Abstract
It has previously been shown that immune complexes (IC) of a given biomarker with class M immunoglobulins (IgM) provide better performances compared to the unbound biomarker in a number of cancer entities. In the present work, we investigated IC of IgM-Aβ as a potential biomarker for Alzheimer’s disease (AD). Aβ–IgM concentration has been measured in 75 plasma samples from patients with AD, individuals with mild cognitive impairment (MCI), and healthy age- and sex-matched controls (HC). To characterize the fractions associated with Aβ, pooled plasma samples were subjected to gel-filtration analysis. Size-separated fractions were analyzed for the presence of Aβ using a sandwich ELISA assay. A strong reactivity was observed in the high molecular weight IgM (>500 kDa) and 150 kDa (IgG) fractions indicating that blood Aβ is strongly associated with antibodies. Using an ELISA assay detecting Aβ–IgM complexes, we observed that high levels of Aβ–IgMs were detectable in HC and MCI patients; however, there was no significant difference to the AD group.
Similar content being viewed by others
Introduction
The earliest pathological events leading to Alzheimer’s disease (AD) are estimated to occur 10–20 years before the appearance of the first cognitive changes in affected patients (Price and Morris 1999; Yamaguchi et al. 2001). Therefore, identification of biomarkers predictive for AD might allow screening for individuals who may benefit from preventive therapies before the development of cognitive impairment. The Aβ42 peptide is supposed to have a central role in the pathogenesis of AD (Hardy and Selkoe 2002), and its measurement in the cerebrospinal fluid (CSF) became nowadays a routine diagnostic procedure with 75–95% sensitivity and specificity (Blennow 2004; Jensen et al. 1999; Lewczuk et al. 2004). Unfortunately, CSF and blood levels of Aβ do not correlate, neither in AD patients (Mehta et al. 2001) nor in healthy controls (Mehta and Pirttila 2005). On the other side, it has been also shown that there is a correlation between CSF and plasma levels of Aβ40 and Aβ42 in healthy individuals, whereas no such correlation could be seen for AD or MCI cases (Giedraitis et al. 2007).
Studies on plasma Aβ levels have shown contradictory results, ranging from increased Aβ40 and decreased Aβ42 in AD patients compared to healthy controls (Xu and Gaskin 2008), no differences (Fukumoto et al. 2003; Vanderstichele et al. 2000) or increased Aβ42 in AD patients (Matsubara et al. 1999). The different findings in these studies may be due to differences in study designs, including variations in age and disease severity of included subjects. A longitudinal study showed that plasma Aβ40 and Aβ42 levels measured at age 70 years were not significantly associated with incident AD (Sundelof et al. 2008). All of the studies though, have shown substantial overlap in plasma Aβ40 and Aβ42 levels between patients and controls, thus limiting the diagnostic value of plasma Aβ assessment. Although the significance of Aβ for diagnosing Alzheimer’s disease is controversial, high plasma concentrations of Aβ40 and low plasma concentrations of Aβ42 indicate an increased risk of dementia (reviewed in Kawarabayashi and Shoji 2008). Nonetheless, analysis of plasma instead of CSF would be highly desirable because of its better accessibility and less invasive sampling procedure. Plasma Aβ levels are commonly quantified with enzyme-linked immunoabsorbent assays (ELISA) using antibodies against a variety of Aβ epitopes (for example Mehta et al. 2000; Suzuki et al. 1994). Quantification of Aβ in blood is technically difficult and limited by the fact that most of it is bound to blood components, including lipids serum albumin, α2-macroglobulin, immunoglobulins, apolipoprotein J, transthyritin, apoferritin, as well as complement components C1q and C3 (Biere et al. 1996; Kuo et al. 2000).
Besides the detection of biochemical AD markers, autoimmune responses to molecules specific to AD pathology have become a current research focus (Gruden et al. 2004; Nath et al. 2003). There seems to be a reduction in the magnitude of lymphocyte stimulation by APP in AD patients (Trieb et al. 1996), and naturally occurring anti-Aβ antibodies seem to be present in sera and CSF of AD patients and healthy controls (Du et al. 2001). However, whether autoimmunity plays a direct role in the pathogenesis of AD is still open to debate (McGeer and McGeer 2001; Singh 1997; Tarkowski et al. 2003).
In the present study, the level of circulating immune complexes (ICs) between Aβ and class M immunoglobulins (IgM) has been investigated, because ICs have been shown to be relevant biomarkers for different types of cancers (Beneduce et al. 2005, 2006; Castaldi et al. 2005), showing an improved diagnostic power compared to the free biomarker protein.
Materials and methods
Patients and samples
Plasma samples (stored at −70°C) from 30 out-patients with mild to moderate AD, 15 patients with mild cognitive impairment (MCI) and 30 healthy controls (HC) were analyzed. The patients were recruited at the Memory Clinic at the Department of Geriatrics, Uppsala University Hospital. All AD patients were diagnosed according to DSM IV (American Psychiatric Association 2000) and NINCDS-ADRDA (McKhann et al. 1984). The MCI patients met the Petersen criteria (Winblad et al. 2004) for MCI.
Gel filtration
Plasma samples from five AD patients and five healthy controls showing high reactivity to Aβ–IgM immune complexes in a preliminary assay were grouped and analyzed by gel-filtration HPLC. 500 µl of pooled samples were analyzed using a gel-filtration column Superdex 200 10/300 GL (GE Healthcare, Freiburg, Germany) on an ACTA Basic system (GE Healthcare, Freiburg, Germany). The elution was carried out in PBS at a flow rate of 1 ml per minute, and sample absorbance was monitored at 280 nm. Fractions were collected every 30 s, immunoreactivity was tested by ELISA and the fractions corresponding to the highest immunoreactivity were pooled and used as reference standard. Before running the samples, a calibration run was carried out according to the manufacturer’s instructions.
ELISA assay to detect Aβ
The Aβ level in gel-filtration fractions was determined as follows: 96-well ELISA plates were coated with 50 μl per well of 1 μg/ml of mouse anti-human Aβ antibody directed against residues 17-24 (4G8, Signet Laboratories, Dedham, MA, USA) in PBS at 4°C overnight and then blocked for 2 h with 3% BSA in PBS at 37°C. After blocking, 50 μl of gel-filtration fractions in PBS containing 1% BSA and 0.05% Tween 20 (PBS-B-T) were incubated for 1.5 h at 37°C. The wells were then washed with PBS containing 0.05% Tween 20 and incubated with 50 μl of rabbit polyclonal anti-Aβ 692 (generous gift from Gerd Multhaup, Free University of Berlin) at a 1:1,000 dilution in PBS-B-T for 1.5 h at 37°C. Aβ was revealed using peroxidase-conjugated goat anti-rabbit IgG (Dako, Glostrup, Denmark) in a 1:1,000 dilution in PBS-B-T and developed with TMB (Pierce manufacturing, Appleton, IL, USA) and hydrogen peroxide as substrate. The results of Aβ determination in the gel-filtration fractions were reported in optical density.
ELISA assay to detect Aβ–IgM immune complexes
96-well ELISA plates were coated with 50 μL per well of 1 μg/mL 4G8 antibody (Signet Laboratories, Dedham, MA, USA) in PBS at 4°C overnight and then blocked for 2 h with 3% BSA in PBS. After blocking, 50 μl of serially diluted reference standard or samples in PBS-B-T were incubated for 1.5 h at 37°C. The Aβ–IgM complex was revealed using peroxidase-conjugated anti-human IgM (Sigma-Aldrich, Munich, Germany) at a dilution of 1:3,000 in PBS-B-T and developed with TMB and hydrogen peroxide as the substrate. Aβ–IgM IC levels in the plasma were expressed in arbitrary units/ml (AU/ml) by using gel-filtration-purified Aβ–IgM reference standards to design a calibration curve, where the undiluted standard was assigned 1,000 AU/ml; concentration was determined by interpolation of samples absorbance on the calibration curve. The linear range of the assay was between 3.9 and 62.5 AU/ml. The samples with values above 62.5 AU/ml were further diluted and re-measured. The assay was standardized and its analytical performance evaluated: inter- and intra-assay coefficient of variation (CV) was less than 10%. Aβ–IgM cut-off was selected as the best combination of specificity and sensitivity according to the receiver-operating characteristic (ROC) curve.
Western blot
Gel-filtration fractions corresponding to 280 nm absorbance peaks were separated on a 4–12% variogel (Anamed, Groß-Bieberau, Germany) and then transferred to a nitrocellulose membrane. The membrane was heated in PBS in a microwave for 5 min and then blocked in 10% non-fat dry milk in TBS containing 0.05% Tween (TBS-T) for 1 h at room temperature. Blots were then incubated with peroxidase-conjugated goat anti-human IgM (Sigma-Aldrich) at 1:1,000 in TBS-T for 2 h or, alternatively, with a primary antibody directed against Aβ residues 4-10 (W0-2, The Genetics Company, Switzerland) overnight at 4°C and secondary peroxidase-conjugated antibodies for 2 h at room temperature. Protein bands were revealed using chemiluminescence solution and peroxide hydrogen as substrates on a Curix60 developing machine (Agfa-Gevaert N.V., Mortsel, Belgium).
Data analysis
All biomarker values were expressed as mean values ± standard deviation. Differences between the groups were determined by ANOVA followed by Student t tests. The diagnostic powers were determined by ROC curve analysis. Chi-square test on independence was used to analyze, if the gender distribution was significantly different between the three groups and if there is a difference between the two patient groups in relation to the number of family members with dementia. All analyses were performed using GraphPad Prism (GraphPad software, Inc., La Jolla, CA, USA and SPSS 16 for Windows). Significance level was α = 0.05. All tests were two-tailed.
Results
There were no significant age differences between the three groups [Alzheimer patients (AD), MCI and healthy controls] (F = 0.3, df = 2, 72; P = 0.74). Patients with MCI diagnosis were not significantly older at onset of the disease than AD patients (F = 2.3, df = 1, 42; P = 0.13). As expected, the mean MMSE score was higher in MCI compared to AD patients (F = 44.3, df = 1, 40; P < 0.0005). Gender distribution was not significantly different between the three groups (Chi² = 1.2, df = 2; P = 0.55) and the proportion of family members with dementia did not differ significantly between the two patients groups (Chi² = 0.8, df = 1; P = 0.38) (Table 1).
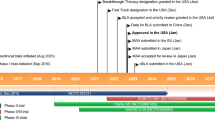
In order to identify circulating Aβ–IgM complexes, plasma samples from ten individuals were pooled and analyzed by gel filtration. Fractions collected from the column were tested for the presence of generic Aβ and Aβ–IgM complexes using ELISA assays. A strong immunoreactivity against Aβ was observed in the fraction eluting at high molecular weight (>500 kDa) (Fig. 1a). In the same fraction high reactivity for ICs of Aβ with IgM was also found, thus providing the first evidence of the occurrence of circulating Aβ–IgM complexes (Fig. 2c). Reactivity for generic Aβ was also found in the fractions eluting at 150 kDa (IgG fraction) and at low molecular weight (not shown). Reactivity against the monomeric form of Aβ has been found in all fractions, confirming previous observations (Kuo et al. 2000). The fractions contained components migrating at the expected molecular weight for reduced IgM that were stained by antihuman IgM antibodies (Fig. 1b).
a Gel-filtration HPLC of pooled plasma samples. Proteins are separated according to their molecular weight, with the larger proteins eluting first. Total protein concentration of each fraction was measured at 280 nm (gray line). The characteristic peaks were as follows: empty volume with a MW > 500 kDa (IgMs), IgGs with a MW of ~150 kDa, and the albumin peak at ~66 kDa. A direct ELISA performed on each fraction to measure the quantity of generic Aβ (diamonds) shows that most of Aβ elutes in the empty volume and IgG fractions suggesting that Aβ in the blood is strongly associated with antibodies. b Western blot against Aβ in the empty volume (IgM) fraction and IgM showing the presence of Aβ in the IgM fraction
a Sandwich ELISA. 96-well titer plates are coated with anti-Aβ (4G8). After incubation with plasma samples, the wells are washed and incubated with an anti-IgM heavy chain antibody conjugated with HRP. Signal of bound molecules is therefore only produced by complexes of both IgM and antigen. b Calibration curve obtained by serial dilutions of the IgM fraction. c Aβ-IgM (diamonds) immune complexes in the fractions derived from gel-filtration HPLC compared to total protein concentration (solid line)
To assess the relevance of these findings, plasma samples from 75 patients with AD, MCI, and from healthy donors were analyzed for the presence of Aβ–IgM ICs. Serial dilutions of the gel filtration-purified IC fraction have been used to draw a reference calibration curve. By interpolation with the standard curve, Aβ–IgM IC concentration in the plasma samples has been expressed in arbitrary units (AU)/ml. According to ANOVA test, no significant differences among the three diagnostic groups were observed (Student t test P value AD vs. HC = 0.18, AD vs. MCI = 0.61, MCI vs. HC = 0.10) (Fig. 3).
Analysis of Aβ–IgM immune complexes. a Levels of Aβ–IgM immune complexes in the different diagnostic groups. b The comparison of the mean values do not show any significant difference. c ROC curve analysis shows a certain difference in the distribution of the immune complexes plasma concentration between AD and HC groups, which however was not significant
ROC curve analysis showed that specificity was only 46.67% when sensitivity was set at 80%, and by setting specificity above 80%, sensitivity was 26.67% (Table 2).
Discussion
The aim of the present study was to analyze the serological profile of samples from AD and MCI patients, and healthy controls, regarding the levels of Aβ–IgM complexes, and to evaluate a possible correlation between the immunological profiles of individuals with AD. Immune complexes, in fact, have recently been proven to correlate better than unbound biomarkers with pathology in different cancer entities (Beneduce et al. 2005, 2007, 2008; Castaldi et al. 2005), which are characterized by an over- or mis-production of an endogenous protein. At present, only CSF Aβ42 levels is a well established Aβ-related AD biomarker with high sensitivity and specificity (Andreasen et al. 2001; Galasko et al. 1998; Kanai et al. 1998; Lewczuk et al. 2004; Tapiola et al. 2000). Unfortunately, there seems to be no correlation between CSF and blood Aβ level, as shown by several groups (Matsumoto et al. 2007; Mehta et al. 2000, 2001; Vanderstichele et al. 2000). A longitudinal study showed that CSF Aβ42 decreases within 12 months significantly in AD patients, while Tau and Phospho-Tau did not (Kessler et al. 2008). Although much better for clinical practice, blood-based Aβ levels are controversially discussed as a useful biomarker for AD. Studies have shown a decreased level of Aβ in AD subjects (Pesaresi et al. 2006; Xu and Gaskin 2008), while others showed an increase of Aβ concentration in the plasma of AD patients (Kosaka et al. 1997; Matsubara et al. 1999), or no statistical differences (Fukumoto et al. 2003; Tamaoka et al. 1996). The same inconsistency emerged from a series of prospective studies, in which a higher risk for developing AD has been associated both with higher baseline plasma Aβ42 concentration (Pomara et al. 2005) or higher Aβ40 with no effect on Aβ42 (van Oijen et al. 2006). Finally, Graff-Radford et al. (2007) linked a high risk for developing AD to a lower Aβ42/40 ratio. Plasma anti-Aβ autoantibody concentration has also been investigated by several groups. Titers of anti-Aβ42 autoantibodies were reported to be lower in AD patients compared to healthy individuals (Du et al. 2001; Weksler et al. 2002), or higher in AD patients (Nath et al. 2003). One study reported no correlation between autoantibodies titers and plasma Aβ40 or 42 levels (Hyman et al. 2001).
The initial goal of this study was to characterize the occurrence of ICs of Aβ in the plasma of AD and MCI patients and HC, as seen with many cancer biomarkers. It is well known that IgM complexes are in equilibrium in blood with the unbound respective antigen and are used as reliable blood biomarkers for diagnosis of different cancer entities. It would make sense that the same equilibrium holds true for any IgM complex in blood. Already established immune complexes as biomarkers include: PSA–IgM for prostate cancer (Beneduce et al. 2007), carcinoembryonic antigen–IgM for colorectal cancer (Castaldi et al. 2005) alpha fetoprotein–IgM and squamous cell carcinoma antigen-IgM for liver cancer (Beneduce et al. 2004, 2005). Moreover, IgM immune complexes have also been shown to be uncorrelated with basal IgM levels (Beneduce 2008). Nydegger (2007) discussed in a review article biochemical properties of immune complexes in general, their formation and their equilibrium state, stating that immune complex interaction is extremely high compared to other biochemical interactions.
Plasma samples from 30 AD patients, 15 MCI patients, and 30 age- and sex-matched HC have been analyzed to determine the levels of circulating Aβ–IgM ICs. After gel-filtration and size fractionation, Aβ was primarily found to be associated with the IgM and the IgG fractions using an ELISA. This is the first characterization of circulating Aβ–IgM complexes in AD. The Aβ–IgM assay did not show any significant difference among the three groups, in contrast with previous findings (Gruden et al. 2007), proving that although there is great interest around autoimmunity in AD, IC levels cannot be used as a diagnostic marker. It should be noted, however, that variability of IC level was high within the groups. This high variance leading to an overlap between AD patients and healthy controls might be partly due to biological variability. Consensus criteria for a suitable biomarker (Trojanowski et al. 1998) for AD were however not met.
On the other hand, the presence of circulating ICs against neuronal antigens supports the notion that autoimmune-mediated processes may be involved in neurodegenerative disorders. Further investigations are needed to elucidate the pathophysiological role of these complexes and the significance of autoantibodies in AD in general. Whether their role is neuroprotective or neurotoxic is still unknown. They may be seen both as a possible protective factor for AD, or as a risk factor in case of an unbalanced level. In any case, autoimmunity-driven homeostasis is a natural process and its understanding may be useful in both diagnosing and treating AD; there are evidences for a therapeutic use of anti-Aβ antibodies as it is being shown by current experimental immunotherapeutic approaches. Hock et al. (2003) showed that active immunization against aggregated Aβ42 led to a slower cognitive decline in a dose-dependent fashion; patients generating a higher titer of anti-Aβ antibodies performed better in cognitive test than patients who did not respond to the immunization protocol. The increase in antibody titer did not correspond to a decrease in Aβ blood levels. In contrast, significant changes were observed in serum and CSF of patients with AD after treatment with intravenous Aβ IgGs (Dodel et al. 2002).
The levels of Aβ autoantibodies of the IgG class for monitoring the effect of passive or active immunization in AD have already been evaluated by recent studies. It is speculative to discuss a possible role of Aβ–IgM levels as a predictive indicator of immunotherapy efficacy. A possible hypothesis includes that they serve as a “buffering system” to keep free potential toxic endogenous peptides and proteins under homeostatic control and lead to their clearance (Gruden et al. 2007). Previous studies have shown the presence of anti-Aβ autoantibodies (Xu and Gaskin 1997) and circulating IC of Aβ and IgGs of different classes (Gruden et al. 2004). APP transgenic mice injected intravenously with monoclonal anti-Aβ antibody showed a rapid and massive increase of CNS-derived Aβ in the plasma suggesting that antibodies may participate in Aβ clearance from the brain (DeMattos et al. 2001). However, whether this immune activity is defensive or toxic is still a matter of debate (Geylis et al. 2005; Nath et al. 2003; Woulfe et al. 2002). It will be interesting to evaluate in future studies possible relationships of Aβ-IC levels with the clinical development of MCI patients, and with AD patients’ response to immune therapies.
References
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders—DSM-IV, 4th edn. American Psychiatric Association, Washington
Andreasen N, Minthon L, Davidsson P, Vanmechelen E et al (2001) Evaluation of CSF-tau and CSF-Abeta42 as diagnostic markers for Alzheimer disease in clinical practice. Arch Neurol 58(3):373–379
Beneduce L, Castaldi F, Marino M, Tono N et al (2004) Improvement of liver cancer detection with simultaneous assessment of circulating levels of free alpha-fetoprotein (AFP) and AFP-IgM complexes. Int J Biol Markers 19(2):155–159
Beneduce L, Castaldi F, Marino M, Quarta S et al (2005) Squamous cell carcinoma antigen-immunoglobulin M complexes as novel biomarkers for hepatocellular carcinoma. Cancer 103(12):2558–2565
Beneduce L, Prayer-Galetti T, Giustinian AM, Gallotta A et al (2007) Detection of prostate-specific antigen coupled to immunoglobulin M in prostate cancer patients. Cancer Detect Prev 31(5):402–407
Beneduce L, Pesce G, Gallotta A, Zampieri F et al (2008) Tumour-specific induction of immune complexes: DCP-IgM in hepatocellular carcinoma. Eur J Clin Invest 38(8):571–577
Biere AL, Ostaszewski B, Stimson ER, Hyman BT et al (1996) Amyloid beta-peptide is transported on lipoproteins and albumin in human plasma. J Biol Chem 271(51):32916–32922
Blennow K (2004) Cerebrospinal fluid protein biomarkers for Alzheimer’s disease. NeuroRx 1(2):213–225
Castaldi F, Marino M, Beneduce L, Belluco C et al (2005a) Detection of circulating CEA-IgM complexes in early stage colorectal cancer. Int J Biol Markers 20(4):204–208
Castaldi F, Marino M, Beneduce L, Belluco C et al (2005b) Detection of circulating CEA-IgM complexes in early stage colorectal cancer Squamous cell carcinoma antigen-immunoglobulin M complexes as novel biomarkers for hepatocellular carcinoma. Int J Biol Markers 20(4):204–208
DeMattos RB, Bales KR, Cummins DJ, Dodart JC et al (2001) Peripheral anti-A beta antibody alters CNS and plasma A beta clearance and decreases brain A beta burden in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci USA 98(15):8850–8855
Dodel R, Hampel H, Depboylu C, Lin S et al (2002) Human antibodies against amyloid beta peptide: a potential treatment for Alzheimer’s disease. Ann Neurol 52(2):253–256
Du Y, Dodel R, Hampel H, Buerger K et al (2001) Reduced levels of amyloid beta-peptide antibody in Alzheimer disease. Neurology 57(5):801–805
Fukumoto H, Tennis M, Locascio JJ, Hyman BT et al (2003) Age but not diagnosis is the main predictor of plasma amyloid beta-protein levels. Arch Neurol 60(7):958–964
Galasko D, Chang L, Motter R, Clark CM et al (1998) High cerebrospinal fluid tau and low amyloid beta42 levels in the clinical diagnosis of Alzheimer disease and relation to apolipoprotein E genotype. Arch Neurol 55(7):937–945
Geylis V, Kourilov V, Meiner Z, Nennesmo I et al (2005) Human monoclonal antibodies against amyloid-beta from healthy adults. Neurobiol Aging 26(5):597–606
Giedraitis V, Sundelof J, Irizarry MC, Garevik N et al (2007) The normal equilibrium between CSF and plasma amyloid beta levels is disrupted in Alzheimer’s disease. Neurosci Lett 427(3):127–131
Graff-Radford NR, Crook JE, Lucas J, Boeve BF et al (2007) Association of low plasma Abeta42/Abeta40 ratios with increased imminent risk for mild cognitive impairment and Alzheimer disease. Arch Neurol 64(3):354–362
Gruden MA, Davudova TB, Malisauskas M, Zamotin VV et al (2004) Autoimmune responses to amyloid structures of Abeta(25–35) peptide and human lysozyme in the serum of patients with progressive Alzheimer’s disease. Dement Geriatr Cogn Disord 18(2):165–171
Gruden MA, Davidova TB, Malisauskas M, Sewell RD et al (2007) Differential neuroimmune markers to the onset of Alzheimer’s disease neurodegeneration and dementia: autoantibodies to Abeta(25–35) oligomers, S100b and neurotransmitters. J Neuroimmunol 186(1–2):181–192
Hardy J, Selkoe DJ (2002) The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 297(5580):353–356
Hock C, Konietzko U, Streffer JR, Tracy J et al (2003) Antibodies against beta-amyloid slow cognitive decline in Alzheimer’s disease. Neuron 38(4):547–554
Hyman BT, Smith C, Buldyrev I, Whelan C et al (2001) Autoantibodies to amyloid-beta and Alzheimer’s disease. Ann Neurol 49(6):808–810
Jensen M, Schroder J, Blomberg M, Engvall B et al (1999) Cerebrospinal fluid A beta42 is increased early in sporadic Alzheimer’s disease and declines with disease progression. Ann Neurol 45(4):504–511
Kanai M, Matsubara E, Isoe K, Urakami K et al (1998) Longitudinal study of cerebrospinal fluid levels of tau, A beta1-40, and A beta1-42(43) in Alzheimer’s disease: a study in Japan. Ann Neurol 44(1):17–26
Kawarabayashi T, Shoji M (2008) Plasma biomarkers of Alzheimer’s disease. Curr Opin Psychiatry 21(3):260–267
Kessler H, Pajonk FG, Bach D, Schneider-Axmann T et al (2008) Effect of copper intake on CSF parameters in patients with mild Alzheimer’s disease: a pilot phase 2 clinical trial. J Neural Transm 115(12):1651–1659
Kosaka T, Imagawa M, Seki K, Arai H et al (1997) The beta APP717 Alzheimer mutation increases the percentage of plasma amyloid-beta protein ending at A beta42(43). Neurology 48(3):741–745
Kuo YM, Kokjohn TA, Kalback W, Luehrs D et al (2000a) Amyloid-beta peptides interact with plasma proteins and erythrocytes: implications for their quantitation in plasma. Biochem Biophys Res Commun 268(3):750–756
Kuo YM, Kokjohn TA, Kalback W, Luehrs D et al (2000b) Amyloid-beta peptides interact with plasma proteins and erythrocytes: implications for their quantitation in plasma. Biochem Biophys Res Commun 268(3):750–756
Lewczuk P, Esselmann H, Otto M, Maler JM et al (2004) Neurochemical diagnosis of Alzheimer’s dementia by CSF Abeta42, Abeta42/Abeta40 ratio and total tau. Neurobiol Aging 25(3):273–281
Matsubara E, Ghiso J, Frangione B, Amari M et al (1999) Lipoprotein-free amyloidogenic peptides in plasma are elevated in patients with sporadic Alzheimer’s disease and Down’s syndrome. Ann Neurol 45(4):537–541
Matsumoto Y, Yanase D, Noguchi-Shinohara M, Ono K et al (2007) Blood-brain barrier permeability correlates with medial temporal lobe atrophy but not with amyloid-beta protein transport across the blood–brain barrier in Alzheimer’s disease. Dement Geriatr Cogn Disord 23(4):241–245
McGeer PL, McGeer EG (2001) Inflammation, autotoxicity and Alzheimer disease. Neurobiol Aging 22(6):799–809
McKhann G, Drachman D, Folstein M, Katzman R et al (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34(7):939–944
Mehta PD, Pirttila T (2005) Increased cerebrospinal fluid A beta38/A beta42 ratio in Alzheimer disease. Neurodegener Dis 2(5):242–245
Mehta PD, Pirttila T, Mehta SP, Sersen EA et al (2000) Plasma and cerebrospinal fluid levels of amyloid beta proteins 1-40 and 1-42 in Alzheimer disease. Arch Neurol 57(1):100–105
Mehta PD, Pirttila T, Patrick BA, Barshatzky M et al (2001) Amyloid beta protein 1-40 and 1-42 levels in matched cerebrospinal fluid and plasma from patients with Alzheimer disease. Neurosci Lett 304(1–2):102–106
Nath A, Hall E, Tuzova M, Dobbs M et al (2003) Autoantibodies to amyloid beta-peptide (Abeta) are increased in Alzheimer’s disease patients and Abeta antibodies can enhance Abeta neurotoxicity: implications for disease pathogenesis and vaccine development. Neuromolecular Med 3(1):29–39
Nydegger UE (2007) Immune complex pathophysiology. Ann N Y Acad Sci 1109:66–83
Pesaresi M, Lovati C, Bertora P, Mailland E et al (2006) Plasma levels of beta-amyloid (1-42) in Alzheimer’s disease and mild cognitive impairment. Neurobiol Aging 27(6):904–905
Pomara N, Willoughby LM, Sidtis JJ, Mehta PD (2005) Selective reductions in plasma Abeta 1-42 in healthy elderly subjects during longitudinal follow-up: a preliminary report. Am J Geriatr Psychiatry 13(10):914–917
Price JL, Morris JC (1999) Tangles and plaques in nondemented aging and “preclinical” Alzheimer’s disease. Ann Neurol 45(3):358–368
Singh VK (1997) Neuroautoimmunity: pathogenic implications for Alzheimer’s disease. Gerontology 43(1–2):79–94
Sundelof J, Giedraitis V, Irizarry MC, Sundstrom J et al (2008) Plasma beta amyloid and the risk of Alzheimer disease and dementia in elderly men: a prospective, population-based cohort study. Arch Neurol 65(2):256–263
Suzuki N, Cheung TT, Cai X-D, Odaka A et al (1994) An increased percentage of long amyloid β protein is secreated by familial amyloid β protein precursor (βAPP717) mutants. Science 264:1336–1340
Tamaoka A, Fukushima T, Sawamura N, Ishikawa K et al (1996) Amyloid beta protein in plasma from patients with sporadic Alzheimer’s disease. J Neurol Sci 141(1–2):65–68
Tapiola T, Pirttila T, Mehta PD, Alafuzofff I et al (2000) Relationship between apoE genotype and CSF beta-amyloid (1-42) and tau in patients with probable and definite Alzheimer’s disease. Neurobiol Aging 21(5):735–740
Tarkowski E, Andreasen N, Tarkowski A, Blennow K (2003) Intrathecal inflammation precedes development of Alzheimer’s disease. J Neurol Neurosurg Psychiatry 74(9):1200–1205
Trieb K, Ransmayr G, Sgonc R, Lassmann H et al (1996) APP peptides stimulate lymphocyte proliferation in normals, but not in patients with Alzheimer’s disease. Neurobiol Aging 17(4):541–547
Trojanowski JQ, Growdon JH (1998) A new consensus report on biomarkers for the early antemortem diagnosis of Alzheimer disease: current status, relevance to drug discovery, and recommendations for future research. J Neuropathol Exp Neurol 57(6):643–644
van Oijen M, Hofman A, Soares HD, Koudstaal PJ et al (2006) Plasma Abeta(1-40) and Abeta(1-42) and the risk of dementia: a prospective case–cohort study. Lancet Neurol 5(8):655–660
Vanderstichele H, Van Kerschaver E, Hesse C, Davidsson P et al (2000) Standardization of measurement of beta-amyloid(1-42) in cerebrospinal fluid and plasma. Amyloid 7(4):245–258
Weksler ME, Relkin N, Turkenich R, LaRusse S et al (2002) Patients with Alzheimer disease have lower levels of serum anti-amyloid peptide antibodies than healthy elderly individuals. Exp Gerontol 37(7):943–948
Winblad B, Palmer K, Kivipelto M, Jelic V et al (2004) Mild cognitive impairment—beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med 256(3):240–246
Woulfe JM, Duke R, Middeldorp JM, Stevens S et al (2002) Absence of elevated anti-alpha-synuclein and anti-EBV latent membrane protein antibodies in PD. Neurology 58(9):1435–1436
Xu S, Gaskin F (1997) Increased incidence of anti-beta-amyloid autoantibodies secreted by Epstein-Barr virus transformed B cell lines from patients with Alzheimer’s disease. Mech Ageing Dev 94(1–3):213–222
Xu W, Kawarabayashi T, Matsubara E, Deguchi K et al (2008) Plasma antibodies to Abeta40 and Abeta42 in patients with Alzheimer’s disease and normal controls. Brain Res 1219:169–179
Yamaguchi H, Sugihara S, Ogawa A, Oshima N et al (2001) Alzheimer beta amyloid deposition enhanced by apoE epsilon4 gene precedes neurofibrillary pathology in the frontal association cortex of nondemented senior subjects. J Neuropathol Exp Neurol 60(7):731–739
Acknowledgments
The excellent technical help of Petra Tucholla is gratefully acknowledged. Financial support was provided by the European Commission, Marie Curie Early Stage Training, MEST-CT-2005-020013 (NEURAD), International Alzheimer Ph.D. Graduate School.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Marcello, A., Wirths, O., Schneider-Axmann, T. et al. Circulating immune complexes of Aβ and IgM in plasma of patients with Alzheimer’s disease. J Neural Transm 116, 913–920 (2009). https://doi.org/10.1007/s00702-009-0224-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-009-0224-y