Abstract
Aim
The current randomized controlled clinical trial assessed the effect of injectable platelet-rich fibrin (I-PRF) combined with demineralized freeze-dried bone allograft (DFDBA) compared to DFDBA alone in the management of intrabony defects of stage-III periodontitis patients.
Methodology
Following sample size calculation, twenty stage-III periodontitis patients with ≥ 5 mm clinical attachment level (CAL)-loss and ≥ 3 mm intrabony defects were randomized into test (I-PRF + DFDBA; n = 10) and control (DFDBA; n = 10) groups. CAL (primary outcome), periodontal probing depth (PPD), gingival recession depth (GRD), full-mouth plaque scores (FMPS), full-mouth bleeding scores (FMBS), radiographic linear defect depth (RLDD), and bone fill (secondary outcomes) were examined at baseline, 3, 6, and 9 months post-surgically.
Results
I-PRF + DFDBA and DFDBA independently demonstrated significant intragroup CAL-gain, PPD-, and RLDD-reduction at 3, 6, and 9 months (p < 0.05), with no significant intergroup differences observed (p > 0.05). CAL-gain (mean ± SD) of 2.40 ± 0.70 mm and 2.50 ± 0.85 mm and PPD-reduction of 3.50 ± 1.18 mm and 2.80 ± 0.42 mm were demonstrated for I-PRF + DFDBA and DFDBA at 9 months respectively. Both groups showed significant intragroup RLDD improvement, with a RLDD of 3.58 ± 0.66 mm and 3.89 ± 1.57 mm for I-PRF + DFDBA and DFDBA at 9 months respectively. Stepwise linear regression analysis revealed that baseline RLDD and bone fill at 9 months were significant predictors of CAL (p < 0.05).
Conclusion
Within the present study’s limitations, DFDBA with or without I-PRF resulted in significant improvement in clinical and radiographic periodontal parameters in the surgical treatment of periodontal intrabony defects of stage-III periodontitis patients. Addition of I-PRF to DFDBA does not appear to significantly enhance the DFDBA’s reparative/regenerative outcomes.
Clinical relevance
Within the current study’s limitations, routinely adding I-PRF to DFDBA cannot be recommended to significantly improve DFDBA’s treatment outcomes in intrabony defects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontitis is a chronic inflammatory disorder, associated with dysbiotic plaque biofilms, resulting untreated in progressive destruction of the tooth-supporting apparatus and intrabony periodontal defects [1]. Such defects present risk factors for further disease progression, and their therapy improves teeth prognosis [2]. In this context, a number of periodontal approaches were advocated, employing barrier membranes, enamel matrix derivatives, bone grafts, or growth factor concentrates [3].
The osteoinductive demineralized freeze-dried bone allograft (DFDBA) harbors a variety of growth/differentiation factors, notably bone morphogenetic proteins (BMPs) 2, 4, and 7, and is inferred to promote periodontal repair/regeneration, with significant PPD-reduction, CAL-gain, and bone fill [4]. Injectable platelet-rich fibrin (I-PRF), a liquid autologous platelet concentrate introduced based on the “low-speed centrifugation concept” [5, 6], further harbors a variety of growth/differentiation factors (GFs), with reported positive attributes on angiogenesis, inflammation, and periodontal wound healing [6,7,8]. Recently, it was proposed that mixing I-PRF with bone grafts, forming a gelatinous fibrin-graft-amalgamate rich in growth/differentiation factors (sticky bone), enhanced the graft’s biological properties, handling, and stability [9]. Through the I-PRF-contained growth/differentiation factors in addition to its fibrin meshwork, “sticky bone” was proposed to endorse periodontal healing processes, enhancing periodontal cell adhesion, osteoprogenitor cell selection, osteoblastic cell viability, attachment, proliferation, and differentiation [9, 10] as well as bone regeneration, while decreasing epithelial soft tissue ingrowth into periodontal intrabony defects [11, 12]. In addition to its enhanced handling characteristics, the clinically improved adaptation and stabilization properties of “sticky bone” are believed to prevent micro- and macro-mobility of the graft introduced into the periodontal defects, with enhanced wound healing and regeneration attributes [13].
Still, limited data is available on the clinical potential of I-PRF in combination with DFDBA in treating intrabony defects. The present randomized controlled trial assessed for the first time the clinical and radiographic outcomes of I-PRF combined with DFDBA in the management of periodontal intrabony defects in patients with stage-III periodontitis. Clinical attachment level (CAL; primary outcome), periodontal probing depth (PPD), gingival recession depth (GRD), full-mouth plaque scores (FMPS), full-mouth bleeding scores (FMBS), radiographic linear defect depth (RLDD), and bone fill (secondary outcomes) were assessed at baseline, 3, 6, and 9 months post-surgically.
Materials and methods
Study registration and design
The current study was conducted in compliance with Helsinki Declaration for medical research involving human subjects as revised in 2013 as double-blind, parallel arms, and randomized controlled clinical trial, with 1:1 allocation ratio, to assess clinical and radiographic outcomes of I-PRF combined with DFDBA (I-PRF + DFDBA; test-group) versus DFDBA alone (DFDBA; control group) in surgical treatment of intrabony defects of stage-III periodontitis patients. The trial protocol was registered on www.clinicaltrials.gov on the 31st of March 2019 (NCT03900013), and the informed consents were approved by the Ethics Committee, Faculty of Dentistry, Cairo University on April 2019 (IRB:19|4|1).
Population
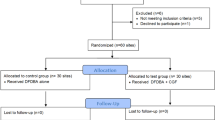
Recruitment, operation, and follow-up of all participants were carried between June 2019 and July 2021 at the Department of Oral Medicine and Periodontology, Faculty of Dentistry, Cairo University, Egypt. Participants were enrolled through screening of patients at the Department of Periodontology, Cairo University, Egypt, personal referrals, and poster announcements. A total of 83 participants were assessed for eligibility, 63 are excluded for not meeting the inclusion criteria, and 20 participants (20 defects) were included (Fig. 1). All participants (age ≥ 18 years) were diagnosed with stage-III periodontitis, full-mouth plaque score (FMPS) and full-mouth bleeding scores (FMBS) ≤ 20% [14], PPD ≥ 6 mm, and CAL ≥ 5 mm, which persisted 6–8 weeks following non-surgical periodontal therapy [15], with ≥ 3 mm two- or three-walled intrabony defects detected radiographically. Patients with systemic conditions contradicting surgical intervention or affecting periodontal healing, including smokers [16, 17], diabetic patients [18], pregnant or lactating females [19], and patients with tooth mobility, furcation involvement, or active orthodontic therapy [20], were excluded.
Sample size
Sample size calculation was conducted using a mean CAL difference of 1.1 mm, as the minimal clinically acceptable CAL difference, and a standard deviation of 0.74 mm [21]. Using a power of β = 80% and type I error α = 5% and based on two-tailed t-test, 8 defects were deemed necessary, which were increased to 10 defects per group to account for dropouts. Sample size calculation was performed, using G-Power software version 3.1 (Heinrich-Heine-Universität, Düsseldorf, Germany).
Randomization and blinding
Participants were randomly assigned to either I-PRF + DFDBA- or DFDBA-group. Sequence generation was carried out using www.randomizer.org. Allocation was concealed in sequentially numbered opaque-sealed envelopes (MH). All participants were equally prepared for the surgical procedure by a single investigator (MA). Following open flap debridement (OFD), the study coordinator (KFE) assigned the participants to either I-PRF + DFDBA or DFDBA-group. Due to the type of interventions, the operator and participants could not be blinded. The outcome assessor and the biostatistician were blinded.
Outcomes
CAL (primary outcome) was measured as the distance from the cemento-enamel junction (CEJ) to the base of periodontal pocket. PPD was determined as the distance from the base of pocket to the gingival margin. GRD was measured as the level from the gingival margin to the CEJ, while FMPS [22] and FMBS [23] were measured as previously described (all secondary outcomes). On the day of surgery, all baseline parameters were recorded. CAL, PPD, and GRD were measured at baseline, 3, 6, and 9 months post-operatively in mm, using UNC-15 periodontal probes and prefabricated customized acrylic stents with interproximal grooves to harbor the periodontal probe, for standardization and reproducibility of clinical measurements [24, 25]. FMPS and FMBS were measured at baseline and 9 months post-operatively. Changes in the recorded parameters were calculated through subtraction of 3, 6, and 9 months from baseline values, and percentage changes were determined through dividing values of changes by baseline values.
Individually customized bite blocks fabricated for each patient and parallel-angle technique were employed (Zhermack Zetaplus C-Silicone kit, Badia Polesine, Italy) using (XCP®) X-ray film holding system (Dentsply Sirona, Charlotte, USA). Periapical radiograph PSP sensor size two (Xios AE, Dentsply Sirona, New York, USA) and standardized exposure setting of 60 kVp, 8 mA, 0.7 mm, and 0.10 s (Heliodent Plus, Dentsply Sirona, PA, USA) were used. The defect angle was measured at baseline, as the angle formed between intersections of AC-DB and tooth long axis lines. RLDD was measured as the depth of the intrabony defect from the alveolar crest (AC) to the defect base (DB) as previously reported [26, 27] at baseline, 6 and 9 months postoperatively (Fig. 2). Calculation of bone fill in mm was done by a subtraction of follow-up from baseline RLDD values, and percentages of bone fill were expressed as the proportion of change to baseline RLDD [28].
Intrabony defect radiographic measurements. a Reference point identification: cemento-enamel junction (CEJ), alveolar crest (AC), and defect base (DB). b Reference line identification (in red): vertical line corresponding to long axis and horizontal perpendicular line passing through AC and identifying radiographic linear defect depth (RLDD) in blue. c Radiographic angle connecting CEJ, DB, and AC
Calibration
Two blinded experienced investigators (WA and MN) obtained all parameters. Prior to study conduction, calibration was performed through comparing two measurements by the two investigators on the same participants (not included in the study) twice, one week apart, retrieving an intraexaminer agreement score > 0.85 for clinical outcomes and > 0.82 score for radiographic measurements.
Interventions
Pre-operatively
Participants were provided with information about the intervention and asked to sign an informed consent. Phase I periodontal therapy was conducted through supra- and subgingival debridement, followed by instructions on oral hygiene performance, using toothbrushes and a twice daily use of 0.12% chlorhexidine HCL mouthwash for two weeks (Hexitol, ADCO Pharma Co, Cairo, Egypt) [15]. After 6–8 weeks, reevaluation was performed to confirm the necessity for surgical intervention through persistence of interproximal defects with PPD ≥ 6 mm, CAL ≥ 5 mm, and vertical intrabony defects ≥ 3 mm on periapical radiographs [29].
Surgery
All surgical procedures were conducted by a single operator (MA). Following administration of local anesthesia (2% mepivacaine HCl with 1:20,000 levonordefrin, Alexandria Co. for Pharmaceuticals, Alexandria, Egypt), intrasulcular incisions were performed buccally and lingually/palatally on the affected tooth and extended one adjacent tooth mesially and distally, using 15c blades (TRINON Titanium GmbH, Augartenstraße, Karlsruhe, Germany). Following mucoperiosteal flaps’ elevation, thorough debridement was performed using ultrasonic scalers (Woodpecker Ultrasonic UDS-K Scaler, Zhengzhou, China) and mini-/after-five Gracey curettes (Hu-Friedy, Chicago, USA), until defects were clear from any granulation tissue [30], and the defect morphology was visually explored and recorded.
In the control group, DFDBA graft material (AlloOss®; demineralized cortical particulates, ACE Surgical Supply Co., Brockton, MA, USA) was placed into the intrabony defect without overfilling. In the test group, 10 mm of fresh blood was withdrawn by venipuncture of the antecubital vein into a sterile 10 ml glass vacuum tube (Voma Med, Chongqing, China) without anticoagulant, and the tube immediately centrifuged (Digital Tabletop Centrifuge, rotor angle: 45° and a maximum radius of 10.6 cm, Velab, VE-4000, TX, USA) at a maximum relative centrifugal force (RCF-max) of 60 g (700 rpm) for 3 min at room temperature [31]. One milliliter of liquid I-PRF was collected using a sterile syringe [32, 33] and amalgamated with DFDBA at a proportion of 1:1 [21], till the I-PRF encapsulated the bone particles, before putting it into the intrabony defect. Finally, the flap was passively repositioned using interrupted 4–0 silk suture (ASSUT Medical, Pully-Lausanne, Switzerland; Fig. 3).
Clinical steps in representative cases of the control (a–d) and test (e–j) groups. Control group using DFDBA alone and test group using I-PRF/DFDBA. Control group: a 7 mm probing pocket depth using a prefabricated stent at baseline, b intrabony defect with vertical component of 4 mm at the mesial site of lower left first molar, c application of DFDBA in the defect, and d 3 mm proping pocket depth 9 months post-operatively. Test group: e 6 mm probing pocket depth at the mesial site of lower left first molar, f intrabony defect with vertical component of mm, g injectable-PRF, h combination of I-PRF with DFDBA, i application of combined I-PRF/DFDBA in the defect, and j 2 mm proping pocket depth 9 months post-operatively
Post-operatively
One gram Augmentin (875 mg amoxicillin + 125 mg clavulanate potassium, GlaxosmithKline, Worthing, England) twice per day for 7 days and Ibuprofen 600 mg, three times daily for 3 days (Kahira Pharm Co., Cairo, Egypt) [34], were prescribed. Participants were instructed to avoid tooth brushing and flossing in the surgical area for two weeks and to rinse with 0.12% chlorhexidine HCL (Hexitol, ADCO Pharma) twice per day for 1 min [35]. Sutures were removed 14 days after the surgical procedure [34], and participants were advised to continue mechanical biofilm removal, using an ultra-soft toothbrush. Recalling of participants was done weekly during the first month then at 3, 6, and 9-months [36].
Statistical analysis
Non-numerical descriptive data were presented as number (n) and percentage (%), using Chi-square test. Numerical data was reported as mean ± standard deviation or median with interquartile range. Kolmogorov–Smirnov test and Shapiro–Wilk test were used to explore the normality of data. For normally distributed data, independent t-test was used for intergroup comparison, while repeated measures ANOVA/Bonferroni post hoc correction (3 or more intervals) was employed for intragroup comparison between different time points. For non-normally distributed data, Mann-Whiney U test was used for intergroup comparison whilst Friedman test and post hoc Wilcoxon signed-rank test were used for intragroup comparison. A stepwise linear regression model used CAL after 9 months as the dependent variable, with study group, gender, age, number of defect walls, FMBS at baseline and 9 months, FMPS at baseline and 9 months, RLDD and radiographic defect angle at baseline, and bone fill at 9 months as independent variables. All tests were two-tailed, and p < 0.05 was statistically significant (SPSS for Windows, version 26, IBM, New York, USA).
Results
Baseline characteristics
This randomized, parallel-group clinical trial included a total of 20 intrabony defects in twenty participants (7 males and 13 females) with stage-III periodontitis. The periodontal intrabony defects were randomly assigned either into I-PRF + DFDBA-group (n = 10, test-group) or DFDBA-group (n = 10, control-group), with no drop-outs. The test group included 3 males and 7 females (mean age of 31.30 ± 4.79 years), while control group included 4 males and 6 females (mean age of 33.90 ± 6.44 years). Healing in all patients was uneventful. Regarding tooth distribution, the I-PRF + DFDBA-group involved three anteriors, two premolars, and five molars, while the DFDBA-group had four, one, and five teeth respectively (baseline characteristics in Table 1). Concerning defects’ morphology, the I-PRF + DFDBA-group comprised of 30% combined one–two walls, 20% combined two–three walls, 40% two-wall, and 10% three-wall defects, while the DFDBA-group included 20% combined one–two walls, 30% combined two–three walls, 30% two-wall, and 20% three-wall defects. The radiographic defect angle in the I-PRF + DFDBA-group was 35.62 ± 8.58° while 40.41 ± 8.24° in the DFDBA-group at baseline (p ≥ 0.05, Table 1).
Clinical outcomes
Compared to baseline values, the I-PRF + DFDBA-group demonstrated significant CAL-gain of 2.20 ± 0.63 mm (38.48 ± 10.80%), 2.50 ± 0.53 mm (43.24 ± 6.67%), and 2.40 ± 0.70 mm (41.81 ± 11.31%, p < 0.05), while the DFDBA-group showed significant CAL-gain of 2.50 ± 1.08 mm (38.12 ± 7.92%), 2.70 ± 1.16 mm (41.55 ± 11.84%), and 2.50 ± 0.85 mm (40.77 ± 15.54%, p < 0.05) at 3, 6, and 9 months respectively, with insignificant intergroup differences (p ≥ 0.05, Table 2). Similarly, compared to baseline, a significant PPD-reduction was notable in the I-PRF + DFDBA-group of 2.50 ± 0.97 mm (36.23 ± 10.70%), 2.90 ± 0.74 mm (43.23 ± 8.74%), and 3.50 ± 1.18 mm (51.26 ± 11.50%, p < 0.05) and in the DFDBA-group of 2.40 ± 1.07 mm (35.98 ± 10.27%), 2.70 ± 0.67 mm (41.54 ± 7.69%), and 2.80 ± 0.42 mm (44.10 ± 9.82%, p < 0.05) at 3, 6, and 9 months respectively, with insignificant intergroup differences (p ≥ 0.05, Table 2). Compared to baseline, a significant change in GRD values of -0.80 ± 0.63 mm, − 0.50 ± 0.97 mm, and 0.10 ± 1.20 mm was evident in the I-PRF + DFDBA-group at 3, 6, and 9 months respectively (p < 0.05). In the DFDBA-group, GRD changes were − 1.40 ± 1.35 mm, − 1.20 ± 1.23 mm, and − 1.10 ± 1.45 mm at 3, 6, and 9 months respectively, with insignificant intergroup differences (p ≥ 0.05, Table 2). In the I-PRF + DFDBA-group, FMPS was 17.30 ± 2.21% and 12.90 ± 2.08% versus 17.70 ± 2.21% and 13.50 ± 1.58% in the DFDBA-group at baseline and 9 months respectively, with insignificant intergroup differences (p ≥ 0.05, Table 2). For FMBS, the I-PRF + DFDBA-group showed significant improvement from 18.30 ± 1.37% to 13.60 ± 2.12%, versus the DFDBA-group, which demonstrated 18.50 ± 1.27% and 14.10 ± 2.13% at baseline and 9 months respectively (p < 0.05), with insignificant intergroup differences (p ≥ 0.05, Table 2).
Radiographic outcomes
In the I-PRF + DFDBA-group, RLDD was 6.21 ± 1.22 mm at baseline and significantly decreased to 4.43 ± 0.80 mm at 6 months and 3.58 ± 0.66 mm at 9 months (p < 0.05). In the DFDBA-group, RLDD was further significantly decreased from 6.61 ± 2.07 mm at baseline, to 4.88 ± 1.46 mm and 3.89 ± 1.57 mm at 6 and 9 months respectively (p < 0.05), with insignificant intergroup differences (p ≥ 0.05, Table 3). The I-PRF + DFDBA-group showed radiographic bone fill of 1.78 ± 0.96 mm (27.83 ± 12.67%) after 6 months and 2.63 ± 0.95 mm (41.64 ± 10.43%) after 9 months (p < 0.05). Similarly, in the DFDBA-group, a significant radiographic bone fill of 1.73 ± 0.97 mm (25.52 ± 9.42%) and 2.72 ± 1.00 mm (41.35 ± 10.64%) was evident after 6 and 9 months respectively, with insignificant intergroup differences (p ≥ 0.05, Table 3).
Stepwise linear regression analysis
A significant direct relationship between CAL at 9 months and RLDD at baseline and a significant inverse relationship between CAL and bone fill and at nine months were evident (p < 0.05, Table 4).
Discussion
The persistence of intrabony defects, following non-surgical periodontal therapy, represents a risk factor for further disease progression [29]. Thus, a primary aim of individualized periodontal therapy remains to be a resolution of such defects with possible reinstitution of the lost tooth-investing and supporting structures [2, 37]. In recent years, autologous platelet concentrates were introduced as promising biological agents in the management of various periodontal defects with remarkable clinical results [38, 39], with PRF alone or in combination with bone replacement grafts reported to induce significant PPD-reduction and CAL-gain [40]. These results were primarily attributed to the PRF’s ability to enhance the periodontal wound healing events, providing three-dimensional fibrin scaffolds for cellular migration, adhesion, and differentiation, through its enclosed leukocytes and platelets, in addition to its continuous delivery of a multitude of crucial growth/differentiation factors into the wound site [41,42,43]. Additionally, the low-speed centrifugation concept, introduced to promote a higher and more uniform distribution of platelets and leukocytes within the PRF, resulted in enhanced PRF formulations, including the liquid I-PRF. Compared to conventional PRF, I-PRF was reported to demonstrate higher concentrations of growth/differentiation factors [31] and a more sustained release of these factors over a period of ten days [5, 6]. To our knowledge, the current randomized clinical trial is the first to explore the adjunctive effect of combining I-PRF with DFDBA in the surgical treatment of intrabony periodontal defects.
The amalgamation of platelet concentrates with bone grafts, in addition to enhancing the grafts’ clinical handling properties, would entrap platelets and neutrophils and release essential growth/differentiation factors in the healing periodontal site [44, 45]. Indeed, similar to earlier investigations combining PRP [46] and PRF [47] with DFDBA, or PRF with demineralized bovine bone matrix (DBBM) [48] in the management of intrabony defects, in the current study, I-PRF + DFDBA as well as DFDBA alone exhibited significant CAL-gain, PPD-reduction, and radiographic bone fill, with no significant differences observed between them. Similarly, the addition of a PRF membrane to bioactive glass did not enhance periodontal clinical parameters in terms of PPD-reduction and CAL-gain compared to bioactive glass alone after 9 months, although more significant bone fill was evident in the intrabony defects receiving the combined treatment after 6 and 9 months [49]. Yet, PRF used in the form of membranes with DFDBA [21] or bioactive glass [50] demonstrated significantly enhanced CAL-gain, PPD-reduction, and bone fill compared with DFDBA or bioactive glass alone, allowing for the plausible assumption that, in contrast to the above-mentioned results, the growth/differentiation factors laden PRF membranes could have provide a short-term compartmentalization effect that could augment their periodontal reparative/regenerative effects. Comparable to previous studies, demonstrating a favorable effect of PRF on soft tissue healing attributes [48, 50, 51], in the present study, I-PRF + DFDBA-group exhibited an enhanced yet non-significant, reduction in gingival recession parameters, underlying the earlier reported favorable effects of the fibrin content of I-PRF, exerting cellular adhesive and migration promoting functions, stabilizing the surgical flap, enriching the area with a multitude of essential growth/differentiation factors, and thereby enhancing angiogenesis, epithelialization, and soft tissue wound healing [52].
Although it was demonstrated that platelet concentrates resulting from the low-speed centrifugation concept release a higher amount of growth/differentiation over time [53], compared to A-PRF, the total number of leukocytes, platelets, and growth/differentiation factors could have been significantly lower in the obtained I-PRF, owing to its lesser volume [6]. This could explain the observed absence of a significant synergistic effect of I-PRF/DFDBA amalgamation on the examined periodontal parameters. A further explanation for the absence of an additional effect, similar to earlier results on the combination of EMD with DFDBA in the treatment of intrabony defects [4], could be that the biological effects of I-PRF have been masked in the amalgamate by the outstanding osteoconductive properties of the DFDBA, harboring itself an array of growth/differentiation factors in higher amounts (BMP-2, -4, and -7; TGF-b1, VEGF, FGF-a, and IGF-I) pivotal for various early and especially late stages of periodontal wound healing [54,55,56]. Finally, the regression model did not show associations between age, gender, number of defect walls, radiographic angle, FMPS, and FMBS at baseline or follow-ups with CAL at 9 months. However, a significant direct association between RLDD at baseline and CAL was evident. Moreover, a significant inverse relationship between bone fill gain and CAL at nine months was evident, as bone gain measured radiographically is translated into a reduced attachment loss clinically.
Still, the current trial’s results should be interpreted in context of its limitations. First, the inclusion of intrabony defects with different morphologies, although randomly distributed could have affected the observed effects. A subgrouping according to the defects’ morphology, although being more informative, would have led to substantial decrease in the trial’s power. Second, the preparation of I-PRF necessitates collection of patient’s own blood. Consequently, patients who are afraid of blood sampling repelled to participate in the current trail. Third, the present study did not use the newly developed horizontal centrifugation protocol [6], which could have elevated the number of platelets and leucocytes in the I-PRF, with a more even platelet distribution. Fourth, although minimally invasive surgical techniques are currently recommended in regenerative therapeutic approaches of intrabony defects [57], these procedures were not applied in the current study due to the presence of deep intrabony defects, involving three or four sides of the root of the affected teeth, that often necessitated more extension of the flap for sufficient visibility for instrumentation and efficient debridement of the intrabony defects and the affected root surfaces [58]. Thus, instead, the standard OFD was employed. Finally, as the included patients stemmed from lower socio-economical levels solely interested in a symptomatic therapy, it was not feasible to reliably include patient-reported outcomes (as self-reported pain scores) in the current investigation.
Within the limitations of current trial, it can be concluded that both treatment modalities (I-PRF + DFDBA and DFDBA alone) resulted in significant improvement in clinical and radiographic parameters 9 months post-surgically. Apart from an observed improvement in gingival recession, combining I-PRF with DFDBA did not appear to significantly augment the DFDBA’s therapeutic outcomes. Further longitudinal clinical and histological studies with larger sample sizes are needed to fully explore the regenerative potential of I-PRF in combination with DFDBA and its efficacy in the treatment of intrabony periodontal defects.
Data availability
Data available on request due to privacy/ethical restrictions.
References
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol 89(Suppl 1):S159-s172. https://doi.org/10.1002/jper.18-0006
Nibali L, Sultan D, Arena C, Pelekos G, Lin GH, Tonetti M (2021) Periodontal infrabony defects: systematic review of healing by defect morphology following regenerative surgery. J Clin Periodontol 48(1):100–113. https://doi.org/10.1111/jcpe.13381
Liang Y, Luan X, Liu X (2020) Recent advances in periodontal regeneration: a biomaterial perspective. Bioact Mater 5(2):297–308. https://doi.org/10.1016/j.bioactmat.2020.02.012
Zhou S, Sun C, Huang S, Wu X, Zhao Y, Pan C, Wang H, Liu J, Li Q, Kou Y (2018) Efficacy of adjunctive bioactive materials in the treatment of periodontal intrabony defects: a systematic review and meta-analysis. Biomed Res Int 2018:8670832. https://doi.org/10.1155/2018/8670832
Choukroun J, Ghanaati S (2018) Reduction of relative centrifugation force within injectable platelet-rich-fibrin (PRF) concentrates advances patients’ own inflammatory cells, platelets and growth factors: the first introduction to the low speed centrifugation concept. Eur J Trauma Emerg Surg 44(1):87–95. https://doi.org/10.1007/s00068-017-0767-9
Miron RJ, Chai J, Zheng S, Feng M, Sculean A, Zhang Y (2019) A novel method for evaluating and quantifying cell types in platelet rich fibrin and an introduction to horizontal centrifugation. J Biomed Mater Res A 107(10):2257–2271. https://doi.org/10.1002/jbm.a.36734
Wend S, Kubesch A, Orlowska A, Al-Maawi S, Zender N, Dias A, Miron RJ, Sader R, Booms P, Kirkpatrick CJ, Choukroun J, Ghanaati S (2017) Reduction of the relative centrifugal force influences cell number and growth factor release within injectable PRF-based matrices. J Mater Sci Mater Med 28(12):188. https://doi.org/10.1007/s10856-017-5992-6
Fujioka-Kobayashi M, Kono M, Katagiri H, Schaller B, Zhang Y, Sculean A, Miron RJ (2021) Histological comparison of platelet rich fibrin clots prepared by fixed-angle versus horizontal centrifugation. Platelets 32(3):413–419. https://doi.org/10.1080/09537104.2020.1754382
Zhao R, Yang R, Cooper PR, Khurshid Z, Shavandi A, Ratnayake J (2021) Bone grafts and substitutes in dentistry: a review of current trends and developments. Molecules 26(10):3007
Kyyak S, Blatt S, Pabst A, Thiem D, Al-Nawas B, Kämmerer PW (2020) Combination of an allogenic and a xenogenic bone substitute material with injectable platelet-rich fibrin - a comparative in vitro study. J Biomater Appl 35(1):83–96. https://doi.org/10.1177/0885328220914407
Sohn D-S, Huang B, Kim J, Park WE, Park CC (2015) Utilization of autologous concentrated growth factors (CGF) enriched bone graft matrix (sticky bone) and CGF-enriched fibrin membrane in implant dentistry. J Implant Adv Clin Dent 7(10):11–18
Dsa E, Chatterjee A, Shetty DN, Pradeep A (2020) Clinical evaluation and comparison of platelet-rich fibrin and injectable platelet-rich fibrin (sticky bone) in the treatment of intrabony defects. Niger J Exp Clin Biosci 8(2):78
Ding ZY, Tan Y, Peng Q, Zuo J, Li N (2021) Novel applications of platelet concentrates in tissue regeneration (Review). Exp Ther Med 21(3):226. https://doi.org/10.3892/etm.2021.9657
Tonetti MS, Sanz M (2019) Implementation of the new classification of periodontal diseases: decision-making algorithms for clinical practice and education. J Clin Periodontol 46(4):398–405. https://doi.org/10.1111/jcpe.13104
Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Beglundh T, Sculean A, Tonetti MS (2020) Treatment of stage I-III periodontitis-the EFP S3 level clinical practice guideline. J Clin Periodontol 47(Suppl 22):4–60. https://doi.org/10.1111/jcpe.13290
Ellis P (2018) The impact of smoking on wound healing: the role of the nurse. Br J Nurs 27(6):S10-s14. https://doi.org/10.12968/bjon.2018.27.6.S10
Naji A, Edman K, Holmlund A (2020) Influence of smoking on periodontal healing one year after active treatment. J Clin Periodontol 47(3):343–350. https://doi.org/10.1111/jcpe.13228
Patel S, Srivastava S, Singh MR, Singh D (2019) Mechanistic insight into diabetic wounds: pathogenesis, molecular targets and treatment strategies to pace wound healing. Biomed Pharmacother 112:108615. https://doi.org/10.1016/j.biopha.2019.108615
Kshirsagar JT, Balamurugan A (2018) Role of sex hormones in periodontium during pregnancy: a review. IJADS 4(4):168–173
Pilloni A, Rojas MA, Marini L, Russo P, Shirakata Y, Sculean A, Iacono R (2021) Healing of intrabony defects following regenerative surgery by means of single-flap approach in conjunction with either hyaluronic acid or an enamel matrix derivative: a 24-month randomized controlled clinical trial. Clin Oral Investig 25(8):5095–5107. https://doi.org/10.1007/s00784-021-03822-x
Agarwal A, Gupta ND, Jain A (2016) Platelet rich fibrin combined with decalcified freeze-dried bone allograft for the treatment of human intrabony periodontal defects: a randomized split mouth clinical trail. Acta Odontol Scand 74(1):36–43. https://doi.org/10.3109/00016357.2015.1035672
O’Leary TJ (1986) The impact of research on scaling and root planing. J Periodontol 57(2):69–75. https://doi.org/10.1902/jop.1986.57.2.69
Tonetti MS, Pini-Prato G, Cortellini P (1993) Periodontal regeneration of human intrabony defects. IV. Determinants of healing response. J Periodontol 64(10):934–940. https://doi.org/10.1902/jop.1993.64.10.934
Ramfjord SP (1967) The periodontal disease index (PDI). J Periodontol 38:602
Francetti L, Del Fabbro M, Basso M, Testori T, Weinstein R (2004) Enamel matrix proteins in the treatment of intra-bony defects. A prospective 24-month clinical trial. J Clin Periodontol 31(1):52–59. https://doi.org/10.1111/j.0303-6979.2004.00437.x
AydemirTurkal H, Demirer S, Dolgun A, Keceli HG (2016) Evaluation of the adjunctive effect of platelet-rich fibrin to enamel matrix derivative in the treatment of intrabony defects. Six-month results of a randomized, split-mouth, controlled clinical study. J Clin Periodontol 43(11):955–964. https://doi.org/10.1111/jcpe.12598
Elbehwashy MT, Hosny MM, Elfana A, Nawar A, Fawzy El-Sayed K (2021) Clinical and radiographic effects of ascorbic acid-augmented platelet-rich fibrin versus platelet-rich fibrin alone in intra-osseous defects of stage-III periodontitis patients: a randomized controlled clinical trial. Clin Oral Investig 25(11):6309–6319. https://doi.org/10.1007/s00784-021-03929-1
Abdulrahman YA, Hosny MM, Elfana A, Fawzy El-Sayed KM (2022) Clinical and radiographic evaluation of low-speed platelet-rich fibrin (PRF) for the treatment of intra-osseous defects of stage-III periodontitis patients: a randomized controlled clinical trial. Clin Oral Investig. https://doi.org/10.1007/s00784-022-04627-2
Graziani F, Karapetsa D, Mardas N, Leow N, Donos N (2018) Surgical treatment of the residual periodontal pocket. Periodontol 2000 76(1):150–163. https://doi.org/10.1111/prd.12156
Cortellini P, Tonetti MS (2005) Clinical performance of a regenerative strategy for intrabony defects: scientific evidence and clinical experience. J Periodontol 76(3):341–350. https://doi.org/10.1902/jop.2005.76.3.341
Miron RJ, Fujioka-Kobayashi M, Hernandez M, Kandalam U, Zhang Y, Ghanaati S, Choukroun J (2017) Injectable platelet rich fibrin (i-PRF): opportunities in regenerative dentistry? Clin Oral Investig 21(8):2619–2627. https://doi.org/10.1007/s00784-017-2063-9
Fujioka-Kobayashi M, Katagiri H, Kono M, Schaller B, Zhang Y, Sculean A, Miron RJ (2020) Improved growth factor delivery and cellular activity using concentrated platelet-rich fibrin (C-PRF) when compared with traditional injectable (i-PRF) protocols. Clin Oral Investig 24(12):4373–4383. https://doi.org/10.1007/s00784-020-03303-7
Wang X, Zhang Y, Choukroun J, Ghanaati S, Miron RJ (2018) Effects of an injectable platelet-rich fibrin on osteoblast behavior and bone tissue formation in comparison to platelet-rich plasma. Platelets 29(1):48–55. https://doi.org/10.1080/09537104.2017.1293807
Aimetti M, Ferrarotti F, Mariani GM, Romano F (2017) A novel flapless approach versus minimally invasive surgery in periodontal regeneration with enamel matrix derivative proteins: a 24-month randomized controlled clinical trial. Clin Oral Investig 21(1):327–337. https://doi.org/10.1007/s00784-016-1795-2
Ferrarotti F, Romano F, Gamba MN, Quirico A, Giraudi M, Audagna M, Aimetti M (2018) Human intrabony defect regeneration with micrografts containing dental pulp stem cells: a randomized controlled clinical trial. J Clin Periodontol 45(7):841–850. https://doi.org/10.1111/jcpe.12931
Aslan S, Buduneli N, Cortellini P (2020) Clinical outcomes of the entire papilla preservation technique with and without biomaterials in the treatment of isolated intrabony defects: a randomized controlled clinical trial. J Clin Periodontol 47(4):470–478. https://doi.org/10.1111/jcpe.13255
Sculean A, Nikolidakis D, Nikou G, Ivanovic A, Chapple IL, Stavropoulos A (2015) Biomaterials for promoting periodontal regeneration in human intrabony defects: a systematic review. Periodontol 2000 68(1):182–216. https://doi.org/10.1111/prd.12086
Castro AB, Meschi N, Temmerman A, Pinto N, Lambrechts P, Teughels W, Quirynen M (2017) Regenerative potential of leucocyte- and platelet-rich fibrin. Part A: intra-bony defects, furcation defects and periodontal plastic surgery. A systematic review and meta-analysis. J Clin Periodontol 44(1):67–82. https://doi.org/10.1111/jcpe.12643
Miron RJ, Moraschini V, Fujioka-Kobayashi M, Zhang Y, Kawase T, Cosgarea R, Jepsen S, Bishara M, Canullo L, Shirakata Y, Gruber R, Ferenc D, Calasans-Maia MD, Wang HL, Sculean A (2021) Use of platelet-rich fibrin for the treatment of periodontal intrabony defects: a systematic review and meta-analysis. Clin Oral Investig 25(5):2461–2478. https://doi.org/10.1007/s00784-021-03825-8
Chen L, Ding Y, Cheng G, Meng S (2021) Use of platelet-rich fibrin in the treatment of periodontal intrabony defects: a systematic review and meta-analysis. Biomed Res Int 2021:6669168. https://doi.org/10.1155/2021/6669168
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(3):e45-50. https://doi.org/10.1016/j.tripleo.2005.07.009
Dohan Ehrenfest DM, Del Corso M, Inchingolo F, Sammartino G, Charrier JB (2010) Platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in human cell cultures: growth factor release and contradictory results. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110(4):418–421. https://doi.org/10.1016/j.tripleo.2010.05.059. author reply 421-412
El Bagdadi K, Kubesch A, Yu X, Al-Maawi S, Orlowska A, Dias A, Booms P, Dohle E, Sader R, Kirkpatrick CJ, Choukroun J, Ghanaati S (2019) Reduction of relative centrifugal forces increases growth factor release within solid platelet-rich-fibrin (PRF)-based matrices: a proof of concept of LSCC (low speed centrifugation concept). Eur J Trauma Emerg Surg 45(3):467–479. https://doi.org/10.1007/s00068-017-0785-7
Agrawal D, Jaiswal P (2020) Injectable platelet rich fibrin (i-PRF): a gem in dentistry. Int J Curr Res Rev 12:25–30
Mourão CF, Valiense H, Melo ER, Mourão NB, Maia MD (2015) Obtention of injectable platelets rich-fibrin (i-PRF) and its polymerization with bone graft: technical note. Rev Col Bras Cir 42(6):421–423. https://doi.org/10.1590/0100-69912015006013
Khosropanah H, Shahidi S, Basri A, Houshyar M (2015) Treatment of Intrabony defects by DFDBA alone or in combination with PRP: a split-mouth randomized clinical and three-dimensional radiographic trial. J Dent (Tehran) 12(10):764–773
Bansal C, Bharti V (2013) Evaluation of efficacy of autologous platelet-rich fibrin with demineralized-freeze dried bone allograft in the treatment of periodontal intrabony defects. J Indian Soc Periodontol 17(3):361–366. https://doi.org/10.4103/0972-124x.115663
Sezgin Y, Uraz A, Taner IL, Çulhaoğlu R (2017) Effects of platelet-rich fibrin on healing of intra-bony defects treated with anorganic bovine bone mineral. Braz Oral Res 31:e15. https://doi.org/10.1590/1807-3107BOR-2017.vol31.0015
Naqvi A, Gopalakrishnan D, Bhasin MT, Sharma N, Haider K, Martande S (2017) Comparative evaluation of bioactive glass putty and platelet rich fibrin in the treatment of human periodontal intrabony defects: a randomized control trial. J Clin Diagn Res 11(7):Zc09-zc13. https://doi.org/10.7860/jcdr/2017/23831.10149
Bodhare GH, Kolte AP, Kolte RA, Shirke PY (2019) Clinical and radiographic evaluation and comparison of bioactive bone alloplast morsels when used alone and in combination with platelet-rich fibrin in the treatment of periodontal intrabony defects-a randomized controlled trial. J Periodontol 90(6):584–594. https://doi.org/10.1002/jper.18-0416
Sharma A, Pradeep AR (2011) Treatment of 3-wall intrabony defects in patients with chronic periodontitis with autologous platelet-rich fibrin: a randomized controlled clinical trial. J Periodontol 82(12):1705–1712. https://doi.org/10.1902/jop.2011.110075
Del Corso M, Sammartino G, Dohan Ehrenfest DM (2009) Re: “Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: a 6-month study.” J Periodontol 80(11):1694–1697. https://doi.org/10.1902/jop.2009.090253. author reply 1697-1699
Kobayashi E, Flückiger L, Fujioka-Kobayashi M, Sawada K, Sculean A, Schaller B, Miron RJ (2016) Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin Oral Investig 20(9):2353–2360. https://doi.org/10.1007/s00784-016-1719-1
Gadkari N, Bawane S, Chopra R, Bhate K, Waknis P, Kakodkar P, Kulkarni D, Kale P (2021) Demineralized freeze-dried bone allograft vs biphasic calcium phosphate: a comparison of two graft materials in sinus augmentation procedures - a pilot study. Adv Oral Maxillofac Surg 4:100177. https://doi.org/10.1016/j.adoms.2021.100177
Vaid T, Kumar S, Mehta R, Shah S, Joshi S, Bhakkand S, Hirani T (2021) Clinical and radiographic evaluation of demineralized freeze-dried bone allograft with concentrated growth factor versus concentrated growth factor alone in the treatment of intrabony defects. Med Pharm Rep 94(2):220–228. https://doi.org/10.15386/mpr-1718
Zhou S, Mizuno S, Glowacki J (2013) Wnt pathway regulation by demineralized bone is approximated by both BMP-2 and TGF-β1 signaling. J Orthop Res 31(4):554–560. https://doi.org/10.1002/jor.22244
Nibali L, Koidou VP, Nieri M, Barbato L, Pagliaro U, Cairo F (2020) Regenerative surgery versus access flap for the treatment of intra-bony periodontal defects: a systematic review and meta-analysis. J Clin Periodontol 47(Suppl 22):320–351. https://doi.org/10.1111/jcpe.13237
Cortellini P, Tonetti MS (2015) Clinical concepts for regenerative therapy in intrabony defects. Periodontol 2000 68(1):282–307. https://doi.org/10.1111/prd.12048
Acknowledgements
The authors thank Dr. Ahmed Elfana for his excellent statistical analysis and Dr. Mona Nour (M.N.) for the great clinical and radiographic evaluation.
Funding
Open Access funding enabled and organized by Projekt DEAL. The work was supported by the Department of Oral Medicine and Periodontology, Faculty of Dentistry, Cairo University, Egypt.
Author information
Authors and Affiliations
Contributions
M.A., K.F.E., W.E., and M.H.: conception and design of the clinical trial; M.A.: surgical procedures; W.E. and M.H.: data acquisition, analysis, and interpretation; M.A.: drafting of the manuscript; K.F.E. and M.H.: data interpretation and manuscript revision and approval. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alshoiby, M.M., Fawzy El-Sayed, K.M., Elbattawy, W. et al. Injectable platelet-rich fibrin with demineralized freeze-dried bone allograft compared to demineralized freeze-dried bone allograft in intrabony defects of patients with stage-III periodontitis: a randomized controlled clinical trial. Clin Oral Invest 27, 3457–3467 (2023). https://doi.org/10.1007/s00784-023-04954-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04954-y