Abstract
Objectives
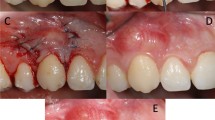
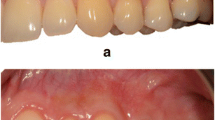
Aim of this clinical study was to evaluate the effects on gingival thickness of three surgical techniques for root coverage: the coronally advanced flap (CAF) alone, with a sub-epithelial connective tissue graft (SCTG) or with leukocyte- and platelet-rich fibrin (L-PRF) membranes.
Methods
Sixty patients with RT1 single maxillary gingival recession were treated with CAF + L-PRF (20 patients), CAF + SCTG (20 patients) or CAF alone (20 patients). At baseline and 6-month after treatment, gingival thickness (GT), keratinized tissue width (KT), gingival recession (GR), clinical attachment level (CAL), probing depth (PD), PROMs, and the aesthetic outcome were recorded.
Results
CAF + SCTG and CAF + L-PRF groups showed a significantly greater mean GT increase than CAF alone (0.31 ± 0.10 mm) with no significant differences between CAF + SCTG (0.99 ± 0.02 mm) and CAF + L-PRF (0.92 ± 0.52 mm) groups (p = 0.55). CAF + SCTG was associated with a significantly greater KT gain (3.85 ± 1.04 mm), while in CAF + L-PRF (2.03 ± 0.53 mm) and CAF (1.50 ± 0.69 mm) groups, KT was not significantly increased. Both GR and CAL showed a significant within groups’ improvement, without among-groups differences. No significant among-groups difference for the aesthetic outcome but greater discomfort and pain-killer consumption in CAF + SCTG group was detected.
Conclusion
All investigated surgical techniques produced significant GR reduction and CAL gain. GT was similarly augmented by CAF + L-PRF and CAF + SCTG techniques; however, the CAF + SCTG technique produced a more predictable KT and GT increase.
Clinical relevance
The results of our study suggest that the CAF + SCTG technique represents the most predictable method for the clinician to improve the gingival phenotype, an important factor for long term gingival margin stability.




Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article, its supplementary materials, and from the corresponding author [author MP] on request.
References
Jepsen S, Caton JG, Albandar JM et al (2018) Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89(Suppl 1):S237–S248. https://doi.org/10.1002/JPER.17-0733
Zweers J, Thomas RZ, Slot DE, Weisgold AS, Van der Weijden FGA (2014) Characteristics of periodontal biotype, its dimensions, associations and prevalence: a systematic review. J Clin Periodontol 41(10):958–971. https://doi.org/10.1111/jcpe.12275
Maroso FB, Gaio EJ, Rösing CK, Fernandes MI (2015) Correlation between gingival thickness and gingival recession in humans. Acta Odontol Latinoam AOL 28(2):162–166. https://doi.org/10.1590/S1852-48342015000200011
Hwang D, Wang HL (2006) Flap thickness as a predictor of root coverage: a systematic review. J Periodontol 77(10):1625–1634. https://doi.org/10.1902/jop.2006.060107
Kim DM, Neiva R (2015) Periodontal soft tissue non-root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol 86(2 Suppl):S56-72. https://doi.org/10.1902/jop.2015.130684
Chambrone L, Tatakis DN (2016) Long-term outcomes of untreated buccal gingival recessions: a systematic review and meta-Analysis. J Periodontol 87(7):796–808. https://doi.org/10.1902/jop.2016.150625
Parameters of Care (2000) American Academy of Periodontology. J Periodontol 71(5 Suppl):i-ii, 847–883. https://doi.org/10.1902/jop.2000.71.5-S.i
Cairo F, Cortellini P, Pilloni A et al (2016) Clinical efficacy of coronally advanced flap with or without connective tissue graft for the treatment of multiple adjacent gingival recessions in the aesthetic area: a randomized controlled clinical trial. J Clin Periodontol 43(10):849–856. https://doi.org/10.1111/jcpe.12590
Cortellini P, Pini Prato G (2012) Coronally advanced flap and combination therapy for root coverage. Clinical strategies based on scientific evidence and clinical experience. Periodontol 2000 59(1):158–184. https://doi.org/10.1111/j.1600-0757.2011.00434.x
Bhatavadekar NB, Gharpure AS, Chambrone L (2019) Long-term outcomes of coronally advanced tunnel flap (CATF) and the envelope flap (mCAF) plus subepithelial connective tissue graft (SCTG) in the treatment of multiple recession-type defects: a 6-year retrospective analysis. Int J Periodontics Restorative Dent 39(5):623–630. https://doi.org/10.11607/prd.4026
Zucchelli G, Mele M, Stefanini M et al (2010) Patient morbidity and root coverage outcome after subepithelial connective tissue and de-epithelialized grafts: a comparative randomized-controlled clinical trial. J Clin Periodontol 37(8):728–738. https://doi.org/10.1111/j.1600-051X.2010.01550.x
Zucchelli G, Mounssif I, Mazzotti C et al (2014) Coronally advanced flap with and without connective tissue graft for the treatment of multiple gingival recessions: a comparative short- and long-term controlled randomized clinical trial. J Clin Periodontol 41(4):396–403. https://doi.org/10.1111/jcpe.12224
Del Corso M, Vervelle A, Simonpieri A et al (2012) Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 1: Periodontal and dentoalveolar surgery. Curr Pharm Biotechnol 13(7):1207–1230. https://doi.org/10.2174/138920112800624391
Bansal M, Kumar A, Puri K, Khatri M, Gupta G, Vij H (2016) Clinical and histologic evaluation of platelet-rich fibrin accelerated epithelization of gingival wound. J Cutan Aesthetic Surg 9(3):196–200. https://doi.org/10.4103/0974-2077.191647
Femminella B, Iaconi MC, Di Tullio M et al (2016) Clinical comparison of platelet-rich fibrin and a gelatin sponge in the management of palatal wounds after epithelialized free gingival graft harvest: a randomized clinical trial. J Periodontol 87(2):103–113. https://doi.org/10.1902/jop.2015.150198
DohanEhrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T (2014) Classification of platelet concentrates (platelet-rich plasma-PRP, platelet-rich fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J 4(1):3–9
Bielecki T, DohanEhrenfest DM (2012) Leukocyte- and platelet-rich plasma (L-PRP)/fibrin (L-PRF) in medicine - past, present, future. Curr Pharm Biotechnol 13(7):i–ii. https://doi.org/10.2174/138920112800624274
Barootchi S, Tavelli L, Di Gianfilippo R et al (2022) Soft tissue phenotype modification predicts gingival margin long-term (10-year) stability: longitudinal analysis of six randomized clinical trials. J Clin Periodontol 49(7):672–683. https://doi.org/10.1111/jcpe.13641
Thamaraiselvan M, Elavarasu S, Thangakumaran S, Gadagi JS, Arthie T (2015) Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian Soc Periodontol 19(1):66–71. https://doi.org/10.4103/0972-124X.145790
Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D (2009) Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: a 6-month study. J Periodontol 80(2):244–252. https://doi.org/10.1902/jop.2009.080253
Kuka S, Ipci SD, Cakar G, Yılmaz S (2018) Clinical evaluation of coronally advanced flap with or without platelet-rich fibrin for the treatment of multiple gingival recessions. Clin Oral Investig 22(3):1551–1558. https://doi.org/10.1007/s00784-017-2225-9
Eren G, Atilla G (2014) Platelet-rich fibrin in the treatment of localized gingival recessions: a split-mouth randomized clinical trial. Clin Oral Investig 18(8):1941–1948. https://doi.org/10.1007/s00784-013-1170-5
Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U (2011) The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: an explorative and reliability study: Interproximal CAL for gingival recessions. J Clin Periodontol 38(7):661–666. https://doi.org/10.1111/j.1600-051X.2011.01732.x
The CONSORT Group. CONSORT. Available at http://www.consort-statement.org/. Accessed 2 May 2013
O’Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43(1):38. https://doi.org/10.1902/jop.1972.43.1.38
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25(4):229–235
Mufti S, Dadawala SM, Patel P, Shah M, Dave DH (2017) Comparative evaluation of platelet-rich fibrin with connective tissue grafts in the treatment of Miller’s class I gingival recessions. Contemp Clin Dent 8(4):531–537. https://doi.org/10.4103/ccd.ccd_325_17
Vandana KL, Gupta I (2016) The relation of gingival thickness to dynamics of gingival margin position pre- and post-surgically. J Indian Soc Periodontol 20(2):167–173. https://doi.org/10.4103/0972-124X.175173
Paolantonio1 M, Murro C di, Cattabriga A, Cattabriga M (1997) Subpedicle connective tissue graft versus free gingival graft in the coverage of exposed root surfaces a 5-year clinical study. J Clin Periodontol 24(1):51–56. https://doi.org/10.1111/j.1600-051X.1997.tb01184.x
Cairo F, Rotundo R, Miller PD, Pini Prato GP (2009) Root coverage esthetic score: a system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical cases. J Periodontol 80(4):705–710. https://doi.org/10.1902/jop.2009.080565
de Sanctis M, Zucchelli G (2007) Coronally advanced flap: a modified surgical approach for isolated recession-type defects: three-year results. J Clin Periodontol 34(3):262–268. https://doi.org/10.1111/j.1600-051X.2006.01039.x
Dohan DM, Choukroun J, Diss A et al (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(3):e45–50. https://doi.org/10.1016/j.tripleo.2005.07.009
Wei Y, Cheng Y, Wang Y, Zhang X, Miron RJ, Zhang Y (2022) The effect of resting and compression time post-centrifugation on the characteristics of platelet rich fibrin (PRF) membranes. Clin Oral Investig 26(8):5281–5288. https://doi.org/10.1007/s00784-022-04496-9
Kan JYK, Morimoto T, Rungcharassaeng K, Roe P, Smith DH (2010) Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent 30(3):237–243
DohanEhrenfest DM, Pinto NR, Pereda A et al (2018) The impact of the centrifuge characteristics and centrifugation protocols on the cells, growth factors, and fibrin architecture of a leukocyte- and platelet-rich fibrin (L-PRF) clot and membrane. Platelets 29(2):171–184. https://doi.org/10.1080/09537104.2017.1293812
Zucchelli G, Marzadori M, Mounssif I, Mazzotti C, Stefanini M (2014) Coronally advanced flap + connective tissue graft techniques for the treatment of deep gingival recession in the lower incisors. A controlled randomized clinical trial. J Clin Periodontol 41(8):806–813. https://doi.org/10.1111/jcpe.12269
Zucchelli G, Marzadori M, Mele M, Stefanini M, Montebugnoli L (2012) Root coverage in molar teeth: a comparative controlled randomized clinical trial. J Clin Periodontol 39(11):1082–1088. https://doi.org/10.1111/jcpe.12002
Stefanini M, Jepsen K, de Sanctis M et al (2016) Patient-reported outcomes and aesthetic evaluation of root coverage procedures: a 12-month follow-up of a randomized controlled clinical trial. J Clin Periodontol 43(12):1132–1141. https://doi.org/10.1111/jcpe.12626
Padma R, Shilpa A, Kumar PA, Nagasri M, Kumar C, Sreedhar A (2013) A split mouth randomized controlled study to evaluate the adjunctive effect of platelet-rich fibrin to coronally advanced flap in Miller’s class-I and II recession defects. J Indian Soc Periodontol 17(5):631–636. https://doi.org/10.4103/0972-124X.119281
Eren G, Kantarcı A, Sculean A, Atilla G (2016) Vascularization after treatment of gingival recession defects with platelet-rich fibrin or connective tissue graft. Clin Oral Investig 20(8):2045–2053. https://doi.org/10.1007/s00784-015-1697-8
Gordon HP, Sullivan HC, Atkins JH (1968) Free autogenous gingival grafts. II. Supplemental findings--histology of the graft site. Periodontics 6(3):130–133
Öncü E (2017) The use of platelet-rich fibrin versus subepithelial connective tissue graft in treatment of multiple gingival recessions: a randomized clinical trial. Int J Periodontics Restorative Dent 37(2):265–271. https://doi.org/10.11607/prd.2741
Pini Prato G, Tinti C, Vincenzi G, Magnani C, Cortellini P, Clauser C (1992) Guided tissue regeneration versus mucogingival surgery in the treatment of human buccal gingival recession. J Periodontol 63(11):919–928. https://doi.org/10.1902/jop.1992.63.11.919
Jankovic S, Aleksic Z, Milinkovic I, Dimitrijevic B (2010) The coronally advanced flap in combination with platelet-rich fibrin (PRF) and enamel matrix derivative in the treatment of gingival recession: a comparative study. Eur J Esthet Dent Off J Eur Acad Esthet Dent 5(3):260–273
Del Corso M, Sammartino G, Dohan Ehrenfest DM (2009) Re: “Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: a 6-month study.” J Periodontol 80(11):1694–1697; author reply 1697–1699. https://doi.org/10.1902/jop.2009.090253
Kattlove HE, Alexander B (1971) The effect of cold on platelets. I. Cold-induced platelet aggregation. Blood 38(1):39–48
Aldana CA, Ruiz AS, Messina DR, Quirynen M, Carrasco NP (2021) Leukocyte- and platelet-rich fibrin versus connective tissue graft for a coronally advanced flap in the treatment of Miller class I and II localized gingival recessions: a randomized controlled clinical trial. Int J Periodontics Restorative Dent 41(6):e287–e296. https://doi.org/10.11607/prd.5093
Cairo F, Cortellini P, Nieri M et al (2020) Coronally advanced flap and composite restoration of the enamel with or without connective tissue graft for the treatment of single maxillary gingival recession with non-carious cervical lesion. A randomized controlled clinical trial. J Clin Periodontol 47(3):362–371. https://doi.org/10.1111/jcpe.13229
Gil S, de la Rosa M, Mancini E et al (2021) Coronally advanced flap achieved higher esthetic outcomes without a connective tissue graft for the treatment of single gingival recessions: a 4-year randomized clinical trial. Clin Oral Investig 25(5):2727–2735. https://doi.org/10.1007/s00784-020-03587-9
Müller HP, Eger T (2002) Masticatory mucosa and periodontal phenotype: a review. Int J Periodontics Restorative Dent 22(2):172–183
Barootchi S, Tavelli L, Zucchelli G, Giannobile WV, Wang HL (2020) Gingival phenotype modification therapies on natural teeth: a network meta-analysis. J Periodontol 91(11):1386–1399. https://doi.org/10.1002/JPER.19-0715
Rasperini G, Acunzo R, Pellegrini G et al (2018) Predictor factors for long-term outcomes stability of coronally advanced flap with or without connective tissue graft in the treatment of single maxillary gingival recessions: 9 years results of a randomized controlled clinical trial. J Clin Periodontol 45(9):1107–1117. https://doi.org/10.1111/jcpe.12932
Pini Prato G, Rotundo R, Franceschi D, Cairo F, Cortellini P, Nieri M (2011) Fourteen-year outcomes of coronally advanced flap for root coverage: follow-up from a randomized trial. J Clin Periodontol 38(8):715–720. https://doi.org/10.1111/j.1600-051X.2011.01744.x
Pini Prato GP, Franceschi D, Cortellini P, Chambrone L (2018) Long-term evaluation (20 years) of the outcomes of subepithelial connective tissue graft plus coronally advanced flap in the treatment of maxillary single recession-type defects. J Periodontol 89(11):1290–1299. https://doi.org/10.1002/JPER.17-0619
Cheng YF, Chen JW, Lin SJ, Lu HK (2007) Is coronally positioned flap procedure adjunct with enamel matrix derivative or root conditioning a relevant predictor for achieving root coverage? A systemic review. J Periodontal Res 42(5):474–485. https://doi.org/10.1111/j.1600-0765.2007.00971.x
Zucchelli G, Mele M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M (2009) Coronally advanced flap with and without vertical releasing incisions for the treatment of multiple gingival recessions: a comparative controlled randomized clinical trial. J Periodontol 80(7):1083–1094. https://doi.org/10.1902/jop.2009.090041
Tatakis DN, Chambrone L (2016) The effect of suturing protocols on coronally advanced flap root-coverage outcomes: a meta-analysis. J Periodontol 87(2):148–155. https://doi.org/10.1902/jop.2015.150394
Acknowledgements
Authors report no conflicts of interest related to this study. The trial director was Michele Paolantonio, Department of Innovative Technologies in Medicine & Dentistry, “G. D’Annunzio” University, Chieti-Pescara, Italy.
Author information
Authors and Affiliations
Contributions
PS, PdN, MP and BF are co-first Authors having designed, written, revised and edited the work; LS and GP collaborated in designing, writing and editing the study; MS and IR cooperated in the study design, article editing and revising; LR collaborated in interpretation of data, article editing, and data collection with IR and BF. PdN did the statistical analysis.
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study protocol was registered at ClinicalTrials.gov as NCT03712852 after the approval obtained by the G. D’Annunzio University ethic committee. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained according to the protocol from all participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Santamaria, P., Paolantonio, M., Romano, L. et al. Gingival phenotype changes after different periodontal plastic surgical techniques: a single-masked randomized controlled clinical trial. Clin Oral Invest 27, 3423–3435 (2023). https://doi.org/10.1007/s00784-023-04944-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04944-0