Abstract
Guanidino compounds such as dimethylarginines (SDMA, ADMA) and L-homoarginine ((L-)hArg) can interfere with bioavailability and function of the main NO-donor L-arginine (L-Arg). High ADMA and SDMA but low L-hArg concentrations have been associated with cardio- and cerebrovascular events and mortality in adults. The role of guanidino compounds in paediatric patients remains less clear. We, therefore, compared guanidino compound levels in plasma samples of 57 individuals with chronic kidney disease (CKD) and 141 individuals without CKD from the age of 0 to 17 years, including patients with different comorbidities by correlation and regression analyses. We found highest hArg, SDMA and ADMA concentrations in neonates (Kruskal–Wallis, p < 0.001 for all). From the age of 1 year on, hArg levels increased, whereas SDMA und ADMA levels further decreased in children. SDMA and ADMA are higher in children with CKD independent of GFR (mean factor 1.92 and 1.38, respectively, p < 0.001 for both), and SDMA is strongly correlated with creatinine concentration in children with CKD (Spearman’s rho 0.74, p < 0.001). We provide guanidino compound levels in a large sample covering all paediatric age groups for the first time. Our data can be used to assess the role of guanidino compounds such as hArg in disease states, i.e. cerebro- and cardiovascular disorders in childhood and adolescence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nitric oxide (NO) functions as potent vasorelaxant, inhibitor of platelet aggregation and neurotransmitter. The main substrate for NO synthase is L-arginine (L-Arg) which results from the urea cycle in the kidney. Guanidino compounds with structural similarity can alter L-Arg bioavailability. Among guanidino compounds, asymmetric dimethylarginine (ADMA), symmetric dimethylarginine (SDMA) and L-homoarginine (L-hArg) have emerged as potential modulators of NO metabolism. Whereas ADMA serves as endogenous NO inhibitor, SDMA inhibits cellular L-Arg uptake, and L-hArg may act as substrate for NO synthetase and increase L-Arg bioavailability by inhibiting arginase (Grosse et al. 2020).
High ADMA and SDMA, but low L-hArg concentrations have been associated with cardio- and cerebrovascular events and mortality (Wanby et al. 2006; Pilz et al. 2011; Grosse et al. 2020). In both population-based and clinical cohorts, ADMA and SDMA concentrations are correlated with cardiovascular risk burden, e.g. CHA2DS2-VASC (Cordts et al. 2019; Grosse et al. 2019). Furthermore, patients with acute ischaemic stroke or myocardial infarction have higher ADMA and SDMA concentrations compared with healthy controls (Schulze 2010, Lüneburg 2012, Jud 2018). Lower L-hArg concentrations are associated with increased adverse events after stroke or cardiovascular events (März et al. 2010; Atzler et al. 2015). Moreover, a causative role for L-hArg in stroke has been demonstrated in mouse models lacking endogenous L-hArg synthesis by arginine:glycine amidinotransferase (AGAT) (Choe et al. 2013).
In addition to cardiovascular function and disease, numerous studies have linked these three guanidino compounds with kidney function. High SDMA and low L-hArg concentrations have been repeatedly shown to correlate with glomerular filtration rate (GFR) (Brooks et al. 2009; Schwedhelm and Böger 2011; Snauwaert et al. 2018a). Especially SDMA is a reliable blood-based marker for early kidney impairment in humans and animals (Schwedhelm and Böger 2011). In adults, L-hArg levels decrease with age, whereas ADMA and SDMA levels increase (Atzler et al. 2014). Of note, in children and adolescents, ADMA concentrations were found to decrease with age, whereas no clear correlation of SDMA with age has been observed (Lücke et al. 2007; Jaźwińska-Kozuba et al. 2013). On the other hand, L-hArg increases from 3 to 18 years of age (Jaźwińska-Kozuba et al. 2013). Interestingly, L-hArg levels also increase during pregnancy from first to third trimester and correlate with flow-dilated vasodilatation (FMD) (Valtonen et al. 2008). However, concentrations of hArg, SDMA and ADMA and their precursors have not been measured systematically in larger cohorts of children younger than 3 years. Given the complex role of guanidino compounds in NO metabolism and cardiovascular disorders, we examined the concentrations of hArg, SDMA and ADMA in neonates, children and adolescents including paediatric patients with chronic kidney disease (CKD).
Methods
Study design, ethical approval and patient consent
This study is a cross-sectional single-centre cohort at the department of paediatrics at the University Medical Center Hamburg-Eppendorf. 141 patients without evidence of impaired renal function and cardio- or cerebrovascular disorder were classified according to their age into 5 subgroups (0–28 days; 1–11 months; 1–6 years; 7–12 years; 13–17 years). Creatinine concentrations were measured in 123 of 141 patients (creatinine levels were not routinely measured in healthy newborns). In addition, 57 paediatric patients with chronic kidney disease (CKD) were included into a separate cohort. GFR was calculated using the Schwarz formula (Schwartz et al. 1976).
The study protocol was approved by the Ethics Committee of the Hamburg Board of Physicians (PV5279). The investigation was conducted in accordance with the Declaration of Helsinki.
Laboratory measurements
The laboratory measurements of guanidino compounds were obtained from blood samples stored at − 80 °C, and processed as previously described with minor modifications (Atzler et al. 2011; Cordts et al. 2015). In brief, 25 μl of EDTA plasma, calibrator or quality control sample was subjected to protein precipitation with 100 μl methanol containing stable isotope-labelled internal standards. Residues were derivatised to their butyl ester derivatives and reconstituted samples were separated on an AQUITY UPLC BEH C18 1.7 µm (2.1 × 50 mm) column (Waters, Eschborn, Germany) using an elution gradient of the two mobile phases (A) 0.1% formic acid in water and (B) 0.1% formic acid in acetonitrile at a flow rate of 0.4 mL/min over 2.6 min. Quantification was performed with a Xevo Triple Quadrupole Mass Spectrometer (Waters) with positive electrospray ionisation in the multiple reaction mode (MRM). Peak area ratios of analyte and internal standard were calculated for calibration (four levels), quality control (QC-low and -high), and study samples and used for quantification. Quality control samples were accepted below 15% relative standard deviation (RSD).
Statistical analysis
Continuous variables are given as mean ± standard deviation (SD) if normally distributed, otherwise as median [25th–75th percentiles], and categorical variables are given as numbers (percentage) of participants. Relationships with continuous variables were assessed by Spearman correlation. Statistical comparisons of age groups were made by Kruskal–Wallis with Bonferroni post hoc test or Chi2 test as appropriate. For statistical comparisons of control children and children with CKD, we used Mann–Whitney U test. The independent association between control and CKD patients with hArg, SDMA and ADMA was determined by multivariable linear regression analyses (mean factor and 95% confidence interval, CI). For unadjusted and adjusted linear regression analyses, we calculated beta coefficients for different models: unadjusted (model 1), adjusted for age and weight (model 2), and adjusted for age, weight and GFR (model 3). A p value < 0.05 was considered statistically significant. Statistical analysis was performed with IBM SPSS Statistics (version 22, IBM Corp., Armonk, NY) and GraphPad Prism (version 5 for Windows, La Jolla, USA).
Data availability statement
Deidentified patient data, related documents such as study protocol and statistical analysis plan will be shared by request from any qualified investigator for 3 years after the date of publication.
Results
In our baseline cohort, 141 children and adolescents across age groups 1–5 without CKD or evidence of cerebro- or cardiovascular disorder were included (Table 1). Comparison between age groups revealed significant differences for haemoglobin, creatinine, GFR, L-Arg, citrulline, ornithine, hArg, SDMA and ADMA concentrations (Table 1). In post hoc analysis, neonates (age group 1, i.e. neonates < 29 days) had lower L-Arg and citrulline, but higher ornithine, hArg, SDMA and ADMA plasma levels compared with age groups 3–5, i.e. 1 year and older (Fig. 1). ADMA and SDMA plasma levels were also higher in children of age group 2 (1–11 months) compared with older age groups, whereas hArg dropped from high levels in age group 1 and then gradually increased from age group 2–5 (Fig. 1).
Given the obvious difference of metabolite kinetics in neonates, we analysed age groups 2–5 separately from age group 1. In children of age groups 2–5, age and creatinine were positively associated with hArg, whereas ADMA and SDMA showed a negative correlation (Table 2). hArg, SDMA and ADMA were positively correlated with ornithine levels (Table 2). Similarly, positive correlations were found for hArg and ADMA with L-Arg and L-lysine, whereas only hArg revealed a positive association with L-citrulline (Table 2). In contrast, hArg and SDMA concentrations strongly and negatively decreased with age in neonates. This is in accordance with high maternal hArg levels during late pregnancy (Table 3) (Valtonen et al. 2008).
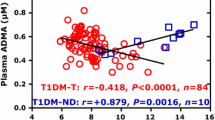
We compared 123 children with normal renal function and 57 children with CKD. As expected, children with CKD had lower haemoglobin and higher creatinine plasma levels. In addition, L-citrulline, SDMA and ADMA plasma levels were increased compared with control children (Table 4). In linear regression analysis, SDMA and ADMA levels were 1.92-fold and 1.38-fold higher in CKD compared with control children in models also adjusted for age, weight, and GFR (Table 5). Consistently, ADMA and SDMA were negatively and hArg was positively correlated with age in CKD children (Table 6). A positive correlation was also found for ADMA and SDMA with citrulline (Table 6). Interestingly, only SDMA levels were correlated with creatinine concentrations in CKD children, whereas hArg and ADMA were not (Table 6).
Other factors than CKD have also been shown to interfere with guanidino compound metabolism (Hanusch et al. 2020). We, therefore, analysed the effects of either inflammatory disorders, immunosuppressive medication or vitamin D supplementation on guanidino compound levels in our control cohort (Table 7). Vitamin D supplementation had no significant effect on SMDA, ADMA and hArg plasma levels. Both inflammatory disorders and immunosuppressive medication, however, were associated with lower SDMA levels, but not with altered hArg or ADMA levels.
Discussion
In this study, we provide the first dataset of guanidino compound levels including all paediatric age groups including neonates as well as children with CKD. Our main findings are that (1) neonates have higher hArg, SDMA and ADMA plasma concentrations compared with children older than 12 months, (2) hArg levels increase, whereas SDMA und ADMA levels decrease in children from the age of 2 months on, (3) SDMA and ADMA are higher in children with CKD independent of GFR and (4) only SDMA but not ADMA and hArg are strongly correlated with creatinine concentration children with in CKD.
To date, there are no reference values available for guanidino compounds in individuals younger than 18 years. Several studies have reported guanidino compound levels including L-hArg, ADMA and SDMA in paediatric healthy control subjects. To our knowledge, the largest cohort consisted in 78 children from the age of 5–17 years (Hanusch et al. 2020). Other studies included younger children but smaller overall numbers (Snauwaert et al. 2018a). However, guanidino compound levels especially in neonates have not been analysed before. Our control cohort includes 141 subjects of distinct paediatric age groups including neonates which allows us to identify correlations of guanidino compound levels with different parameters such as age and precursor metabolite concentrations. Our results are in the same range as previously published average concentrations for the relevant guanidino metabolites L-Arg (44–93 µmol/l) (Buck et al. 2017; Hanusch et al. 2020), L-hArg (1.2–1.8 µmol/l) (Hörster et al. 2015; Hanusch et al. 2022), SDMA (0.4–0.7 µmol/l) (Brooks et al. 2009; Andrade et al. 2015), and ADMA (0.6–0.9 µmol/l) (Langen et al. 2015; Buck et al. 2017) in children and adolescents.
In neonates, hArg and SDMA levels steadily decreased during the first 28 days after birth. In our cohort, hArg levels in neonates were 3.06 [1.19, 5.42] µmol/l and therefore much higher than in children and adolescents. Interestingly, Valtonen and colleagues have shown that L-hArg concentrations are significantly increased during the second and third trimester in pregnant women reaching concentrations up to 5 µmol/l (Valtonen et al. 2008). Therefore, high hArg concentrations in neonates are likely not due to endogenous synthesis in neonates but result from elevated maternal hArg. Given that hArg levels continuously increase from age group 2 with median levels of 0.8 µmol/l to age group 5 with median levels of 1.57 µmol/l, endogenous production seems to be low in early development and does steadily evolve during childhood. In accordance, a previous study in children and adolescents revealed increasing L-hArg in the age range of 3–18 years (Jaźwińska-Kozuba et al. 2013).
SDMA and ADMA both result from protein degradation by N-methyl protein transferases. Similar to hArg, SDMA levels drop during the first weeks of life from elevated levels to a baseline around 0,4 µmol/l and do not increase again during childhood and adolescence. SMDA is excreted almost exclusively via the kidney, and high SDMA levels in early development might either indicate low renal filtration rate in newborns, increased protein degradation or exogenous supply during pregnancy. In a similar but less pronounced fashion, ADMA concentrations decline from slightly elevated levels after birth to around 0,5 µmol/l in infancy, but continuously decrease during childhood and adolescence. ADMA is metabolised in liver and kidney, and excreted via the kidney to a smaller extent (Chen et al. 2012). ADMA levels, thus, might also mirror protein turnover which is high during periods of rapid growth during early development and steadily declines during development.
The high levels of all three guanidino compounds ADMA, SDMA and hArg in neonates are puzzling, and the physiological consequences are not entirely clear. ADMA and SDMA are negatively correlated with cardiac function and circulation in adults (Wanby et al. 2006; Grosse et al. 2020). hArg, on the other hand, exerts positive effects on cardiac and vascular function as well as overall mortality (Atzler et al. 2017; Faller et al. 2018; Rodionov et al. 2019; Schwedhelm et al. 2020). Following low endogenous L-hArg production due to immature renal synthesis in the developing foetus and neonates, maternal supply of high levels of L-hArg might thus be protective to counterbalance excessive SDMA/ADMA levels during this early developmental period.
Guanidino compounds are in part synthetised and excreted via the kidney. Consequently, the levels of ADMA, SDMA and L-hArg have been shown to be correlated with renal function in adults (Drechsler et al. 2013; Tomaschitz et al. 2014; Snauwaert et al. 2018a). Similar results have been published for SDMA and ADMA in paediatric patients suffering from CKD, but L-hArg levels have not been previously analysed in detail (Brooks et al. 2009; Snauwaert et al. 2018a, b). In accordance with previous studies, our data confirm the strong correlation of SDMA and to a lesser extent ADMA with renal function. Especially SDMA has been proposed as a sensitive surrogate marker for GFR (Schwedhelm and Böger 2011). Our data demonstrate a strong age dependence during the first months which might limit its use during this age group. However, we did not analyse the correlation of SDMA and GFR in newborns and toddlers in detail. With regard to hArg, we only found a trend, but not a clear correlation between plasma concentrations and CKD possibly due to the relatively preserved renal function in our CKD group and small number of individuals.
In paediatric patients, guanidino compounds have previously been analysed in a number of conditions such as growth retardation, airway inflammation, atopic diseases or muscular dystrophy (Hörster et al. 2015; Langen et al. 2015; Hanusch et al. 2020, 2022). Elevated L-hArg levels have been found in short stature children, for example (Langen et al. 2015). Minor alterations in the Arg/NO pathway have been described in patients with inflammatory diseases such as cystic fibrosis, but antibiotic treatment led to a significant reduction in local L-hArg in sputum (Hanusch et al. 2022). In addition, chronic treatment with steroids did not affect guanidino compound levels in a cohort of Duchenne patients (Hörster et al. 2015). In our sample, we detected reduced SDMA levels in both inflammatory disorders and immunosuppressive treatment, whereas ADMA and hArg plasma levels remained unaffected. As SDMA is produced by N-methyl protein transferases during protein degradation, decreased levels following acute antibiotic treatment might reflect reduction in protein turnover. Reduced SDMA levels under immunosuppressive medication in our cohort of patients might also be explained by reduced protein turnover. The reason for lower SDMA levels in inflammatory disorders, however, remains unclear.
In summary, we provide guanidino compound levels of all paediatric age groups in a relatively large clinical sample. We show for the first time that hArg and SDMA plasma concentrations are highest in neonates compared with older children. Furthermore, our data confirm that SDMA is a valuable marker to distinguish and quantify CKD in children. Our data can be used to assess the role of guanidino compounds such as hArg in other disease states in the future, i.e. in cerebro- and cardiovascular disorders during childhood and adolescence.
Data availability
Data generated during this study are available from the corresponding author on request.
Abbreviations
- ADMA:
-
Asymmetric dimethylarginine
- CKD:
-
Chronic kidney disease
- GFR:
-
Glomerular filtration rate
- L-Arg:
-
L-Arginine
- hArg:
-
Homoarginine
- SDMA:
-
Symmetric dimethylarginine
References
Andrade F, Llarena M, Lage S, Aldámiz-Echevarría L (2015) Quantification of arginine and its methylated derivatives in healthy children by liquid chromatography-tandem mass spectrometry. J Chromatogr Sci 53:787–792. https://doi.org/10.1093/chromsci/bmu126
Atzler D, Mieth M, Mass R et al (2011) Stable isotope dilution assay for liquid chromatography-tandem mass spectrometric determination of L-homarginine in human plasma. J Chromatogr B 879:2294–2298
Atzler D, Schwedhelm E, Nauck M et al (2014) Serum reference intervals of homoarginine, ADMA, and SDMA in the Study of Health in Pomerania. Clin Chem Lab Med 52:1835–1842. https://doi.org/10.1515/cclm-2014-0314
Atzler D, Schwedhelm E, Choe C (2015) L-Homoarginine and cardiovascular disease. Curr Opin Clin Nutr Metab Care 18:83–88. https://doi.org/10.1097/MCO.0000000000000123
Atzler D, Mcandrew DJ, Cordts K et al (2017) Dietary supplementation with homoarginine preserves cardiac function in a murine model of post-myocardial infarction heart failure. Circulation 135:400–402. https://doi.org/10.1161/CIRCULATIONAHA.116.025673
Brooks ER, Langman CB, Wang S et al (2009) Methylated arginine derivatives in children and adolescents with chronic kidney disease. Pediatr Nephrol 24:129–134. https://doi.org/10.1007/s00467-008-0972-1
Buck A, Kayacelebi AA, Chobanyan-Jürgens K et al (2017) Comprehensive analysis of the l-arginine/l-homoarginine/nitric oxide pathway in preterm neonates: potential roles for homoarginine and asymmetric dimethylarginine in foetal growth. Amino Acids 49:783–794. https://doi.org/10.1007/s00726-017-2382-9
Chen S, Li N, Deb-Chatterji M et al (2012) Asymmetric Dimethyarginine as marker and mediator in Ischemic stroke. Int J Mol Sci 13:15983–16004. https://doi.org/10.3390/ijms131215983
Choe CU, Atzler D, Wild PS et al (2013) Homoarginine levels are regulated by l-arginine: Glycine amidinotransferase and affect stroke outcome: Results from human and murine studies. Circulation 128:1451–1461. https://doi.org/10.1161/CIRCULATIONAHA.112.000580
Cordts K, Atzler D, Qaderi V et al (2015) Measurement of homoarginine in human and mouse plasma by LC-MS/MS and ELISA: A comparison and a biological application. Amino Acids 47:2015–2022. https://doi.org/10.1007/s00726-015-2037-7
Cordts K, Grzybowski R, Lezius S et al (2019) Guanidino compound ratios are associated with stroke etiology, internal carotid artery stenosis and CHA2DS2-VASc score in three cross-sectional studies. J Neurol Sci 397:156–161. https://doi.org/10.1016/j.jns.2018.12.037
Drechsler C, Kollerits B, Meinitzer A et al (2013) Homoarginine and Progression of Chronic Kidney Disease: Results from the Mild to Moderate Kidney Disease Study. PLoS ONE 8:4–9. https://doi.org/10.1371/journal.pone.0063560
Faller KME, Atzler D, McAndrew DJ et al (2018) Impaired cardiac contractile function in arginine:glycine amidinotransferase knockout mice devoid of creatine is rescued by homoarginine but not creatine. Cardiovasc Res 114:417–430. https://doi.org/10.1093/cvr/cvx242
Grosse GM, Biber S, Sieweke JT et al (2019) Plasma dimethylarginine levels and carotid intima–media thickness are related to atrial fibrillation in patients with embolic stroke. Int J Mol Sci 20:1–13. https://doi.org/10.3390/ijms20030730
Grosse GM, Schwedhelm E, Worthmann H, Choe CU (2020) Arginine derivatives in cerebrovascular diseases: mechanisms and clinical implications. Int J Mol Sci. https://doi.org/10.3390/ijms21051798
Hanusch B, Brinkmann F, Mayorandan S et al (2020) Local and systemic alterations of the l-arginine/nitric oxide pathway in sputum, blood, and urine of pediatric cystic fibrosis patients and effects of antibiotic treatment. J Clin Med 9:1–19. https://doi.org/10.3390/jcm9123802
Hanusch B, Sinningen K, Brinkmann F et al (2022) Characterization of the L-Arginine/Nitric Oxide Pathway and Oxidative Stress in Pediatric Patients with Atopic Diseases. Int J Mol Sci. https://doi.org/10.3390/ijms23042136
Hörster I, Weigt-Usinger K, Carmann C et al (2015) The l-arginine/NO pathway and homoarginine are altered in Duchenne muscular dystrophy and improved by glucocorticoids. Amino Acids 47:1853–1863. https://doi.org/10.1007/s00726-015-2018-x
Jaźwińska-Kozuba A, Martens-Lobenhoffer J, Kruszelnicka O et al (2013) Opposite associations of plasma homoarginine and ornithine with arginine in healthy children and adolescents. Int J Mol Sci 14:21819–21832. https://doi.org/10.3390/ijms141121819
Jud P, Hafner F, Verheyen N et al (2018) Homoarginine/ADMA ratio and homoarginine/SDMA ratio as independent predictors of cardiovascular mortality and cardiovascular events in lower extremity arterial disease. Sci Rep 8:1–7. https://doi.org/10.1038/s41598-018-32607-8
Langen J, Kayacelebi AA, Beckmann B et al (2015) Homoarginine (hArg) and asymmetric dimethylarginine (ADMA) in short stature children without and with growth hormone deficiency: hArg and ADMA are involved differently in growth in the childhood. Amino Acids 47:1875–1883. https://doi.org/10.1007/s00726-015-2028-8
Lücke T, Kanzelmeyer N, Kemper MJ et al (2007) Developmental changes in the L-arginine/nitric oxide pathway from infancy to adulthood: Plasma asymmetric dimethylarginine levels decrease with age. Clin Chem Lab Med 45:1525–1530. https://doi.org/10.1515/CCLM.2007.300
Lüneburg N, von Holten RA, Töpper RF et al (2012) Symmetric dimethylarginine is a marker of detrimental outcome in the acute phase after ischaemic stroke: Role of renal function. Clin Sci 122:105–111. https://doi.org/10.1042/CS20110013
März W, Meinitzer A, Drechsler C et al (2010) Homoarginine, Cardiovascular Risk, and Mortalitiy. Circulation 122:967–975
Pilz S, Tomaschitz A, Meinitzer A et al (2011) Low serum homoarginine is a novel risk factor for fatal strokes in patients undergoing coronary angiography. Stroke 42:1132–1134. https://doi.org/10.1161/STROKEAHA.110.603035
Rodionov RN, Begmatov H, Jarzebska N et al (2019) Homoarginine Supplementation Prevents Left Ventricular Dilatation and Preserves Systolic Function in a Model of Coronary Artery Disease. J Am Heart Assoc 8:1–12. https://doi.org/10.1161/JAHA.119.012486
Schulze F, Carter AM, Schwedhelm E et al (2010) Symmetric dimethylarginine predicts all-cause mortalitiy following ischemic stroke. Atherosclerosis 208:518–523
Schwartz GJ, Haycock GB, Edelmann CM, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Schwedhelm E, Böger RH (2011) The role of asymmetric and symmetric dimethylarginines in renal disease. Nat Rev Nephrol 7:275–285. https://doi.org/10.1038/nrneph.2011.31
Schwedhelm E, Song RJ, Vasan RS et al (2020) Association of lower plasma homoarginine concentrations with greater risk of all-cause mortality in the community: The framingham offspring study. J Clin Med 9:1–10. https://doi.org/10.3390/JCM9062016
Snauwaert E, Van Biesen W, Raes A et al (2018a) Concentrations of representative uraemic toxins in a healthy versus non-dialysis chronic kidney disease paediatric population. Nephrol Dial Transplant 33:978–986. https://doi.org/10.1093/ndt/gfx224
Snauwaert E, Van Biesen W, Raes A et al (2018b) Accumulation of uraemic toxins is reflected only partially by estimated GFR in paediatric patients with chronic kidney disease. Pediatr Nephrol 33:315–323. https://doi.org/10.1007/s00467-017-3802-5
Tomaschitz A, Meinitzer A, Pilz S et al (2014) Homoarginine, kidney function and cardiovascular mortality risk. Nephrol Dial Transplant 29:663–671. https://doi.org/10.1093/ndt/gft512
Valtonen P, Laitinen T, Lyyra-Laitinen T et al (2008) Serum L-Homoarginine Concentration is Elevated During Normal Pregnancy and is Related to Flow-Mediated Vasodilatation. Circ J 72:1879–1884. https://doi.org/10.1253/circj.cj-08-0240
Wanby P, Teerlink T, Brudin L et al (2006) Asymmetric dimethylarginine (ADMA) as a risk marker for stroke and TIA in a Swedish population. Atherosclerosis 185:271–277
Funding
Open Access funding enabled and organized by Projekt DEAL. Dr. Choe was supported by an Else Kröner Exzellenzstipendium from the Else Kröner-Fresenius Stiftung (grant number: 2018_EKES.04).
Author information
Authors and Affiliations
Contributions
ES, CC and AN contributed to study concept and design. Sample collection and analysis was performed by FB, BM, ES and AN. Statistical analysis was performed by CC and SL. All authors contributed to manuscript preparation. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related to this study.
Additional information
Handling editor: S. Gross.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baach, F., Meyer, B., Oh, J. et al. Developmental dynamics of homoarginine, ADMA and SDMA plasma levels from birth to adolescence. Amino Acids 55, 1381–1388 (2023). https://doi.org/10.1007/s00726-023-03318-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-023-03318-w