Abstract
Introduction
A 28.2 μg twice-weekly formulation of teriparatide (2/W-TPD) was developed to provide comparably high efficacy for osteoporosis to a 56.5 μg once-weekly formulation while improving the safety and persistence rate. In the current study, we aimed to elucidate the real-world persistence of 2/W-TPD and to identify the factors associated with the discontinuation of 2/W-TPD in patients with severe osteoporosis.
Materials and methods
This retrospective study included 90 patients who were treated with 2/W-TPD at three hospitals in Japan. Patient information was collected, including age, sex, distance to the hospital, family structure, comorbidities, previous treatment for osteoporosis, timing of the injection, side effects and duration of 2/W-TPD treatment, barthel index (BI), and bone mineral density (BMD) of the lumbar spine and femoral neck. We examined the factors influencing 2/W-TPD discontinuation using the Cox proportional hazards model.
Results
The 12 month completion rate of 2/W-TPD therapy was 47.5%. The Cox hazard analysis identified side effects [Hazard Ratio (HR) = 14.59, P < 0.001], low BMD of the femoral neck (HR = 0.04, P = 0.002), and morning injection (HR = 3.29, P = 0.006) as risk factors influencing the discontinuation of 2/W-TPD. Other variables, including age, did not contribute to the continuation of 2/W-TPD.
Conclusion
One year continuation rate of 2/W-TPD was higher than the previously reported value of the once-weekly formulation in real-world setting, probably due to the lower incidence of side effects. Introducing injection of 2/W-TPD may further improve the persistence of TPD therapy for osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In aging societies, including those in Japan, efforts to treat osteoporosis across the nation are becoming more critical. Approximately 30% of all postmenopausal women have osteoporosis [1], and 9 million new osteoporosis-related fractures were reported worldwide in 2000 [2]. Drug treatment is the basis for osteoporosis treatment and various drugs are available. Teriparatide (TPD) [3], which is one of the medicines used to treat osteoporosis, has been demonstrated to exhibit potent anabolic effects on bone in several animal models and humans [4, 5] and is recommended for patients at high risk of fracture [6,7,8].
Before 2019, two types of TPD preparations were available in Japan: a once-weekly 56.5 μg TPD formulation (1/W-TPD), administered subcutaneously by a physician or nurse once per week, and a daily 20 μg TPD formulation (daily TPD), administered as self-injection. Both regimens have been reported to increase the bone mineral density (BMD) of the spine and reduce the risk of vertebral fractures, with comparable effects [7, 9]. 1/W-TPD is unlikely to induce histologic changes, such as cortical porosity, which were observed following daily TPD administration in a non-clinical study [10]. However, some patients find it difficult to continue 1/W-TPD treatment because of the high frequency of hospital visits or side effects [11, 12]. In Japan, to improve patient compliance, a self-administered 28.2 μg teriparatide formulation for twice-weekly use (2/W-TPD) (Teribone Auto injector®, Asahi Kasei Pharma Co., Ltd., Tokyo, Japan) became commercially available in December 2019. In the TWICE study, a phase 3 non-inferiority study, 2/W-TPD was shown to reduce the incidence of adverse drug reactions such as nausea and pyrexia compared to 1/W-TPD [13]. These results suggest that 2/W-TPD is an easier formulation for patients to continue than 1/W-TPD.
The outbreak of the coronavirus disease 2019 (COVID-19) [14] established a new normal in medicine. Considering the need for rigorous infection prevention, paying constant attention to physical contacts, and reduction in the frequency of hospital visits, the Japanese Osteoporosis Society and the Japanese Society for Bone Metabolism recommended switching to 2/W-TPD in patients receiving 1/W-TPD who have difficulty continuing it. However, the continuation rates and factors affecting the continuation of 2/W-TPD in real-world settings have not been clarified. This study aimed to examine the persistence rate of 2/W-TPD and the factors affecting treatment discontinuation in patients with severe osteoporosis.
Materials and methods
Study design
This retrospective study was conducted in accordance with the ethical standards of the Helsinki Declaration of 1975 as revised in 1983. Three spine centers staffed with board-certified spine surgeons participated in this retrospective study in Hokkaido, Japan. The study was based on data obtained from medical records and imaging findings of osteoporosis patients. The requirement for patient informed consent was waived, owing to the retrospective nature of the study and its unidentified data (approval numbers of Hokkaido Orthopedic Memorial Hospital, Hakodate Central General Hospital, and KKR Sapporo Medical Center are 92, 10, and 28 respective).
Patients
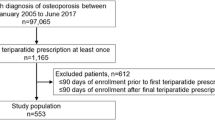
We retrospectively reviewed the medical records of patients who underwent 2/W-TPD treatment between December 2019 and 2021 at three hospitals in the urban regions of Japan. Among these patients, those who could be followed up for at least 6 months were surveyed. Patients with a history of metabolic bone diseases other than osteoporosis or malignancies were excluded from the study. There were a total of 90 patients who met the inclusion criteria of the study. All patients at high risk for fracture were defined as follows: (1) lumbar BMD < − 3.3 of standard deviation (SD) [15, 16]; (2) hip or lumbar BMD < − 2.5 of SD and one or more fragility fractures; (3) two or more fragility fractures [15, 17]; or (4) semi-quantitative evaluation [18] of existing grade 3 vertebral fracture [17].
Administration of 2/W-TPD
Briefly, this product is an auto-injector formulation that contains a single-use needle that needs no replacement [19]. The injection was completed by removing the cap and pressing the tip of the auto-injector against the site of administration in two steps, making it easy for elderly patients to self-inject. This formulation was refrigerated at home, and all patients were injected twice a week by themselves or their family members living with them. Regarding the timing of the injections, no specific instructions were given, as the patients were allowed to follow their own preferences.
Introduction and the continuation of 2/W-TPD
All patients were informed by their physicians regarding the need to introduce 2/W-TPD or switch from previous medications. They were also informed in detail about the cost and use of the formulation by the nurse before the first use. All patients agreed on the treatment strategy of osteoporosis and cost of 2/W-TPD and started the 2/W/TPD treatment. They visited the same hospital every 1–3 months to receive this formulation. In all hospitals, elderly patients received ongoing intervention including telephone contact from osteoporosis managers for the continuation after the start of 2/W-TPD through the Osteoporosis Liaison Service (OLS) activities.
Subjects and persistence measure of 2/W-TPD
Patient information included age, sex, distance to the hospital, family structure, reason for the start of 2/W-TPD administration, comorbidities treated at the same hospital, previous treatment for osteoporosis, history of fracture, side effects of 2/W-TPD, duration of 2/W-TPD treatment, injection timing (morning or evening), and fracture during 2/W-TPD treatment. We defined morning as the period from just after waking up to noon; evening as the period from before dinner to just before going to sleep. The mobility scale of the Barthel Index (BI) was used to quantitatively assess gait independence [20]. The BI is widely used for activities of daily living (ADL) scale [21], and can assess gait ability on a four-point scale of 0, 5, 10, and 15 points; briefly, 0: unable to walk, 5: able to self-propel a wheelchair for 45 min, 10: able to walk with assistance for more than 45 min, and 15: able to walk alone for more than 45 min. BMD measurements were performed in all patients before and 1 year after the start of 2/W-TPD treatment, using the anteroposterior views of the lumbar spine (L2–L4) and femoral neck.
The persistence rate of 2/W-TPD was assessed at 6 months and 1 year of treatment. Because of a short-term study in a special environment of COVID-19, we defined the completion of the study as the achievement of 1 year of 2/W-TPD treatment instead of 2 years, which is the maximum duration of TPD administration. If the patient did not report the date of treatment discontinuation, the date of the last follow-up was considered as the endpoint. The duration was measured by clinical records and calculation of the number of the formulation prescribed since treatment initiation. We defined a 1 month continuance as the period from the date of commencement of use to the same day of the following month. All patients were followed up with sequential treatment. Therefore, the exact duration of treatment was determined on a monthly basis, regarding whether patients continued to use 2/W-TPD or not.
Statistical analysis
All continuous variables were expressed as mean ± standard deviation (SD). 2/W-TPD continuation curves were drawn using the Kaplan–Meier method, and differences were analyzed using the log-rank test for variables including age, living alone or not, presence or absence of osteoporosis treatment history, timing of injection (morning or evening), presence or absence of side effects of 2/W-TPD, and reason for the start of 2/W-TPD (fracture or examination). Considering previous reports that older age affects the continuation rate of 1/W-TPD and daily TPD, we divided patients into two groups: late-stage elderly (≥ 75 years of age) and early-stage elderly (< 75 years of age). The Cox proportional hazards model was used to identify factors associated with the continuation of 2/W-TPD; for variable selection, backward and forward stepwise regression with minimum Bayesian information criterion (BIC) was used. An unpaired t test was performed to compare the percent change from the baseline BMD between patients who received 2/W-TPD in the morning or evening. Results with P values less than 0.05 were considered statistically significant. All statistical analyses were performed using JMP Pro version 16.0 software (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics and disease status of patients
The patient demographics and clinicopathological information are presented in Table 1. The mean age of the patients treated with 2/W-TPD was 78.5 years (range 54–99), and 95.6% were women. A total of 45.9% of the patients were prescribed other osteoporosis medications before receiving 2/W-TPD treatment. Six patients were transferred from daily TPD to 2/W-TPD. Nineteen patients were prescribed active vitamin D preparations, and 16 of them took Vitamin D in combination with other medications. A total of 54% of patients received their injections in the evening. A total of 73.3% of patients had concomitant diseases other than osteoporosis and were being treated at the same hospital. A total of 75.5% of patients started receiving 2/W-TPD treatment after a fracture. A total of 70% of patients were able to walk alone, and the BI score was 15 points.
The completion rate of 2/W-TPD treatment and the frequency of side effects
The results regarding the continuation of 2/W-TPD and the occurrence of side effects are shown in Tables 2 and 3. The completion rates of 2/W-TPD at 6 and 12 months were 72.2% (65 of 90) and 47.5% (39 of 82), respectively, with the exception of 8 patients receiving ongoing treatment. Regarding the sequential therapy, out of 43 patients who discontinued 2/W-TPD treatment before a year, 6 patients were switched to denosumab, 2 patients were switched to romosozumab, 33 patients were switched to bisphosphonates, and 2 patients were switched to selective estrogen modulator and active vitamin D preparation. Fractures during 2/W-TPD treatment occurred in 2 patients (vertebral body fracture and radius fracture). Side effects occurred in 33.3% (30 of 90) patients, and the most frequent side effect was nausea, which occurred in 14 patients. Out of 14 patients, 12 received nausea in the first 6 months after receiving 2/W-TPD. Regarding dizziness, which occurred in 8 patients, 4 patients received dizziness in the first 6 months after receiving 2/W-TPD treatment.
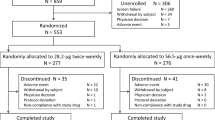
Analysis of factors influencing the discontinuation of 2/W-TPD treatment
Next, we drew 2/W-TPD continuation curves using the Kaplan–Meier method and compared the factors associated with the discontinuation of 2/W-TPD using the log-rank test. There were no significant differences between the two groups in the late-stage elderly (≥ 75 years of age) and early-stage elderly (< 75 years of age) groups, living alone or not, presence or absence of osteoporosis treatment history, or reason for the start of 2/W-TPD (fracture or examination). The rate of 2/W-TPD discontinuation significantly increased in the group of patients with side effects and TPD administration in the morning (P < 0.001 and P = 0.002, respectively) (Fig. 1).
Comparison of factors associated with the discontinuation of twice-weekly teriparatide formulation (2/W-TPD) using the Kaplan–Meier curves: late-stage elderly (≥ 75 years of age) vs. early-stage elderly (< 75 years of age) (a), living alone or not (b), presence or absence of osteoporosis treatment history (c), timing of injection (morning or evening) (d), presence or absence of side effects of 2/W-TPD (e), and the reason for the start of 2/W-TPD (fracture or examination) (f)
The results of the Cox hazard analysis also showed that the risk factors for 2/W-TPD discontinuation were side effects [Hazard Ratio (HR) = 14.59, P < 0.001], BMD of the femoral neck before 2/W-TPD treatment (HR = 0.04, P = 0.002), and injection in the morning (HR = 3.29, P = 0.006) (Table 4). Age, sex, number of family members living together, living with a young generation, distance to hospital, history of osteoporosis treatment, BMD of the lumbar spine, BI, and comorbidities treated at the same hospital were not associated with 2/W-TPD discontinuation (data not shown).
The effect of 1-year 2/W-TPD treatment on the BMD of the lumbar spine and femoral neck
The BMD of the lumbar spine and femoral neck were measured before and 1 year after the start of 2-W/TPD treatment. In patients who were able to continue 2/W-TPD for 1 year, BMD of the lumbar spine and femur increased by an average of 4.9 and 1.5%, respectively, from the baseline.
In addition, we compared the changes in BMD in the lumbar spine and femoral neck between patients who received 2/W-TPD in the morning and evening. Patients in both groups showed an elevation in bone mineral density at the lumbar spine and femoral neck, but there was no significant difference between the two groups (Fig. 2).
Discussion
This study focused on the continuation rate of 2/W-TPD and the factors affecting treatment discontinuation in patients with severe osteoporosis. The results showed that completion rates of 2/W-TPD at 6 and 12 months were 72.2 and 47.5%, respectively. In the previous reports, the continuation rate at 12 months of the daily TPD formulation ranged from 43.1 to 87% [11, 22,23,24,25,26], while that of the 1/W-TPD formulation was approximately 16.8–23.5% [12, 27]. Although the 1 year persistence rate of the present study was much lower than that of the TWICE study, which was reported as 87.4% [13], it was higher than that of the 1 year persistence rate of the previous 1/W-TPD in clinical practice. To the best of our knowledge, this is the first study to demonstrate the continuation rate of 2/W-TPD in real-world settings, despite the special environment of COVID-19. The results of this study suggest that 2/W-TPD is more likely to be continued than 1/W-TPD.
Our results indicated that side effects were associated with the discontinuation of 2/W-TPD. This was similar to previous reports, in which side effects were associated with a negative influence on TPD continuation rates [28]. In the present study, the incidence of side effects of 2/W-TPD was 32.2%, which was comparable to the results of the TWICE study [13]. The main side effects of 2/W-TPD were nausea and dizziness, which accounted for 75.0% of all side effects (Table 3). As with previous reports [12], nausea has been cited as one of the major reasons for the difficulty with treatment continuation in 1/W-TPD. In the present study, 85.7% (12/14) of patients received nausea in the first 6 month after starting 2/W-TPD and 92.8% (13/14) of all patients were unable to continue for 1 year. Therefore, it is important to inform patients that nausea may occur in the early phase of the treatment before 2/W-TPD initiation, and the use of medications to stop nausea should be considered in some cases. Since TPD has relaxant effects on vascular smooth muscles [29], it can induce hypotension and vasovagal reflex, causing nausea and dizziness after administration. Prevention of teriparatide-induced hypotension by drinking water before and after administration may be helpful in reducing complications and improving the continuation rate [28, 30].
Our results also showed that morning injection was a risk factor for the discontinuation of 2/W-TPD. A possible explanation for this is that the incidence of side effects may have been higher after waking up because patients were often dehydrated and prone to hypotension. The present study showed that there was no significant difference in the increase in lumbar spine BMD between patients with 2/W-TPD in the morning and evening; however, a previous study reported that a 12 month morning daily TPD administration resulted in a larger increase in lumbar spine BMD than an evening administration [31]. Further analysis is needed to investigate the appropriate timing of TPD injections in patients with osteoporosis.
Low BMD of the femoral neck was another risk factor associated with discontinuation of 2/W-TPD. However, in this study, we were not able to clearly interpret this result. We expected that patients with low BMD of the femoral neck would include those who could not walk much and/or had low ADL, which made it difficult for them to visit the hospital to receive the 2/W-TPD formulation. According to a previous report, among patients diagnosed with osteoporosis, those who were confined to wheelchairs or beds showed a negative correlation with osteoporosis treatment [32]. Thus, we investigated the BI of osteoporosis patients; however, contrary to our expectations, the BI did not affect the discontinuation of 2/W-TPD in the present study.
It is worth mentioning that age was not associated with the discontinuation of 2/W-TPD. This result differs from previous reports that showed age as a significant factor in the continuation of both 1/W-TPD and daily TPD [24, 28, 33]. There are several possible reasons for this result. First, 2/W-TPD is a relatively easy to administer device, even for the elderly; it does not require the attachment of a needle and has a single-use syringe. Second, all three hospitals in this study were relatively active in OLS activities. In these hospitals, nurses and osteoporosis managers actively intervened by contacting the homes of elderly patients or those living alone, after the start of the 2/W-TPD. Previous reports have shown that OLS activities may be related to treatment continuation rates [34], and these hospitals may have provided an appropriate environment for the elderly to continue 2/W-TPD treatment.
This study had several limitations. First, the sample size was small. Second, because all hospitals in this study were in relatively urban areas, it is not certain whether the results would be the same in rural areas, where transportation is limited. Third, there was a potential for selection bias because the study was conducted in hospitals where OLS activities were intensive. Furthermore, no definite conclusions were made regarding whether the continuation rate and factors affecting the discontinuation of 2/W-TPD are the same in the setting of COVID-19 subsidence. Our results may be useful for increasing the continuation rate of 2/W-TPD in the setting of COVID-19, where respiratory disease continue to occur; however, further research is required in the post-COVID-19 context, especially to investigate the real-world continuation rate.
In conclusion, our results showed that the continuation rate of 2/W-TPD at 12 months was 47.5%, which was relatively higher than that of 1/W-TPD in the previous reports. Side effects, low BMD of the femoral neck, and morning injections were risk factors for the discontinuation of 2/W-TPD. Twice a week, teriparatide is relatively easy to use even in the elderly and may contribute to increasing the rate of continuation of osteoporosis treatment by controlling side effects and the timing of injections.
References
Melton LJ, Chrischilles EA, Cooper C, Lane AW, Riggs BL (1992) Perspective how many women have osteoporosis? (In Eng). J Bone Miner Res 7:1005–1010. https://doi.org/10.1002/jbmr.5650070902
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Komatsubara S, Mori S, Mashiba T, Nonaka K, Seki A, Akiyama T, Miyamoto K, Cao Y, Manabe T, Norimatsu H (2005) Human parathyroid hormone (1–34) accelerates the fracture healing process of woven to lamellar bone replacement and new cortical shell formation in rat femora. Bone 36:678–687. https://doi.org/10.1016/j.bone.2005.02.002
Andreassen TT, Ejersted C, Oxlund H (1999) Intermittent parathyroid hormone (1–34) treatment increases callus formation and mechanical strength of healing rat fractures. J Bone Miner Res 14:960–968. https://doi.org/10.1359/jbmr.1999.14.6.960
Peichl P, Holzer LA, Maier R, Holzer G (2011) Parathyroid hormone 1–84 accelerates fracture-healing in pubic bones of elderly osteoporotic women. J Bone Joint Surg Am 93:1583–1587. https://doi.org/10.2106/JBJS.J.01379
Greenspan SL, Bone HG, Ettinger MP, Hanley DA, Lindsay R, Zanchetta JR, Blosch CM, Mathisen AL, Morris SA, Marriott TB, Treatment of osteoporosis with parathyroid hormone study group (2007) Effect of recombinant human parathyroid hormone (1–84) on vertebral fracture and bone mineral density in postmenopausal women with osteoporosis: a randomized trial. Ann Intern Med 146:326–339. https://doi.org/10.7326/0003-4819-146-5-200703060-00005
Nakamura T, Sugimoto T, Nakano T, Kishimoto H, Ito M, Fukunaga M, Hagino H, Sone T, Yoshikawa H, Nishizawa Y, Fujita T, Shiraki M (2012) Randomized teriparatide [human parathyroid hormone (PTH) 1–34] once-weekly efficacy research (TOWER) trial for examining the reduction in new vertebral fractures in subjects with primary osteoporosis and high fracture risk. J Clin Endocrinol Metab 97:3097–3106. https://doi.org/10.1210/jc.2011-3479
Ito M, Oishi R, Fukunaga M, Sone T, Sugimoto T, Shiraki M, Nishizawa Y, Nakamura T (2014) The effects of once-weekly teriparatide on hip structure and biomechanical properties assessed by CT. Osteoporos Int 25:1163–1172. https://doi.org/10.1007/s00198-013-2596-y
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mitlak BH (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441. https://doi.org/10.1056/NEJM200105103441904
Yamane H, Takakura A, Shimadzu Y, Kodama T, Lee JW, Isogai Y, Ishizuya T, Takao-Kawabata R, Iimura T (2017) Acute development of cortical porosity and endosteal naïve bone formation from the daily but not weekly short-term administration of PTH in rabbit. PLoS ONE 12:e0175329. https://doi.org/10.1371/journal.pone.0175329
Adachi JD, Hanley DA, Lorraine JK, Yu M (2007) Assessing compliance, acceptance, and tolerability of teriparatide in patients with osteoporosis who fractured while on antiresorptive treatment or were intolerant to previous antiresorptive treatment: an 18-month, multicenter, open-label, prospective study. Clin Ther 29:2055–2067. https://doi.org/10.1016/j.clinthera.2007.09.024
Usui T, Funagoshi M, Seto K, Ide K, Tanaka S, Kawakami K (2018) Persistence of and switches from teriparatide treatment among women and men with osteoporosis in the real world: a claims database analysis. Arch Osteoporos 13:54. https://doi.org/10.1007/s11657-018-0466-0
Sugimoto T, Shiraki M, Fukunaga M, Kishimoto H, Hagino H, Sone T, Nakano T, Ito M, Yoshikawa H, Minamida T, Tsuruya Y, Nakamura T (2019) Study of twice-weekly injections of teriparatide by comparing efficacy with once-weekly injections in osteoporosis patients: the TWICE study. Osteoporos Int 30:2321–2331. https://doi.org/10.1007/s00198-019-05111-6
Fauci AS, Lane HC, Redfield RR (2020) Covid-19 navigating the uncharted. N Engl J Med 382:1268–1269. https://doi.org/10.1056/NEJMe2002387
Marcus R, Wang O, Satterwhite J, Mitlak B (2003) The skeletal response to teriparatide is largely independent of age, initial bone mineral density, and prevalent vertebral fractures in postmenopausal women with osteoporosis. J Bone Miner Res 18:18–23. https://doi.org/10.1359/jbmr.2003.18.1.18
Shiraki M, Kuroda T, Miyakawa N, Fujinawa N, Tanzawa K et al (2011) Design of a pragmatic approach to evaluate the effectiveness of concurrent treatment for the prevention of osteoporotic fractures: rationale, aims and organization of a Japanese osteoporosis intervention trial (JOINT) initiated by the research group of adequate treatment of osteoporosis (A-TOP). J Bone Miner Metab 29:37–43. https://doi.org/10.1007/s00774-010-0188-x
Gallagher JC, Genant HK, Crans GG, Vargas SJ, Krege JH (2005) Teriparatide reduces the fracture risk associated with increasing number and severity of osteoporotic fractures. J Clin Endocrinol Metab 90:1583–1587. https://doi.org/10.1210/jc.2004-0826
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148. https://doi.org/10.1002/jbmr.5650080915
Asahi Kasei Pharma Corporation (2021) Self-injection instruction manual for Teribone 28.2-µg subcutaneous autoinjector (in Japanese). https://static.akp-pharma-digital.com/article_objects/2021/06/30/08d784fee078.pdf. Accessed 12 Jan 2022
Ranhoff AH, Laake K (1993) The Barthel ADL index: scoring by the physician from patient interview is not reliable. Age Ageing 22:171–174. https://doi.org/10.1093/ageing/22.3.171
Watanabe S, Iida Y, Ito T, Mizutani M, Morita Y, Suzuki S, Nishida O (2018) Effect of early rehabilitation activity time on critically Ill patients with intensive care unit-acquired weakness: a Japanese retrospective multicenter study. Prog Rehabil Med 3:20180003. https://doi.org/10.2490/prm.20180003
Rajzbaum G, Grados F, Evans D, Liu-Leage S, Petto H, Augendre-Ferrante B (2014) Treatment persistence and changes in fracture risk, back pain, and quality of life amongst patients treated with teriparatide in routine clinical care in France: results from the European forsteo observational study. Joint Bone Spine 81:69–75. https://doi.org/10.1016/j.jbspin.2013.05.001
Kyvernitakis I, Kostev K, Kurth A, Albert US, Hadji P (2014) Differences in persistency with teriparatide in patients with osteoporosis according to gender and health care provider. Osteoporos Int 25:2721–2728. https://doi.org/10.1007/s00198-014-2810-6
Foster SA, Foley KA, Meadows ES, Johnston JA, Wang SS, Pohl GM, Long SR (2011) Adherence and persistence with teriparatide among patients with commercial, medicare, and medicaid insurance. Osteoporos Int 22:551–557. https://doi.org/10.1007/s00198-010-1297-z
Ziller V, Zimmermann SP, Kalder M, Ziller M, Seker-Pektas B, Hellmeyer L, Hadji P (2010) Adherence and persistence in patients with severe osteoporosis treated with teriparatide. Curr Med Res Opin 26:675–681. https://doi.org/10.1185/03007990903538409
Arden NK, Earl S, Fisher DJ, Cooper C, Carruthers S, Goater M (2006) Persistence with teriparatide in patients with osteoporosis: the UK experience. Osteoporos Int 17:1626–1629. https://doi.org/10.1007/s00198-006-0171-5
Fujimori K, Sakurazawa K, Nakafuji S (2019) Analysis of the persistence and compliance of medications for osteoporosis using E-claim database (in Japanese). J Jpn Osteoporos Soc 5:69–77 ((in Japanese))
Tsuchie H, Miyakoshi N, Kasukawa Y, Abe H, Masutani N, Shimada Y (2020) Factors affecting continuation of weekly teriparatide administration in rural areas. J Bone Miner Metab 38:248–253. https://doi.org/10.1007/s00774-019-01051-7
Mok LL, Nickols GA, Thompson JC, Cooper CW (1989) Parathyroid hormone as a smooth muscle relaxant. Endocr Rev 10:420–436. https://doi.org/10.1210/edrv-10-4-420
Omura F (2016) Decrease of blood pressure after once-weekly teriparatide administration and the prevention (in Japanese). J New Rem Clin 65:20–33
Michalska D, Luchavova M, Zikan V, Raska I, Kubena AA, Stepan JJ (2012) Effects of morning vs. evening teriparatide injection on bone mineral density and bone turnover markers in postmenopausal osteoporosis. Osteoporos Int 23:2885–2891. https://doi.org/10.1007/s00198-012-1955-4
Vik SA, Jantzi M, Poss J, Hirdes J, Hanley DA, Hogan DB, Maxwell CJ (2007) Factors associated with pharmacologic treatment of osteoporosis in an older home care population. J Gerontol A Biol Sci Med Sci 62:872–878. https://doi.org/10.1093/gerona/62.8.872
Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R (2007) Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer 110:1860–1867. https://doi.org/10.1002/cncr.22991
Moriwaki K, Noto S (2017) Economic evaluation of osteoporosis liaison service for secondary fracture prevention in postmenopausal osteoporosis patients with previous hip fracture in Japan. Osteoporos Int 28:621–632. https://doi.org/10.1007/s00198-016-3777-2
Acknowledgements
None
Author information
Authors and Affiliations
Contributions
RF: conceptualization, methodology, formal analysis, investigation, and writing—original draft. TE and MT: writing—review and editing, and supervision. KH: investigation and writing—review and editing. HS: investigation and writing—review and editing. IO: investigation and writing—review and editing. MK: investigation and writing—review and editing. TA: investigation and writing—review and editing. KS: investigation and writing—review and editing. KY: investigation and writing—review and editing. AI: investigation and writing—review and editing. Hirohito Takeuchi: formal analysis and writing—review and editing. HO: formal analysis and writing—review and editing. NI: writing, review, and editing.
Corresponding author
Ethics declarations
Conflicts of interest
All authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Fujita, R., Endo, T., Takahata, M. et al. Real-world persistence of twice-weekly teriparatide and factors associated with the discontinuation in patients with osteoporosis. J Bone Miner Metab 40, 782–789 (2022). https://doi.org/10.1007/s00774-022-01347-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-022-01347-1