Abstract
Purpose
The definition of chronic adult hydrocephalus encompasses different pathological entities with overlapping characteristics, including long-standing overt ventriculomegaly in adults (LOVA), late-onset idiopathic aqueductal stenosis (LIAS) and idiopathic normal pressure hydrocephalus (iNPH). The aim of our study was to identify preoperative clinical and radiological features peculiar of these diseases providing some pathophysiology inferences on these forms of hydrocephalus.
Methods
Clinical and radiological preoperative records, type of surgical treatment and clinical outcome of patients with chronic adult hydrocephalus who were surgically treated between 2013 and 2019 were retrospectively reviewed. Univariate and multivariate analyses were performed to evaluate the contribution of each variable to the differential diagnosis.
Results
In total, 105 patients were included: 18 with LOVA, 23 with LIAS and 64 with iNPH. On multivariate analysis, an enlarged cisterna magna and a more severe ventriculomegaly were associated with the diagnosis of LOVA, while an older age and DESH with iNPH. LIAS patients tend to have an higher prevalence of raised ICP symptoms. Based on that, a clinical and radiological scoring system was developed to distinguish between iNPH and no iNPH cases. A precise cut-off value with a sensitivity of 95.1% and a specificity of 90.6% was identified.
Conclusions
LOVA, LIAS and iNPH are different forms of chronic adulthood hydrocephalus and present different and peculiar clinical and radiological features, with an impact on the treatment and outcome prediction. The implementation of a clinical-radiological score for differential diagnosis may help the differentiation. Further studies are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The definition of chronic adult hydrocephalus encompasses different pathological entities with overlapping characteristics. Long-standing overt ventriculomegaly in adults has been firstly described as a distinct pathological entity by Oi et al. in 1996 [34]. There are, however, other heterogeneous conditions described as “arrested hydrocephalus”, “occult hydrocephalus” or “compensated hydrocephalus” without consensus about specific features of these pathological entities. Thus, diagnostic criteria are a matter of debate even among expert clinicians [10, 17, 28, 29, 39, 40].
For instance, aqueductal stenosis has been considered as a common feature in LOVA patients, but its pathogenetic role is matter of debate [37, 42]. Thus, some authors hypothesized two subtypes of LOVA according to the patency of the aqueduct, with different aetiology [18]. Indeed, the aqueductal stenosis seems to characterize a specific subtype of adulthood hydrocephalus that can be defined as late-onset idiopathic aqueductal stenosis (LIAS) [10, 29, 44].
It is thus not clear if LIAS should be considered a subgroup of LOVA patients and if LOVA with aqueductal stenosis have different clinical, diagnostic and treatment features when compared to those without.
Furthermore, idiopathic normal pressure hydrocephalus (iNPH), a better recognized and separate clinical entity, also shares many radiological and clinical features with LOVA, especially with an open aqueduct [5, 6, 14].
The differential diagnosis between these three diseases (LOVA, LIAS, iNPH) is not trivial, as different forms of hydrocephalus may benefit from different surgical procedures, as endoscopic third ventriculostomy (ETV) or ventriculo-peritoneal shunting (VPS) [2, 7, 12, 18, 19, 21, 29, 36, 38, 41, 42]. Accordingly, a more accurate classification of chronic adulthood hydrocephalus is desirable to improve our ability to plan surgical treatment and predict patient outcome [8].
The aim of the present study was to identify specific preoperative clinical and neuroradiological features in a retrospective comparative cohort of patients with adult hydrocephalus, in order to define the major clinical and radiological characteristics of LOVA, LIAS and iNPH patients, outlining also their clinical outcome after treatment. Moreover, according to literature, the major discrimination in surgical treatment of the aforementioned pathologies is between LOVA and LIAS, for which ETV as a first choice treatment is suggested, and iNPH, which requires VPS or other forms of CSF shunting. We also explored the feasibility of a diagnostic score to support the differential diagnosis between iNPH and obstructive hydrocephalus patients.
Methods
Study design, setting and inclusion criteria
We retrospectively selected patients consecutively referred to the Department of Neurosurgery of the IRCCS Istituto delle Scienze Neurologiche di Bologna (ISNB) between July 2013 and December 2019 (78 months) and who underwent ETV and/or VPS for adult hydrocephalus.
All surgical procedures were performed by one single surgeon leading the hydrocephalus management group (G.P.). Included patients were categorized in LOVA, LIAS and iNPH subcohorts, respectively.
The following criteria were further required for being included in this study: (1) age > 18 years old; (2) exclusion of secondary hydrocephalus, such as post-traumatic, post-infectious, post-hemorrhagic or caused by neoplasms affecting the patency of CSF pathways; (3) absence of foramina of Monro, Luschka and Magendie stenosis causing hydrocephalus; (4) no previous neurosurgical procedures performed; (5) available complete preoperative imaging and clinical history.
Cohort assignment
LOVA
Characteristics of this cohort have been extensively described in a previous paper [36]. In this present study, we included in the group an open-aqueduct LOVA patients’ cohort consecutively treated at our institution. All the patients had MRI evidence of CSF flow through the aqueduct and their clinical and radiological parameters were consistent with LOVA diagnosis according to Ved’s criteria (Table 1) [42].
LIAS
In the second group, we allocated patients without CSF flow through aqueduct in phase-contrast (PC) MRI sequences, no turbulence void signal in T2-weighted images, and evidence of complete aqueductal stenosis in midsagittal thin-slice sequences, as established in literature [10, 29]. These patients were diagnosed as affected by LIAS.
iNPH
A third group included iNPH patients whose data were retrospectively analysed from an ongoing prospective observational study (the Bologna PRO-HYDRO study) database. Characteristics of this cohort have been also extensively reported in previous papers [11, 30]. Briefly, all the patients with clinical suspicion of chronic primary adulthood hydrocephalus were extensively investigated with a specific clinical and diagnostic assessment, including 3 T brain magnetic resonance imaging (MRI). iNPH clinical assessment was conducted on 5 consecutive days in our inpatient clinic and included standardized clinical evaluations, neuropsychological assessments, tap test and instrumental gait analysis before and after (24 h and 72 h) the tap test. On the basis of these findings, a multidisciplinary team (neurologists, neurosurgeons, neuropsychologists, neuroradiologists, physiatrists, engineers in movement science and nurses) established eligible patients for VPS placement. All of them were consistent with the diagnosis of “probable iNPH” according to the 2005 guidelines [38].
Variables
The following preoperative clinical and radiological features were collected from clinical and radiological records: (1) age and sex; (2) symptomatology on admission as headache, nausea, papilledema, gait disturbance, urinary incontinence, cognitive impairment; (3) cranial circumference (measured in centimetres); (4) neuroradiological features as evidence of sellar bone distortion, empty sella (defined as at least 66% of pituitary height loss, grades IV–V according to Yuh WTC et al. [46]), DESH sign [32], bulging of the third ventricle floor [16, 33], an enlarged cisterna magna measuring ≥ 10 mm on mid-sagittal images [4], Evans’ index, third ventricle width (measured in millimetres), callosal angle and tentorial angle. Moreover, the type of surgical procedures the patients underwent and their clinical status at the last follow-up visit were also collected. The outcome was classified as “improved” if any improvement in at least one symptomalogical domain was reported (with stability of the remaining ones), “stable” if complete stability or halting of the symptomatological progression were described and “worsened” if the patient suffered deterioration in at least one domain of the preoperative status.
The qualitative radiological parameters were independently evaluated by three blinded researchers (A.C., E.L.C. and M.M.) and discussion was performed in case of disagreement. For continuous data collected, the mean among the three measurements was calculated and included. Data were reported according to the STROBE guidelines for observational studies.
Diagnostic score
The proposed diagnostic score is shown in Table 2. Every patient included in our study, according to his clinical and radiological features, received a grade for each domain, which are added up to obtain a single score ranging from 0 to 17. In contrast to the “iNPH” cohort, in the “no iNPH” cohort were included both LIAS and LOVA patients.
Data sources
Clinical and neuroradiological data were retrospectively collected from our institution digital records and included in an-hoc anonymized database.
Ethics approval
The aforementioned prospective PRO-HYDRO study was approved by the Ethics Review Board of our Institute (Cod. CE: 14,131, 23/02/2015.) and all patients consented to the use of their clinical records for research. On the other hand, ethics committee approval was waived for the retrospective observational part of this study.
Statistical methods
The statistical analysis was performed with IBM SPSS Statistics Version 28.0.1.0 (IBM Corp. Released 2021. IBM SPSS Statistics for Mac. Armonk, NY: IBM Corp.). Normal distribution was analysed with the Shapiro–Wilk test. According to their normal or not normal distribution, continuous variables (age, cranial circumference, tentorial angle, callosal angle, Evans’ index and third ventricle width) were compared using parametric one-way ANOVA and non-parametric Kruskal–Wallis H test, respectively. Bonferroni and Mann–Whitney U post hoc test was performed to evaluate intergroup variability. Categorical variables (sex, sellar bone distortion, empty sella, bulging of third ventricle floor, enlarged cisterna magna and all the clinical manifestations) were catalogued in contingency tables according to the patients’ cohort and compared with Freeman-Halton extension of the Fisher exact probability test. LOVA and LIAS outcome comparison was also compared with two-tailed Fisher exact probability test. Significant parameters on univariate analysis were compared with multivariate logistic regression. Furthermore, cutoff values between different pathological entities were determined using different receiver operating characteristic (ROC) curves, and accuracy rates were calculated measuring areas under the ROC curves (AUC). AUCs < 0.5 were excluded. The Youden Index (J) was used to determine the sensitivity and specificity rates of the cutoff values between populations. Odds ratios (OR) and confidence intervals (CI) of different cutoff values were determined using contingency tables.
Similarly, cutoff values of the continuous variables included in the diagnostic score were also determined using ROC curves and AUCs. Variables with AUC < 0.5 were excluded from the diagnostic score. The cutoff score between “iNPH” and “no iNPH” population, its sensitivity and specificity was also calculated with Youden Index. Odds ratios (OR) and confidence intervals (CI) of different cutoff values were determined using contingency tables.
The p-value was assumed to be statistically significant when ≤ 0.05.
Results
Demographics
A total of 192 patients in the selected timespan were considered and analysed for the purpose of this study. Twenty-two (11.5%) lacked complete clinical and/or radiological data and were therefore excluded, as well as 58 (30.2%) who were treated for secondary hydrocephalus and 7 (3.6%) who had undergone previous neurosurgical procedures. Of 105 patients included in this study, 18 (12 males and 6 females) were assigned to the LOVA cohort, 23 (12 males and 11 females) to the LIAS cohort and 64 (33 males and 31 females) to iNPH group.
Median age at the time of surgery significantly differed among the three groups: 70 years (64–72) for LOVA, 59 (38–68.5) years for LIAS and 75.5 (73–78.75) for iNPH, p < 0.001 (Table 3).The univariate analysis demonstrated that LOVA were significantly older than LIAS (p = 0.03) and significantly younger than iNPH patients (p < 0.001). ROC analysis reported a cutoff of 59.5 years to discriminate LOVA and LIAS, J = 0.41, OR 1.974 (Supplementary Table 1 and Table 4). No difference in gender rates was identified.
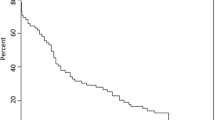
Clinical features
Clinical characteristics are summarized and compared in Fig. 1 and Tables 3 and 4. Signs and symptoms of raised ICP were reported in LOVA (16.7% for headache and 11.1% for nausea) and LIAS (30.4% and 8.7%, respectively), while they were absent in iNPH patients. A significant lower occurrence of headache was reported in iNPH group when compared to LOVA and LIAS (p = 0.04 and p < 0.001, respectively) by univariate analysis. Similar results were found for nausea, with borderline significance (p = 0.05) between LOVA and iNPH. Multivariate analysis did not yield significant results.
Incidental papilledema, in our cohort, was found only in one patient suffering from LIAS and therefore was not analysed among the other clinical manifestations.
At least one of the Hakim’s triad symptoms was reported in every iNPH patient, with a constant presence of gait abnormalities and a high prevalence of urinary incontinence and cognitive impairment (89.1% and 87.5% respectively). Symptoms of Hakim’s triad were reported in a slightly smaller proportion of the LOVA cohort, with gait abnormalities present in 94.4% of the patients, urinary incontinence in 83.3% and cognitive impairment in 66.7%. These symptoms were, however, less frequent in LIAS patients, with a prevalence of 73.9%, 43.5% and 39.1% respectively. Univariate analysis showed strong significance comparing Hakim’s triad between LIAS and iNPH cohorts (p < 0.001) and when comparing the prevalence of urinary incontinence in LOVA and LIAS (p = 0.03).
Median cranial circumference was 58.5, 57 and 56 cm in LOVA, LIAS and iNPH with a statistically significant difference between LOVA and iNPH (p = 0.001).
ROC analysis reported a cranial circumference cutoff of 56.5 cm to discriminate between LOVA and iNPH, J = 0.36, OR 1.320 (Supplementary Table 1 and Table 4).
Radiological features
Neuroradiological features of the 3 groups are shown and compared in Fig. 1, Tables 4 and 5, Supplementary Table 1. No significant difference in tentorial angle between cohorts was found. On the other hand, a significant difference in Evans’ index was disclosed among groups (p < 0.001). This significance was ascribable to the difference between LOVA and both LIAS (p = 0.02) and iNPH (p < 0.001). Moreover, ROC analysis determined Evans’ index cutoff values of 0.365 (J = 0.37, OR 1.974) and 0.425 (J = 0.59, OR 2.456) between LOVA and the other two entities, respectively.
We found a significant larger third ventricle width comparing LOVA with LIAS (p = 0.01) and iNPH (p = 0.002), mirroring the Evans’ index. Furthermore, ROC curves showed a cutoff value of 13.5 mm (J = 0.5, OR 2.253) for LOVA vs. LIAS and 18.5 mm (J = 0.45, OR 2.429) for LOVA vs. iNPH.
In addition, comparable but not equal results have been reported analyzing the callosal angle. A significant variation between the three groups was found (p = 0.02); the post hoc analysis reported a significantly smaller callosal angle (p = 0.04) in LOVA compared to LIAS. The iNPH group showed a smaller callosal angle than the LIAS one, without reaching a statistical significance (p = 0.06).
Multivariate analysis confirmed the role of ventricular size (i.e. third ventricle width) as an independent predictor of the diagnosis of LOVA.
The prevalence of an empty sella was not found to be significantly different in the three cohorts. On the other hand, sellar bone abnormalities and the bulging of third ventricle floor were reported to be significant features of LOVA and LIAS but not of iNPH. The prevalence of an empty sella was 27.8% in LOVA and 17.4% in LIAS, while it was found only in one iNPH patient. Univariate analysis confirms these findings (p = 0.002 and p = 0.02, respectively). Similar results were reported for the bulging of the third ventricle floor, as it was found in 38.9% of the LOVA cohort, 60.9% of the LIAS cohort and only 7.8% of the iNPH cohort. Statistical significance on univariate analysis (p = 0.005 and p < 0.001, respectively) was shown.
A remarkable finding was an enlarged cisterna magna in all the patients of the LOVA cohort, especially when compared to its prevalence in LIAS (4.3%) and iNPH (39.1%). Univariate analysis confirmed the differences between the cohorts with strong statistical significance (p < 0.001).
DESH sign, as a well-known typical feature of iNPH, was found in 93.8% of this cohort, with a significantly lower (p < 0.001) prevalence in LOVA (11.1%) and LIAS (4.3%).
Further multivariate analysis did not confirm the significance of sellar distortion and bulging of the third ventricle floor, but strongly underlined enlarged cisterna magna (p < 0.001 or p = 0.002) as a differentiation factor between the three pathologies and DESH (p < 0.001) as a typical feature of iNPH.
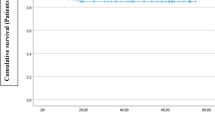
Diagnostic score
According to cohort assignment, 64 patients were included in the iNPH cohort and 41 patients in the “no iNPH” cohort. ROC curves identified different cutoffs of the continuous variables, except for callosal angle which showed an AUC of 0.44 and was therefore excluded (Supplementary Table 2). Similarly, contingency tables analysed ORs and CIs of the features included in the proposed diagnostic score (Supplementary Table 3).
Furthermore, ROC curve analysis, as outlined in Fig. 2, reported a cutoff value of 3.5 to best discriminate between iNPH and no iNPH cohorts (J = 0.857, OR 188.5, 95% CI 36.166–982.469). Patients with a diagnostic score of 3 or less belong, with a sensitivity of 95.1% and a specificity of 90.6%, to the iNPH cohort. Conversely, patients with a diagnostic score of 4 or more belong with the same accuracy to the “no iNPH” cohort.
Clinical outcome
Among LOVA patients, 12 underwent ETV and 6 underwent VPS. Five patients (27.8%) were lost to follow-up, 3 of them belonging to ETV group and 2 to VPS. A clinical improvement at follow-up visit was reported in 6 patients receiving ETV (66.7%), stability in 1 patient (11.1%) and clinical worsening in 2 patients (22.2%). Median follow-up was 38 months (interquartile range 15–67) [36].
In the LIAS cohort, all the patients underwent ETV, with 2 (8.7%) lost to follow-up. A clinical improvement was reported in all patients at a median follow-up duration of 28 months (interquartile range 6–44).
All the patients with a diagnosis of iNPH underwent VPS. Two (3.1%) were lost to follow-up. Clinical improvement was observed in 45 cases (72.6%), stability in 6 cases (9.7%) and worsening in 11 cases (17.7%). Median follow-up was 16 months (interquartile range 6–24).
Discussion
In this study, a clinical and radiological categorization of patients with chronic hydrocephalus was attempted. Some of those characteristics turned out to have a significant diagnostic value. Among the most relevant, ventriculomegaly, measured by an enlarged third ventricle width and Evans index > 0.40, a cranial circumference > 56.5 cm and an over-represented cisterna magna were distinctive features of LOVA. Moreover, we found a remarkable correlation of an enlarged cisterna magna and upward compressed cerebellar folia with the diagnosis of LOVA. This finding is indeed of value when speculating on the possible physiopathology of this entity and helps understanding why an apparent form of communicating hydrocephalus responds satisfactorily to ETV. We also propose a scoring system to support the differential diagnosis between iNPH and no iNPH based on clinic-radiological characteristics retrieved in our patients. The present comparative study actually completes our previous work whose aim was to shedding some light on the misty differential diagnosis of adulthood chronic hydrocephalus [36].
The cisterna magna enlargement
We consider the regular evidence of an enlarged cisterna magna in all the patients included in our LOVA cohort as the most relevant finding of our study. This feature is rare in LIAS patients (4.3%) and has a limited prevalence in iNPH patients (38.1%). Furthermore, the continuous turbulent flow starting from the third ventricle, throughout the aqueduct and fourth ventricle until the cisterna magna and the distorted anatomy of the posterior fossa, yet previously described [36], characterized by an upwards shifted cerebellum and compressed caudal folia (Fig. 3), are lacking in the other patients’ cohorts, especially in iNPH when a slightly enlarged cisterna magna could be observed (Fig. 4). According to these results, an enlarged cisterna magna be taken into consideration as a possible diagnostic criteria of open-aqueduct LOVA. This feature is also associated, due to its strongly correlation with LOVA, with a more severe ventriculomegaly as further discussed.
T2-weighted MRI showing landmark features of LOVA in midsagittal (A), axial (B) and coronal (C) view. A Empty sella, patent aqueduct with turbulent flow and an enlarged cisterna magna are reported. B, C Concomitant severe supratentorial ventriculomegaly is observed. Evans Index: 0.47. Third ventricle width: 26 mm
T2-weighted MRI in midsagittal view of the three different types of adult hydrocephalus analysed in our study is compared. A LOVA, distorted and empty sella, bulging of third ventricle floor, turbulent flow through the aqueduct and an enlarged cisterna magna with upwards shifted cerebellar vermis are showed. B LIAS, CSF flow throughout the aqueduct, which is totally obstructed by a thin septum, is absent. C iNPH, with a patent aqueduct, and no abnormalities in the anatomy of sella turcica, third ventricle floor and cisterna magna
Thus, to our knowledge, this is one of the first studies to correlate supratentorial adult hydrocephalus and the increased volumetry of the cisterna magna as a specific characteristic of the open-aqueduct LOVA subgroup of patients. Our study corroborates the theory of the “intracisternal” obstruction in communicant hydrocephalus with a bulging third ventricle floor, hypothesized by Kehler in 2003 [23] and discussed by Kageyama [22] in 2016 and Al-Hakim in 2019 [1], as peculiar of LOVA, in view of the lack of posterior fossa abnormalities in the other cohorts. Venous stenosis, as already theorized by other authors, could have a possible role in distal CSF blockade and impaired reabsorption, but this does not explain the satisfactory outcomes achieved by ETV in patients without aqueductal stenosis [36, 42].
The ventricle size
According to our observations, LOVA cases had a cranial circumference significantly greater than iNPH but similar to LIAS. They had a median age of 70, the presence of an enlarged cisterna magna and a symptomatology encompassing raised ICP and Hakim’s triad (Fig. 2).
Moreover, Ibanez-Botella et al. underlined the “overt” ventriculomegaly as a feature of LOVA patients, proposing a minimum Evans’ index of 0.4 as a criterion for their diagnosis [18]. Our study confirms this severe degree of ventriculomegaly in LOVA, especially when compared to the other forms of chronic adulthood hydrocephalus. The two parameters assessing ventriculomegaly, namely the Evans’ index and third ventricle width, have the potential to provide robust differentiation among LOVA and the other two groups. Reasonably, this phenomenon reflects the “long-standing” feature of this pathology, with a slow and almost asymptomatic course for the most part of the patient’s lifespan until late decompensation, and the induced adaptive changes of the brain and the ventricular anatomy [35, 45]. Nonetheless, in our opinion, a cut-off value of 0.4 in the Evans’ index could be too strict for the diagnosis of LOVA and therefore carrying a concrete risk of misdiagnosing some patients, as underlined in our previous analysis [36]. The aforementioned cut-off value, for example, would have excluded one quarter of the analysed LOVA cohort.
Other parameters
On the other hand, LIAS patients represented the youngest cohort, with a median age at surgery of 59, whereas LOVA patients had a median age of 70 and iNPH a median age of 75.5 (Table 3).
LIAS and LOVA presented higher rates of sellar bone abnormalities and bulging of the third ventricle, although only at univariate analysis, when compared to iNPH. These results are congruous with the obstructive pathogenetic hypothesis of both subtypes of chronic hydrocephalus. iNPH, according to its “normal pressure” definition, lacks these features [32]. The callosal angle, which is a widely accepted parameter to differentiate iNPH from atrophic hydrocephalus and a predictor of outcome [20, 43], was similar between LOVA and iNPH (median values 63 and 69 degrees, respectively), but much higher in LIAS (median 87 degrees). On the other hand and in line with literature, the prevalence of DESH, a recognized and peculiar feature of iNPH, was a characteristic of the iNPH where it was present in 93.8% versus 11.1% in LOVA and 4.3% in LIAS (Table 5 and Fig. 3).
Clinical symptoms caused by raised ICP, like headache and nausea, were present in our LOVA and LIAS cohort, although infrequently (overall less than 30% of prevalence), but substantially absent in iNPH. These results mirror the prevalence of sellar bone changes and third ventricle floor bulging, indeed reflecting obstructive pathogenesis with long-standing raised ICP. Green et al. recently investigated ICP measurements and amplitude in a direct comparison between iNPH and LIAS patients, with the expected finding of a mean higher ICP in the latter cohort, although not critical and lower than the 15 mmHg cut-off, strengthening the hypothesis of a chronically compensated supratentorial CSF accumulation due to aqueductal stenosis [13]. Other authors also underlined the role of ICP pulsatility in the etiopathogenesis of LIAS [9].
As expected, a complete Hakim’s triad was fundamental for the diagnosis of iNPH, with gait disturbance as a constant symptom of that cohort, urinary incontinence found in 89.1% of patients and cognitive impairment in 87.5%.
A similar occurrence of the Hakim’s triad was present, in slightly smaller percentages, in open-aqueduct LOVA. On the other hand, it was less frequent in LIAS, with gait disturbances found in 73.9% of patients, urinary incontinence in 43.5% and cognitive impairment in only 39.1%. Thus, LOVA could be recognized as a pathological entity characterized by overlapping symptoms from the other two categories of adult hydrocephalus.
A diagnostic score
Different scales to classify and standardize hydrocephalus symptoms and radiological findings are available and validated [3, 15, 24,25,26,27, 31]. Nevertheless, a comprehensive diagnostic score including clinical and radiological features, with a clear aim on differential diagnosis of adult hydrocephalus, has never been proposed. Developing our score, we focused on the differential diagnosis of pathologies requiring different forms of surgical treatment, with the final goal of providing a practical tool to discriminate between iNPH and no iNPH cases. According to our results, a diagnostic score with such features is feasible with satisfactory accuracy (sensitivity of 95.1% and specificity of 90.6%). We purposely chose to exclude the enlarged cisterna magna and the aqueductal stenosis from our scoring system. As the first one is a constant of the LOVA cohort and the second one as part of the LIAS cohort by definition, they were used to differentiate the two included forms of obstructive hydrocephalus. Moreover, an enlarged cisterna magna is also an inconstant but not trascurable finding of the iNPH cohort. It is clear and we underline that the proposed score is a proof-of-principle of its feasibility, as it is modeled and analysed only in a small, retrospective and monocentric cohort. On the other hand, it could also represent a starting point for hydrocephalus researchers, to be improved, extended and validated in larger cohorts.
Clinical outcome
Overall, ETV turned out to be successful in 90% of no iNPH patients, with a higher rate of symptoms improvement in LIAS as compared to LOVA (p = 0.02). This is in line with the findings of Ibáñez-Botella et al. and Ved et al. reporting an ETV success rate between 76 and 93% [18, 42]. These satisfactory results seem to corroborate the “obstructive” pathophysiological mechanism of no iNPH cases and support our view about the necessity of robust criteria for distinguishing iNPH from no iNPH to identify patients that may benefit from ETV.
Strengths and limitations
The strengths of our study are that all patients included were diagnosed in a single centre, by an established hydrocephalus-focused multidisciplinary team of expert physicians. Similarly, iNPH patients were gathered from an established prospective study which ensured systematicity of the data collection and strict adhesion to diagnostic criteria according to 2005 guidelines.
There are, however, some limitations. As an unavoidable bias of the retrospective data collection, patients which lacked complete data were excluded (a significant percentage of 11.5%). A significant, but substantially unavoidable limitation of our study is the overlapping of many features of the analysed pathologies, especially between open-aqueduct LOVA and iNPH. Since the two pathologies share many tracts and there is an inevitable diagnostic “grey zone”, patients with LOVA could have been treated as iNPH patients and vice versa, despite the adhesion to diagnostic criteria established in literature [36, 38, 42]. Furthermore, our routine hydrocephalus diagnostic algorithm lacked systematical fundus examination, ICP measurement and MR-venography to investigate potential obstacles to venous outflow with impaired retrograde CSF reabsorption. The results of all of these diagnostic procedures results could have also be compared between the three cohorts, shedding more light on peculiar features of the analysed pathologies. Finally, despite iNPH incidence is significant, and it is diagnosed and treated daily on a worldwide basis, LOVA and LIAS diagnosis are not as common, even in specialized centres, leading us to analyse small sample sizes which may preclude a more thorough statistical analysis and a better generalizability of the results.
Further analysis of surgical outcome, complications and factors predicting treatment success is beyond the scope of this paper, which primarily and purposely focuses on preoperative features.
Conclusions and implications of our study
The definitive identification of specific clinical and neuroradiological features of LOVA, LIAS and iNPH could help in defining their clinical criteria, which up to now also remains a challenge, and therefore could help to standardize the management and treatment of these patients. Despite some overlapping characteristics between the three cohorts, we suggest that typical open-aqueduct LOVA patients are on average 70 years old and significantly younger than the usual iNPH, but older than LIAS. Similarly to LIAS, they have macrocephaly and suffer from a severe degree of ventriculomegaly, sometimes with sellar bone changes or bulging of the third ventricle floor. Both LIAS and LOVA typically lack a DESH sign that is a marker of iNPH. The finding of an enlarged cisterna magna with an observed caudal cerebellar compression in LOVA caused by an hypothesized “intracisternal obstruction” appears to be a peculiar feature which can be proposed between of its diagnostic criteria. This study provides some additional evidence concerning the clinical characteristics and neuroradiological features of different forms of adult hydrocephalus. Our clinical-radiological findings should be considered in the diagnostic criteria of these misdiagnosed and heterogeneous forms of adult hydrocephalus. Moreover, according to our reports, a diagnostic score with the aim of differentiate these separate pathological entities appears to be feasible and could have a role in clinical practice, although with mandatory validation on larger cohorts. Further well-designed, prospective and multicentric studies on larger samples should be performed to improve our results.
Data availability
The authors declare that the gathered data included and used for analysis outline are available in the manuscript.
Code availability
Not applicable.
References
Al-Hakim S, Schaumann A, Tietze A, Schulz M, Thomale U-W (2019) Endoscopic third ventriculostomy in children with third ventricular pressure gradient and open ventricular outlets on MRI. Childs Nerv Syst 35(12):2319–2326
Bianchi F, Ducoli G, Moriconi F, Chieffo DPR, Anile C, Tamburrini G (2021) Long-standing overt ventriculomegaly in adults and endoscopic third ventriculostomy, the perfect treatment for the proper diagnosis. World Neurosurg 149:104–110
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzer HA, Avezaat CJ, de Jong DA, Gooskens RH, Hermans J (1997) Dutch normal-pressure hydrocephalus study: prediction of outcome after shunting by resistance to outflow of cerebrospinal fluid. J Neurosurg 87(5):687–693
Bosemani T, Orman G, Boltshauser E, Tekes A, Huisman TAGM, Poretti A (2015) Congenital abnormalities of the posterior fossa. Radiographics 35(1):200–220
Bradley WG (2016) Magnetic resonance imaging of normal pressure hydrocephalus. Semin Ultrasound CT MR 37(2):120–128
Bräutigam K, Vakis A, Tsitsipanis C (2019) Pathogenesis of idiopathic normal pressure hydrocephalus: a review of knowledge. J Clin Neurosci 61:10–13
Burtscher J, Bartha L, Twerdy K, Eisner W, Benke T (2003) Effect of endoscopic third ventriculostomy on neuropsychological outcome in late onset idiopathic aqueduct stenosis: a prospective study. J Neurol Neurosurg Psychiatry 74(2):222–225
Craven CL, Ramkumar R, D’Antona L, Thompson SD, Thorne L, Watkins LD, Toma AK (2019) Natural history of ventriculomegaly in adults: a cluster analysis. J Neurosurg 132(3):741–748
Eide PK (2018) The pathophysiology of chronic noncommunicating hydrocephalus: lessons from continuous intracranial pressure monitoring and ventricular infusion testing. J Neurosurg 129(1):220–233
Fukuhara T, Luciano MG (2001) Clinical features of late-onset idiopathic aqueductal stenosis. Surg Neurol 55(3):132–136; discussion 136–137
Giannini G, Palandri G, Ferrari A et al (2019) A prospective evaluation of clinical and instrumental features before and after ventriculo-peritoneal shunt in patients with idiopathic normal pressure hydrocephalus: the Bologna PRO-Hydro study. Parkinsonism Relat Disord 66:117–124
Giordan E, Palandri G, Lanzino G, Murad MH, Elder BD (2018) Outcomes and complications of different surgical treatments for idiopathic normal pressure hydrocephalus: a systematic review and meta-analysis. J Neurosurg Nov 1:1–13
Green LM, Wallis T, Schuhmann MU, Jaeger M (2021) Intracranial pressure waveform characteristics in idiopathic normal pressure hydrocephalus and late-onset idiopathic aqueductal stenosis. Fluids Barriers CNS 18(1):25
Hashimoto M, Ishikawa M, Mori E, Kuwana N (2010) Study of INPH on neurological improvement (SINPHONI) Diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: a prospective cohort study. Cerebrospinal Fluid Res 7:18
Hellström P, Klinge P, Tans J, Wikkelsø C (2012) A new scale for assessment of severity and outcome in iNPH. Acta Neurol Scand 126(4):229–237
Hellwig D, Grotenhuis JA, Tirakotai W, Riegel T, Schulte DM, Bauer BL, Bertalanffy H (2005) Endoscopic third ventriculostomy for obstructive hydrocephalus. Neurosurg Rev 28(1):1–34; discussion 35–38
Hong J, Barrena BG, Lollis SS, Bauer DF (2016) Surgical management of arrested hydrocephalus: case report, literature review, and 18-month follow-up. Clin Neurol Neurosurg 151:79–85
Ibáñez-Botella G, González-García L, Carrasco-Brenes A, Ros-López B, Arráez-Sánchez MÁ (2017) LOVA: the role of endoscopic third ventriculostomy and a new proposal for diagnostic criteria. Neurosurg Rev 40(4):605–611
Isaacs AM, Bezchlibnyk YB, Yong H, Koshy D, Urbaneja G, Hader WJ, Hamilton MG (2016) Endoscopic third ventriculostomy for treatment of adult hydrocephalus: long-term follow-up of 163 patients. Neurosurg Focus 41(3):E3
Ishii K, Kanda T, Harada A, Miyamoto N, Kawaguchi T, Shimada K, Ohkawa S, Uemura T, Yoshikawa T, Mori E (2008) Clinical impact of the callosal angle in the diagnosis of idiopathic normal pressure hydrocephalus. Eur Radiol 18(11):2678–2683
Jenkinson MD, Hayhurst C, Al-Jumaily M, Kandasamy J, Clark S, Mallucci CL (2009) The role of endoscopic third ventriculostomy in adult patients with hydrocephalus. J Neurosurg 110(5):861–866
Kageyama H, Miyajima M, Ogino I, Nakajima M, Shimoji K, Fukai R, Miyake N, Nishiyama K, Matsumoto N, Arai H (2016) Panventriculomegaly with a wide foramen of Magendie and large cisterna magna. J Neurosurg 124(6):1858–1866
Kehler U, Gliemroth J (2003) Extraventricular intracisternal obstructive hydrocephalus–a hypothesis to explain successful 3rd ventriculostomy in communicating hydrocephalus. Pediatr Neurosurg 38(2):98–101
Kockum K, Lilja-Lund O, Larsson E-M, Rosell M, Söderström L, Virhammar J, Laurell K (2018) The idiopathic normal-pressure hydrocephalus Radscale: a radiological scale for structured evaluation. Eur J Neurol 25(3):569–576
Kockum K, Virhammar J, Riklund K, Söderström L, Larsson E-M, Laurell K (2020) Diagnostic accuracy of the iNPH Radscale in idiopathic normal pressure hydrocephalus. PLoS One 15(4):e0232275
Krauss JK, Droste DW, Vach W, Regel JP, Orszagh M, Borremans JJ, Tietz A, Seeger W (1996) Cerebrospinal fluid shunting in idiopathic normal-pressure hydrocephalus of the elderly: effect of periventricular and deep white matter lesions. Neurosurgery 39(2):292–299; discussion 299–300
Kubo Y, Kazui H, Yoshida T, Kito Y, Kimura N, Tokunaga H, Ogino A, Miyake H, Ishikawa M, Takeda M (2008) Validation of grading scale for evaluating symptoms of idiopathic normal-pressure hydrocephalus. Dement Geriatr Cogn Disord 25(1):37–45
Larsson A, Stephensen H, Wikkelsø C (1999) Adult patients with “asymptomatic” and “compensated” hydrocephalus benefit from surgery. Acta Neurol Scand 99(2):81–90
Locatelli M, Draghi R, DI Cristofori A, Carrabba G, Zavanone M, Pluderi M, Spagnoli D, Rampini P (2014) Third ventriculostomy in late-onset idiopathic aqueductal stenosis treatment: a focus on clinical presentation and radiological diagnosis. Neurol Med Chir (Tokyo) 54(12):1014–1021
Mantovani P, Giannini G, Milletti D et al (2021) Anterior callosal angle correlates with gait impairment and fall risk in iNPH patients. Acta Neurochir (Wien) 163(3):759–766
Meier U (2002) The grading of normal pressure hydrocephalus. Biomed Tech (Berl) 47(3):54–58
Mori E, Ishikawa M, Kato T et al (2012) Guidelines for management of idiopathic normal pressure hydrocephalus: second edition. Neurol Med Chir (Tokyo) 52(11):775–809
Morota N, Watabe T, Inukai T, Hongo K, Nakagawa H (2000) Anatomical variants in the floor of the third ventricle; implications for endoscopic third ventriculostomy. J Neurol Neurosurg Psychiatry 69(4):531–534
Oi S, Sato O, Matsumoto S (1996) Neurological and medico-social problems of spina bifida patients in adolescence and adulthood. Child’s Nervous System 12(4):181–187
Oi S, Shimoda M, Shibata M, Honda Y, Togo K, Shinoda M, Tsugane R, Sato O (2000) Pathophysiology of long-standing overt ventriculomegaly in adults. J Neurosurg 92(6):933–940
Palandri G, Carretta A, La Corte E, Mazzatenta D, Conti A (2021) Longstanding overt ventriculomegaly in adults (LOVA) with patent aqueduct: surgical outcome and etiopathogenesis of a possibly distinct form of chronic hydrocephalus. Acta Neurochir (Wien) 163(12):3343–3352
Rekate HL (2007) Longstanding overt ventriculomegaly in adults: pitfalls in treatment with endoscopic third ventriculostomy. Neurosurg Focus 22(4):E6
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM (2005) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57(3 Suppl):S4–16; discussion ii-v
Schick RW, Matson DD (1961) What is arrested hydrocephalus? J Pediatr 58:791–799
Torkelson RD, Leibrock LG, Gustavson JL, Sundell RR (1985) Neurological and neuropsychological effects of cerebral spinal fluid shunting in children with assumed arrested (“normal pressure”) hydrocephalus. J Neurol Neurosurg Psychiatry 48(8):799–806
Tuniz F, Fabbro S, Piccolo D, Vescovi MC, Bagatto D, Cramaro A, Skrap M (2021) Long-standing overt ventriculomegaly in adults (LOVA): diagnostic aspects, CSF dynamics with lumbar infusion test and treatment options in a consecutive series with long-term follow-up. World Neurosurg 156:e30–e40
Ved R, Leach P, Patel C (2017) Surgical treatment of long-standing overt ventriculomegaly in adults (LOVA). Acta Neurochir (Wien) 159(1):71–79
Virhammar J, Laurell K, Cesarini KG, Larsson E-M (2014) The callosal angle measured on MRI as a predictor of outcome in idiopathic normal-pressure hydrocephalus. J Neurosurg 120(1):178–184
Wilkinson HA, LeMay M, Drew JH (1966) Adult aqueductal stenosis. Arch Neurol 15(6):643–648
Xiao L, Xu C, Liu Y, Dong L, Wei F, Wang L, Li D (2019) The surgical results of endoscopic third ventriculostomy in long-standing overt ventriculomegaly in adults with papilledema. Clin Neurol Neurosurg 183:105366
Yuh WT, Zhu M, Taoka T, Quets JP, Maley JE, Muhonen MG, Schuster ME, Kardon RH (2000) MR imaging of pituitary morphology in idiopathic intracranial hypertension. J Magn Reson Imaging 12(6):808–813
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The prospective PRO-HYDRO study was approved by the Ethics Review Board of our Institute (Cod. CE: 14131, 23/02/2015.). Ethics committee approval was waived for the retrospective observational part of this study.
Consent to participate
All patients enrolled in the prospective PRO-HYDRO study gave informed consent to the use of their clinical records for research. Informed consent was waived for the retrospective observational part of this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on CSF Circulation
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Palandri, G., Carretta, A., La Corte, E. et al. Open-aqueduct LOVA, LIAS, iNPH: a comparative clinical-radiological study exploring the “grey zone” between different forms of chronic adulthood hydrocephalus. Acta Neurochir 164, 1777–1788 (2022). https://doi.org/10.1007/s00701-022-05215-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05215-9