sectional) [27, 37,38,39,40,41,42,43] from the USA, Brazil, and Czech Republic investigated 31 biomarkers: eotaxin, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12P40, IL-12p70, IL-17, IP-10, IFN-γ, MCP1, MIP-α, TNF-α, G-CSF, GM-CSF, receptor activator of NF-kappaB ligand (RANKL), osteoprotegerin (OPG), β-glucuronidase, MMP-1, MMP-2, MMP-3, MMP-8, MMP-9, MMP-12, MMP-13, lysozyme, lactoferrin, IgG, IgA, Ig to Aa. The majority of biomarkers were higher in cases than in controls except for MCP-1, which was higher in controls in 2 studies. Additionally, a few biomarkers such as IFN-γ, IL-4, IL-6, IL-8, IL10, IL-17, and TNF-α were higher in controls in some studies and lower in others (Table 2). Twelve meta-analyses were performed involving the following molecules: GM-CSF, IFN-γ, IL1-β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p40, MCP-1, MIP-1α, and TNF-α. However, because of high heterogeneity (I2 > 75%), the meta-analyses are considered inconclusive (Appendix 4).
Characteristics of studies in whole blood
Three studies (two case–control and one cross-sectional) [44,45,46] from Turkey, Sweden, and Finland found that B-cells, CD3 + cells, CD4 + cells, CD8 + cells, and haemoglobin were all lower in cases than in controls. Lymphocyte counts were higher in cases in one study and lower in another, whereas mean corpuscular volume (MCV), leukocytes (LPK), absolute neutrophil count (ANC), and tyrosine-protein kinase (TPK) were higher in cases than controls. A meta-analysis was not possible due to the different biomarkers in whole blood used in the different studies.
Characteristics of studies in plasma
Three studies (two case–control and one cohort) [27, 47, 48] from the USA and Germany analysed plasma samples for lipopolysaccharides (LPS), ELP-a-PI complex, and ELP content. As reported in Shaddox et al. study, LPS was significantly higher in cases than controls [27], and patients showed a significant reduction in LPS following treatment in Kalash et al. study [47]. ELP-a-PI complex was also statistically significant while ELP content was not [48]. A meta-analysis was not possible due to the different biomarkers in whole blood used in the different studies.
Characteristics of studies in serum
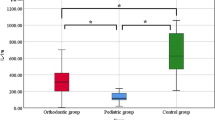
Several biomarkers were assessed in 13 studies (11 case–control and 2 cross-sectional) [28, 34, 36, 44,45,46, 49,50,51,52,53,54,55] from the USA, UK, Sweden, India, Turkey, Norway, and Finland. They are as follows: beta 2-microglobulin, IgG to Aa, IgG to P. gingivalis, IgG to B. fragilis, IgG to P. intermedia, IgG to C. rectus, IgG to E. corrodens, IgG to F. nucleatum, IgG to C. ochracea, IgA to Aa, IgA to P. gingivalis, IgA to B. fragilis, IgA to P. intermedia, IgA to C. rectus, IgA to E. corrodens, IgA to F. nucleatum, IgM to Aa, IgM to P. gingivalis, IgM to B. fragilis, IgM to P. intermedia, IgM to C. rectus, IgM to E. corrodens, IgM to F. nucleatum, IL-1β, C3, C4, IgG, IgA, IgM, IgG1, IgG2, IgG3, IgG4, α2M, protein, IgG/albumin ratio, and alkaline phosphatase ALP. Most investigated biomarkers were higher in cases than controls except for a few biomarkers that were lower in cases than controls as specified in Table 2. Six meta-analyses were performed involving the following molecules: IgG, IgM, IgG to Aa, IgG to P. gingivalis, IgM to Aa, and IgM to P. gingivalis. However, because of high heterogeneity (I2 > 75%), except for IgG, most meta-analyses should be considered inconclusive (Appendix 5). Only the meta-analysis of total serum IgG with low heterogeneity value revealed a significant increase in its levels in C/MIPs compared to controls (standardised mean difference: 1.08; 95% CI: 0.76, 1.40) (Fig. 2).
Risk of bias analysis
All 28 studies were assessed for risk of bias. All cohort studies (4/4) and the majority of the case–control studies (19/20) revealed good quality whereas one case–control study had fair quality, and four cross-sectional studies had a high risk of bias (Appendix 6).
Discussion
This review represents the first attempt to systematically assess biomarkers associated with the very unique phenotype of C/MIP periodontitis. The main findings are that there is a paucity of studies investigating this aspect and not many robust conclusions can be drawn. Although several reports suggest increased or decreased levels of specific inflammatory and tissue degradation markers in GCF, saliva, whole blood, serum, and plasma, meta-analysis was only possible for total IgG levels in serum. This analysis, based on only 2 papers, suggested increased total IgG levels in C/MIP cases compared with controls [50, 52]. Immunoglobulins (Ig) play a major role as part of humoral immunity by stimulating phagocytosis and eliminating microorganisms [56]. IgG is the most prevalent in human serum with periodontitis among the four other classes, IgA, IgM, IgE, and IgD [56], and that was consistent with the results of our meta-analysis and the literature.
Previous literature highlighted the host-microbial interactions and how the imbalance between them is essential for the occurrence of the disease and for determining the extent of the destruction [9, 40, 57]. Following colonisation by gram-negative bacteria including A. actinomycetemcomitans, P. gingivalis, and Tannerella forsythia, and the production of leukotoxins, endotoxins, collagenases, and proteases to cause bone resorption, the host responds by recruiting a significant amount of polymorphonuclear neutrophils (PMNs) including neutrophils, basophils, eosinophils in addition to monocytes, macrophages, and dendritic cells [58]. Particularly in the presence of neutrophils defects, periodontal destruction evolves aggressively resulting in rapid attachment and bone loss [59, 60]. The constant recruitment of host cells causes the oversecretion of several inflammatory mediators, including cytokines, tissue degradation markers, immunoglobulins, tumour markers, enzymes, and proteins [61]. Which can be found in larger quantities in C/MIP patients than in healthy controls, as listed in Table 2. In this context, biomarkers measuring the response to the microbial challenge could be valuable tools to corroborate the clinical findings and potentially have a diagnostic and prognostic added value.
The uniqueness of C/MIP lies in its rapidly-progressive nature and the irreversible periodontal damage caused at an early age and initially localised to the incisors and molars despite the minimal amounts of plaque, calculus, and marginal gingival inflammation [62], which suggests that microbes do not contribute solely to the severity of the disease [63]. The complexity of C/MIP makes it difficult to manage these cases especially since the plaque deposit is not the main etiological factor compared to other forms of periodontitis (formerly known as chronic periodontitis CP) [9]. In other types of periodontitis, maintaining good oral hygiene effectively reduces all the clinical parameters since the absence of bacteria is sufficient to arrest the disease [64]. Undoubtedly, clinical parameters help measure the current condition of the periodontium. However, they do not give a clear picture of the host-microbial interactions and stability or not of disease, especially for the very unique and poorly investigated C/MIP. Therefore molecular biomarkers could be beneficial, providing a diagnostic tool, which is relatively easy and painless to collect if present in saliva or GCF [65].
Treatment and long-term tooth retention may be challenging in C/MIP cases affecting young individuals [9, 40]. A treatment approach consisting of supra- and sub-gingival debridement with adjunctive systemic antibiotics was shown to assist in balancing the host immune responses and disease progression and significantly decrease disease biomarkers [40]. Surprisingly, in some studies, some biomarkers remained higher in cases than in controls even after receiving treatment [66].
Biomarkers have diagnostic and prognostic values as they are beneficial in understanding disease mechanisms and monitoring the host immune response before, during, and after the treatment [67]. Besides the biomarkers of C/MIP mentioned earlier, another set of biomarkers was significantly higher in patients with CP than in controls such as MCP-1, IL-6, MMP-8, macrophage inflammatory protein-1 alpha (MIP-1α), IL-1β, and Hb, and assessment of both salivary IL-6 and MMP-8 was used for early diagnosis [68]. In GCF, prostaglandin E2 (PGE2), aspartate aminotransferase (AST), IL-1β, IL-8, IL-10, neutrophil elastase (NE), osteocalcin and calprotectin, alkaline phosphatase (ALP), macroglobulins (alpha 2, beta 2), MMP-3, MMP-8, MMP-9 [69], MCP-1 [70], and deoxypyridinoline (DPD) have shown promise as biomarkers [71]. To the best of our knowledge, no systematic reviews/meta-analyses were conducted to comprehensively assess different periodontal biomarkers in the blood and serum of systemically healthy individuals. One review evaluated the blood cell count [72], while most existing reviews focused on specific biomarkers. Nonetheless, some potential biomarkers were noticed in the serum of patients with periodontitis, such as resistin [73], C-reactive protein [74], visfatin [75], oncostatin M [76], chemokine CXCL10 [77], and proprotein convertase subtilisin/kexin type 9 (PCSK9) [78]. In the blood, decreased total antioxidant status (TAS) [79] was observed in addition to the increased WBC and neutrophils and reduced erythrocytes and platelets [80]. While previous systematic reviews performed a meta-analysis of the diagnostic “accuracy” of biomarkers, meta-analysis for diagnostic accuracy could not be performed here, as none of the included papers reported the specificity and sensitivity, and only one study gave the diagnostic classification contingency table. Additionally, the paucity of data and high heterogeneity made it impossible to meta-analyse other biomarkers.
The four cohorts [37, 40, 42, 47] and nineteen case–control studies [27, 28, 32,33,34, 36, 38, 41, 43, 44, 46, 48,49,50,51,52,53, 55, 81] had a good quality for meeting NOS criteria in terms of selection, comparability, and exposure/outcome. However, one case control had a fair quality for not providing adequate definitions of stage III grade C and healthy controls [35]. The remaining cross-sectional studies did not have control groups to compare findings [39, 45, 54], failed to calculate and justify the sample size [39, 45, 54, 82], and did not control for confounding factors [39, 45, 54].
This review had several strengths including merging the biomarkers’ data of all the former classifications with the data of the 2017 new classification. The search was not limited to a specific language, as all relevant papers were included and translated if they were in a language other than English. Multiple main databases were searched to ensure that none of the relevant papers was missed unintentionally. Various types of samples were assessed to gain a comprehensive overview of existing biomarkers in the literature. The pre-specified age range was met as the included studies recruited subjects of 5–25 years of age. Although this might be considered a wide age range, it reflects the age range in most published studies. The authors of the papers with graphical representations of their data were contacted multiple times for the raw data. The main limitation of this review was the heterogeneity of the data among six studies that initially had the potential for meta-analysis of 18 biomarkers. Heterogeneity was very high in the 34 meta-analysis models performed, with the exception of the meta-analysis for IgG, so they were considered inconclusive. Another limitation was the lack of recent studies, as most studies (74%) were conducted more than 10 years ago, of which 55% were conducted before 1999. Also, when attempts were made to request raw data/full-text research for some studies, no contacts were found for some old publications and were therefore excluded for missing full-text. The graphs/plots were narratively described if the raw data was not received.
In conclusion, this review highlighted the existing gap in the literature regarding biomarkers of C/MIP and summarised what biomarkers had been investigated in saliva, GCF, blood, plasma, and serum to date. The results emphasise the importance of conducting future observational studies to identify reliable biomarkers that could be useful adjunctive diagnostic tools and/or could accurately predict the likelihood of developing C/MIP before it occurs. This will contribute to prevention/early diagnosis, better treatment outcome, and maintenance of the quality of life. More robust research studies should be conducted in this area, ideally investigating large cohorts of young individuals affected by C/MIP and reporting data on biomarkers that could have clinical utility and could potentially be used for larger meta-analyses.
Data Availability
The data supporting this study’s findings are available on request from the corresponding author.
References
Wara-aswapati N, Howell TH, Needleman HL, Karimbux N (1999) Periodontitis in the child and adolescent. ASDC J Dent Child 66(167–74):154
Zhang L, Henson BS (2000) Camargo PM and Wong DT (2009) The clinical value of salivary biomarkers for periodontal disease. Periodontol 51:25–37. https://doi.org/10.1111/j.1600-0757.2009.00315.x
Velsko IM, Harrison P, Chalmers N, Barb J, Huang H, Aukhil I, Shaddox L (2020) Grade C molar-incisor pattern periodontitis subgingival microbial profile before and after treatment. J Oral Microbiol 12:1814674. https://doi.org/10.1080/20002297.2020.1814674
Shaddox LM, Huang H, Lin T, Hou W, Harrison PL, Aukhil I, Walker CB, Klepac-Ceraj V, Paster BJ (2012) Microbiological characterization in children with aggressive periodontitis. J Dent Res 91:927–933. https://doi.org/10.1177/0022034512456039
Meusel DR, Ramacciato JC, Motta RH, Brito Júnior RB, Flório FM (2015) Impact of the severity of chronic periodontal disease on quality of life. J Oral Sci 57:87–94. https://doi.org/10.2334/josnusd.57.87
Allin N, Cruz-Almeida Y, Velsko I, Vovk A, Hovemcamp N, Harrison P, Huang H, Aukhil I, Wallet SM, Shaddox LM (2016) Inflammatory response influences treatment of localized aggressive periodontitis. J Dent Res 95:635–641. https://doi.org/10.1177/0022034516631973
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MS (2018) Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the classification of periodontal and peri-implant diseases and conditions. J Clin Periodontol 45(Suppl 20):S162-s170. https://doi.org/10.1111/jcpe.12946
Yoshida A, Bouziane A, Erraji S, Lakhdar L, Rhissassi M, Miyazaki H, Ansai T, Iwasaki M, Ennibi O (2021) Etiology of aggressive periodontitis in individuals of African descent. Jpn Dent Sci Rev 57:20–26. https://doi.org/10.1016/j.jdsr.2020.12.001
Albandar JM (2000) (2014) Aggressive periodontitis: case definition and diagnostic criteria. Periodontol 65:13–26. https://doi.org/10.1111/prd.12014
Miller K, Treloar T, Guelmann M, Rody WJ, Jr. and Shaddox LM (2018) Clinical characteristics of localized aggressive periodontitis in primary dentition. J Clin Pediatr Dent 42:95–102. https://doi.org/10.17796/1053-4628-42.2.3
Llanos AH, Silva CGB, Ichimura KT, Rebeis ES, Giudicissi M, Romano MM, Saraiva L (2018) Impact of aggressive periodontitis and chronic periodontitis on oral health-related quality of life. Braz Oral Res 32:e006. https://doi.org/10.1590/1807-3107bor-2018.vol32.0006
Prakasam A, Elavarasu SS, Natarajan RK (2012) Antibiotics in the management of aggressive periodontitis. J Pharm Bioallied Sci 4:S252–S255. https://doi.org/10.4103/0975-7406.100226
Saygun I, Nizam N, Keskiner I, Bal V, Kubar A, Açıkel C, Serdar M, Slots J (2011) Salivary infectious agents and periodontal disease status. J Periodontal Res 46:235–239. https://doi.org/10.1111/j.1600-0765.2010.01335.x
Mishra S, Gazala MP, Rahman W (2022) Clinical and diagnostic significance of blood leukocyte ratios in young patients with stage III grade C periodontitis. Acta Odontol Scand 80:161–168. https://doi.org/10.1080/00016357.2021.1969035
Patil PB, Patil BR (2011) Saliva: a diagnostic biomarker of periodontal diseases. J Indian Soc Periodontol 15:310–317. https://doi.org/10.4103/0972-124x.92560
Arias-Bujanda N, Regueira-Iglesias A, Balsa-Castro C, Nibali L, Donos N, Tomás I (2020) Accuracy of single molecular biomarkers in saliva for the diagnosis of periodontitis: a systematic review and meta-analysis. J Clin Periodontol 47:2–18. https://doi.org/10.1111/jcpe.13202
Fatima T, Khurshid Z, Rehman A, Imran E, Srivastava KC, Shrivastava D (2021) Gingival crevicular fluid (GCF): a diagnostic tool for the detection of periodontal Health and diseases. Molecules 26. https://doi.org/10.3390/molecules26051208
Giannobile WV, Beikler T, Kinney JS, Ramseier CA (2000) Morelli T and Wong DT (2009) Saliva as a diagnostic tool for periodontal disease: current state and future directions. Periodontol 50:52–64. https://doi.org/10.1111/j.1600-0757.2008.00288.x
Subbarao KC, Nattuthurai GS, Sundararajan SK, Sujith I, Joseph J, Syedshah YP (2019) Gingival crevicular fluid: an overview. J Pharm Bioallied Sci 11:S135-s139. https://doi.org/10.4103/jpbs.Jpbs_56_19
de Lima CL, Acevedo AC, Grisi DC, Taba M Jr, Guerra E, De Luca CG (2016) Host-derived salivary biomarkers in diagnosing periodontal disease: systematic review and meta-analysis. J Clin Periodontol 43:492–502. https://doi.org/10.1111/jcpe.12538
Schenkein HA, Koertge TE, Brooks CN, Sabatini R, Purkall DE, Tew JG (2010) IL-17 in sera from patients with aggressive periodontitis. J Dent Res 89:943–947. https://doi.org/10.1177/0022034510369297
Stefaniuk P, Szymczyk A, Podhorecka M (2020) The neutrophil to lymphocyte and lymphocyte to monocyte ratios as new prognostic factors in hematological malignancies - a narrative review. Cancer Manag Res 12:2961–2977. https://doi.org/10.2147/cmar.S245928
Wang H, Luo Z, Lei L, Sun Z, Zhou M, Dan H, Zeng X, Chen Q (2013) Interaction between oral lichen planus and chronic periodontitis with Th17-associated cytokines in serum. Inflammation 36:696–704. https://doi.org/10.1007/s10753-013-9594-2
Andreu R, Santos-Del-Riego S and Payri F (2021) Serum inflammatory and prooxidant marker levels in different periodontal disease stages. Healthcare (Basel) 9. https://doi.org/10.3390/healthcare9081070
Machado V, Botelho J, Escalda C, Hussain SB, Luthra S, Mascarenhas P, Orlandi M, Mendes JJ, D’Aiuto F (2021) Serum C-reactive protein and periodontitis: a systematic review and meta-analysis. Front Immunol 12:706432. https://doi.org/10.3389/fimmu.2021.706432
Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T (2016) De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 104:240–243. https://doi.org/10.3163/1536-5050.104.3.014
Shaddox LM, Wiedey J, Calderon NL, Magnusson I, Bimstein E, Bidwell JA, Zapert EF, Aukhil I, Wallet SM (2011) Local inflammatory markers and systemic endotoxin in aggressive periodontitis. J Dent Res 90:1140–1144. https://doi.org/10.1177/0022034511413928
Albandar JM, DeNardin AM, Adesanya MR, Diehl SR, Winn DM (2001) Associations between serum antibody levels to periodontal pathogens and early-onset periodontitis. J Periodontol 72:1463–1469. https://doi.org/10.1902/jop.2001.72.11.1463
Ebert MHaPCaTFaDD (2019) dmetar: companion R package for the guide ‘doing meta-analysis in R’. http://dmetar.protectlab.org/. Accessed Acces Date
Balduzzi S, Rücker G, Schwarzer G (2019) How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 22:153–160. https://doi.org/10.1136/ebmental-2019-300117
Viechtbauer W (2005) Bias and efficiency of meta-analytic variance estimators in the random-effects model. J Educ Behav Stat 30:261–293. https://doi.org/10.3102/10769986030003261
Acquier AB, De Couto Pita AK, Busch L, Sanchez GA (2017) Parameters of oxidative stress in saliva from patients with aggressive and chronic periodontitis. Redox Rep:Commun Free Radic Res 22:119–126. https://doi.org/10.1080/13510002.2016.1198104
Acquier AB, Pita AKDC, Busch L, Sanchez GA (2015) Comparison of salivary levels of mucin and amylase and their relation with clinical parameters obtained from patients with aggressive and chronic periodontal disease. J Appl Oral Sci: revista FOB 23:288–294. https://doi.org/10.1590/1678-775720140458
Akalin FA, Bulut S, Yavuzyilmaz E (1993) Beta 2-microglobulin levels in serum and saliva of patients with juvenile periodontitis. J Nihon Univ Sch Dent 35:230–234. https://doi.org/10.2334/josnusd1959.35.230
Fine DH, Furgang D, McKiernan M, Rubin M (2013) Can salivary activity predict periodontal breakdown in A. actinomycetemcomitans infected adolescents? Arch Oral Biol 58:611–620. https://doi.org/10.1016/j.archoralbio.2012.10.009
Lehner T, Wilton JM, Ivanyi L, Manson JD (1974) Immunological aspects of juvenile periodontitis (periodontosis). J Periodontal Res 9:261–272
Albandar JM, Kingman A, Lamster IB (1998) Crevicular fluid level of beta-glucuronidase in relation to clinical periodontal parameters and putative periodontal pathogens in early-onset periodontitis. J Clin Periodontol 25:630–639
Alfant B, Shaddox LM, Tobler J, Magnusson I, Aukhil I, Walker C (2008) Matrix metalloproteinase levels in children with aggressive periodontitis. J Periodontol 79:819–826. https://doi.org/10.1902/jop.2008.070513
Bartova J, Krejsa O, Sirova M, Tlaskalova H, Prochazkova J, Duskova J (1995) Local antibodies and cytokine responses in crevicular fluid of patients with juvenile periodontitis. Adv Exp Med Biol 371B:1109–1112
Branco-de-Almeida LS, Cruz-Almeida Y, Gonzalez-Marrero Y, Kudsi R, de Oliveira ICV, Dolia B, Huang H, Aukhil I, Harrison P, Shaddox LM (2021) Treatment of localized aggressive periodontitis alters local host immunoinflammatory profiles: a long-term evaluation. J Clin Periodontol 48:237–248. https://doi.org/10.1111/jcpe.13404
Friedman SA, Mandel ID, Herrera MS (1983) Lysozyme and lactoferrin quantitation in the crevicular fluid. J Periodontol 54:347–350
Goncalves PF, Huang H, McAninley S, Alfant B, Harrison P, Aukhil I, Walker C, Shaddox LM (2013) Periodontal treatment reduces matrix metalloproteinase levels in localized aggressive periodontitis. J Periodontol 84:1801–1808. https://doi.org/10.1902/jop.2013.130002
Monteiro MF, Casati MZ, Sallum EA, Silverio KG, Nociti-Jr FH, Casarin RCV (2022) The familial trend of the local inflammatory response in periodontal disease. Oral Dis 28:202–209. https://doi.org/10.1111/odi.13738
Celenligil H, Ebersole JL (1998) Analysis of serum antibody responses to periodontopathogens in early-onset periodontitis patients from different geographical locations. J Clin Periodontol 25:994–1002
Sandholm L, Saxen L (1983) Concentrations of serum protease inhibitors and immunoglobulins in juvenile periodontitis. J Periodontal Res 18:527–533
Sjodin B, Arnrup K, Matsson L, Wranne L, Carlsson J, Hanstrom L (1995) Periodontal and systemic findings in children with marginal bone loss in the primary dentition. J Clin Periodontol 22:214–224
Kalash D, Vovk A, Huang H, Aukhil I, Wallet SM, Shaddox LM (2015) Influence of periodontal therapy on systemic lipopolysaccharides in children with localized aggressive periodontitis. Pediatr Dent 37:35–40
Zafiropoulos GG, Eldanassouri N, Flores-de-Jacoby L, Havemann K (1987) Determination of the ELP (elastase-like proteinase) plasma levels in patients with rapidly advancing and with juvenile periodontitis. Deutsche zahnarztliche Zeitschrift 42:1056–1060
Albandar JM, DeNardin AM, Adesanya MR, Winn DM, Diehl SR (2002) Associations of serum concentrations of IgG, IgA, IgM and interleukin-1beta with early-onset periodontitis classification and race. J Clin Periodontol 29:421–426
Anil S, Remani P, Ankathil R, Vijayakumar T (1990) Circulating immune complexes in localised juvenile periodontitis. Singapore Dent J 15:17–19
Dibart S, Eftimiadi C, Socransky S, Taubman MA, Van Dyke TE (1998) Rapid evaluation of serum and gingival crevicular fluid immunoglobulin G subclass antibody levels in patients with early-onset periodontitis using checkerboard immunoblotting. Oral Microbiol Immunol 13:166–172
Johnson RJ, Matthews JL, Stone MJ, Hurt WC, Newman JT (1980) Immunopathology of periodontal disease. I. Immunologic profiles in periodontitis and juvenile periodontitis. J Periodontol 51:705–712. https://doi.org/10.1902/jop.1980.51.12.705
Schenck K, Porter SR, Tollefsen T, Johansen JR, Scully C (1989) Serum levels of antibodies against Actinobacillus actinomycetemcomitans in various forms of human periodontitis. Acta Odontol Scand 47:271–277
Spindler SJ, Thompson JJ, Yukna RA, Costales AD (1986) Juvenile periodontitis. I. Demonstration of local immunoglobulin synthesis. J Periodontol 57:300–304
Unsal BT, Ozcan G, Balos K, Mevsim G (1996) Serum antibodies to Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis in juvenile periodontitis and adult periodontitis (part I). J Marmara Univ Dent Fac 2:470–473
Kulshrestha D, Siddeshappa S, Biswas J (2013) Role of immunoglobulin G and A in periodontitis: a review. Jof Pure Appl Microbiol 70:673–676
Nibali L (2015) Aggressive periodontitis: microbes and host response, who to blame? Virulence 6:223–228. https://doi.org/10.4161/21505594.2014.986407
Kantarci A, Oyaizu K, Van Dyke TE (2003) Neutrophil-mediated tissue injury in periodontal disease pathogenesis: findings from localized aggressive periodontitis. J Periodontol 74:66–75. https://doi.org/10.1902/jop.2003.74.1.66
Bhansali RS, Yeltiwar RK, Bhat K (2017) Evaluation of peripheral neutrophil functions in aggressive periodontitis patients and their family members in Indian population: an assessment of neutrophil chemotaxis, phagocytosis, and microbicidal activity. J Indian Soc Periodontol 21:449–455. https://doi.org/10.4103/jisp.jisp_107_17
Meng H, Xu L, Li Q (2000) Han J and Zhao Y (2007) Determinants of host susceptibility in aggressive periodontitis. Periodontol 43:133–159. https://doi.org/10.1111/j.1600-0757.2006.00204.x
Kornman KS (2008) Mapping the pathogenesis of periodontitis: a new look. J Periodontol 79:1560–1568. https://doi.org/10.1902/jop.2008.080213
Niklaus Lang PMB, Cullinan M, Jeffcoat M, Mombelli A, Murakami S, Page R, Papapanou P, Tonetti M, Van Dyke T (1999) Consensus report: aggressive periodontitis. Ann Periodontol 4:53
Mani A, James R, Mani S (2018) Etiology and pathogenesis of aggressive periodontitis: a mini review. Galore Int J Health Sci Res 3(2):4–8
Lertpimonchai A, Rattanasiri S, Arj-Ong Vallibhakara S, Attia J, Thakkinstian A (2017) The association between oral hygiene and periodontitis: a systematic review and meta-analysis. Int Dent J 67:332–343. https://doi.org/10.1111/idj.12317
Ji S, Choi Y (2015) Point-of-care diagnosis of periodontitis using saliva: technically feasible but still a challenge. Front Cell Infect Microbiol 5:65. https://doi.org/10.3389/fcimb.2015.00065
Trombelli L, Scapoli C, Tatakis DN, Minenna L (2006) Modulation of clinical expression of plaque-induced gingivitis: response in aggressive periodontitis subjects. J Clin Periodontol 33:79–85. https://doi.org/10.1111/j.1600-051X.2005.00873.x
Bhuyan R, Bhuyan SK, Mohanty JN, Das S, Juliana N and Juliana IF (2022) Periodontitis and its inflammatory changes linked to various systemic diseases: a review of its underlying mechanisms. Biomedicines 10. https://doi.org/10.3390/biomedicines10102659
Cafiero C, Spagnuolo G, Marenzi G, Martuscelli R, Colamaio M and Leuci S (2021) Predictive periodontitis: the most promising salivary biomarkers for early diagnosis of periodontitis. J Clin Med 10. https://doi.org/10.3390/jcm10071488
Gupta S, Chhina S, Arora SA (2018) A systematic review of biomarkers of gingival crevicular fluid: their predictive role in diagnosis of periodontal disease status. J Oral Biol Craniofac Res 8:98–104. https://doi.org/10.1016/j.jobcr.2018.02.002
Gupta M, Chaturvedi R, Jain A (2013) Role of monocyte chemoattractant protein-1 (MCP-1) as an immune-diagnostic biomarker in the pathogenesis of chronic periodontal disease. Cytokine 61:892–897. https://doi.org/10.1016/j.cyto.2012.12.012
Syed S, Kankara VR, Pathakota KR, Krishnan P, Mishra A (2020) Evaluation of deoxypyridinoline levels in gingival crevicular fluid and serum as alveolar bone loss biomarker in patients with periodontitis. J Indian Soc Periodontol 24:322–328. https://doi.org/10.4103/jisp.jisp_256_19
Almășan O, Leucuța DC and Hedeșiu M (2022) Blood cell count inflammatory markers as prognostic indicators of periodontitis: a systematic review and meta-analysis. J Pers Med 12. https://doi.org/10.3390/jpm12060992
Akram Z, Rahim ZH, Taiyeb-Ali TB, Shahdan MS, Baharuddin NA, Vaithilingam RD, Safii SH (2017) Resistin as potential biomarker for chronic periodontitis: a systematic review and meta-analysis. Arch Oral Biol 73:311–320. https://doi.org/10.1016/j.archoralbio.2016.08.016
Pradeep AR, Manjunath RG, Kathariya R (2010) Progressive periodontal disease has a simultaneous incremental elevation of gingival crevicular fluid and serum CRP levels. J Investig Clin Dent 1:133–138. https://doi.org/10.1111/j.2041-1626.2010.00022.x
Türer ÇC, Balli U, Güven B, Çetinkaya B, Keleş G (2016) Visfatin levels in gingival crevicular fluid and serum before and after non-surgical treatment for periodontal diseases. J Oral Sci 58:491–499. https://doi.org/10.2334/josnusd.16-0116
Thorat M, Pradeep AR, Garg G (2010) Correlation of levels of oncostatin M cytokine in crevicular fluid and serum in periodontal disease. Int J Oral Sci 2:198–207. https://doi.org/10.4248/ijos10077
Aldahlawi S, Youssef AR, Shahabuddin S (2018) Evaluation of chemokine CXCL10 in human gingival crevicular fluid, saliva, and serum as periodontitis biomarker. J Inflamm Res 11:389–396. https://doi.org/10.2147/jir.S177188
Tabeta K, Hosojima M, Nakajima M, Miyauchi S, Miyazawa H, Takahashi N, Matsuda Y, Sugita N, Komatsu Y, Sato K, Ishikawa T, Akiishi K, Yamazaki K, Kato K, Saito A, Yoshie H (2018) Increased serum PCSK9, a potential biomarker to screen for periodontitis, and decreased total bilirubin associated with probing depth in a Japanese community survey. J Periodontal Res 53:446–456. https://doi.org/10.1111/jre.12533
Konopka T, Król K, Kopeć W, Gerber H (2007) Total antioxidant status and 8-hydroxy-2’-deoxyguanosine levels in gingival and peripheral blood of periodontitis patients. Arch Immunol Ther Exp (Warsz) 55:417–422. https://doi.org/10.1007/s00005-007-0047-1
Botelho J, Machado V, Hussain SB, Zehra SA, Proença L, Orlandi M, Mendes JJ, D’Aiuto F (2021) Periodontitis and circulating blood cell profiles: a systematic review and meta-analysis. Exp Hematol 93:1–13. https://doi.org/10.1016/j.exphem.2020.10.001
Celenligil H, Kansu E, Eratalay K (1990) Juvenile and rapidly progressive periodontitis. Peripheral blood lymphocyte subpopulations. J Clin Periodontol 17:207–210
Tavakoli TT, Gholami F, Huang H, Gonçalves PF, Villasante-Tezanos A, Aukhil I, de Oliveira RCG, Hovencamp N, Wallet S, Ioannidou E, Shaddox LM (2022) Gender differences in immunological response of African-American juveniles with grade C molar incisor pattern periodontitis. J Periodontol 93:392–402. https://doi.org/10.1002/jper.21-0143
Author information
Authors and Affiliations
Contributions
L. Nibali conceived the study. All authors contributed to the study design, added to the manuscript and critically reviewed it, the tables, and the appendices, and commented on previous versions of the manuscript. Searching for relevant data, screening retrieved articles, extracting data, and assessing the risk of bias were done by M. Alamri and G. N. Antonoglou. Drafting the manuscript and creating tables and appendices were done by M. Alamri. L. Nibali and M. Alamri made data requests for studies with a graphical data representation. C. Balsa-Castro performed programming in R for meta-analysis and graphs, and I. Tomás performed the selection of the meta-analysis method and interpretation of meta-analytical results. Finally, all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with ID no. CRD42022312530.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alamri, M.M., Antonoglou, G.N., Proctor, G. et al. Biomarkers for diagnosis of stage III, grade C with molar incisor pattern periodontitis in children and young adults: a systematic review and meta-analysis. Clin Oral Invest 27, 4929–4955 (2023). https://doi.org/10.1007/s00784-023-05169-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05169-x