Abstract
Background
Delirium is an acute and reversible deterioration of mental state. Postoperative delirium (POD) can develop after surgical procedures and is associated with impaired health status and worse recovery. So far, there is little data about postoperative delirium after brain surgery. The aim of this study was to evaluate frequency, risk factors, and prognostic value of POD in predicting short-term postoperative outcomes after brain tumor surgery.
Methods
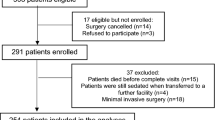
Five-hundred and twenty-two patients who underwent elective brain tumor surgery in 2010–2017 were included in this prospective study. Patients were monitored for POD using the Confusion Assessment Method for the ICU (CAM-ICU) for 2 to 7 days after the surgery. At hospital discharge, outcomes were evaluated using the Glasgow Outcome Scale (GOS).
Results
POD was diagnosed in 22 (4.2%) patients. Risk factors of POD were low level of hemoglobin, poor functional status at time of admission, low education level and older age (65 years and older). POD incidence was not associated with brain tumor laterality, location, extent of resection, histological diagnosis, or affected brain lobe. POD was associated with greater risk for unfavorable outcomes at hospital discharge (OR = 5.3; 95% CI [2.1–13.4], p = 0.001).
Conclusions
POD is not a common complication after elective brain tumor surgery. Older age, poor functional status, low education level and anemia are associated with greater POD risk. Extent of surgical intervention and brain tumor location are not associated with POD risk. POD is associated with worse outcome at hospital discharge.

Similar content being viewed by others
References
Ahmed S, Leurent B, Sampson E (2014) Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Ageing 43(3):326–333
Aitken S, Blyth F, Naganathan V (2017) Incidence, prognostic factors and impact of postoperative delirium after major vascular surgery: a meta-analysis and systematic review. Vasc Med 22(5):387–397
Aldecoa C, Bettelli G, Bilotta F et al (2017) European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol 34(4):192–214
Androsova G, Krause R, Winterer G, Schneider R (2015) Biomarkers of postoperative delirium and cognitive dysfunction. Front Aging Neurosci 7:1–16
Bettelli G, Neuner B (2017) Postoperative delirium: a preventable complication in the elderly surgical patient. Monaldi Arch Chest Dis 87(2):31–33
Brauer C, Morrison R, Silberzweig S, Siu A (2000) The cause of delirium in patients with hip fracture. Arch Intern Med 160(12):1856–1860
Bunevicius A, Kazlauskas H, Raskauskiene N, Mickuviene N, Ndreu R, Corsano E et al (2015) Role of N-terminal pro-B-type natriuretic peptide, high-sensitivity C-reactive protein, and Inteleukin-6 in predicting a poor outcome after a stroke. Neuroimmunomodulation 22(6):365–372
Bunevicius A, Deltuva V, Tamasauskas S, Smith T, Laws E, Bunevicius R et al (2016) Preoperative low tri-iodothyronine concentration is associated with worse health status and shorter five year survival of primary brain tumor patients. Oncotarget 8(5):8648–8656
Bunevicius A, Deltuva V, Laws E, Iervasi G, Tamsauskas A, Bunevicius R (2017) Preoperative N-terminal pro-B-type natriuretic peptide concertation and prognosis of brain tumor patients: a 5-year follow up study. Sci Rep 7(1):1–8
Casati A, Fanelli G, Pietropaoli P, Proietti R, Tufano R, Montanini S et al (2007) Monitoring cerebral oxygen saturation in elderly patients undergoing general abdominal surgery. Eur J Anaesthesiol 24(1):59–65
Chen L, Xu M, Li G, Cai W, Zhou J (2014) Incidence, risk factors and consequences of emergence agitation in adult patients after elective craniotomy for brain tumor: a prospective cohort study. PLoS One 9(12):1–15
Choi Y, Kim D, Kim T, Lim T, Kim S, Yoo J (2017) Early postoperative delirium after hemiarthroplasty in elderly patients aged over 70 years with displaced femoral neck fracture. Clin Interv Aging 12:1835–1842
Crocker E, Beggs T, Hassan A et al (2016) Long-term effects of postoperative delirium in patients undergoing cardiac operation: a systematic review. Ann Thorac Surg 102(4):1391–1399
Elsamadicy AA, Adogwa O, Lydon E, Sergesketter A, Kaakati R, Mehta AI et al (2017) Depression as an independent predictor of postoperative delirium in spine deformity patients undergoing elective spine surgery. J Neurosurg Spine 27(2):209–214
Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R et al (2001) Evaluation of delirium in critically ill patients: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med 29(7):1370–1379
Filley C, Kleinschmidt-Demasters B (1995) Neurobehavioral presentations of brain neoplasms. West J Med 163(1):19–25
Fineberg SJ, Nandyala SV, Oglesby M, Patel AA, Singh K, Marquez-Lara A et al (2013) Incidence and risk factors for postoperative delirium after lumbar spine surgery. Spine 38(20):1790–1796
Flanigan P, Jahangiri A, Weinstein D et al (2018) Postoperative delirium in glioblastoma patients: risk factors and prognostic implications. Neurosurgery. https://doi.org/10.1093/neuros/nyx606
Fong TG, Hshieh TT, Wong B, Tommet D, Jones RN, Schmitt EM et al (2015) Neuropsychological profiles of an elderly cohort undergoing elective surgery and the relationship between cognitive performance and delirium. J Am Geriatr Soc 63(5):977–982
Inouye SK, Robinson T, Blaum C et al (2014) American geriatrics society abstracted clinical practice guideline for postoperative delirium in older adults. J Am Geriatr Soc 63(1):142–150
Jennett B (1975) Assessment of outcome after severe brain damage: a practical scale. Lancet 305(7905):480–484
Jeong JH, Seo YH, Ahn JY, Kim KH, Seo JY, Kim MJ et al (2016) The prognostic value of serum levels of heart-type fatty acid binding protein and high sensitivity C-reactive protein in patients with increased levels of amino-terminal pro-B type natriuretic peptide. Ann Lab Med 36(5):420–426
Jiang X, Chen D, Lou Y, Li Z (2016) Risk factors for postoperative delirium after spine surgery in middle- and old-aged patients. Aging Clin Exp Res 29(5):1039–1044
Kobayashi K, Imagama S, Ando K et al (2017) Risk factors for delirium after spine surgery in extremely elderly patients aged 80 years or older and review of the literature: Japan Association of Spine Surgeons with Ambition Multicenter Study. Glob spine J 7(6):560–566
Krzych ŁJ, Szurlej D, Kołodziej T, Machej L, Węglarzy A, Błach A et al (2018) Diagnostic accuracy of pre−operative NT−proBNP level in predicting short−term outcomes in coronary surgery: a pilot study. Kardiol Pol 69(11):1121–1127
Lenehan M, Summers M, Saunders N, Summers J, Vickers J (2014) Relationship between education and age-related cognitive decline: a review of recent research. Psychogeriatrics 15(2):154–162
Madeira T, Peixoto-Plácido C, Goulão B et al (2016) National survey of the Portuguese elderly nutritional status: study protocol. BMC Geriatr 16(1):1–9
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Mor V, Laliberte L, Morris J, Wiemann M (1984) The Karnofsky performance status scale: an examination of its reliability and validity in a research setting. Cancer 53(9):2002–2007
Nazemi A, Gowd A, Carmouche J, Kates S, Albert T, Behrend C (2017) Prevention and management of postoperative delirium in elderly patients following elective spinal surgery. Clin Spine Surg 30(3):112–119
Nishizawa Y, Hata T, Takemasa I et al (2017) Clinical benefits of single-incision laparoscopic surgery for postoperative delirium in elderly colon cancer patients. Surg Endosc 32(3):1434–1440
Oldroyd C, Scholz A, Hinchliffe R, McCarthy K, Hewitt J, Quinn T (2017) A systematic review and meta-analysis of factors for delirium in vascular surgical patients. J Vasc Surg 66(4):1269–1279.e9
Raats J, Steunenberg S, de Lange D, van der Laan L (2016) Risk factors of post-operative delirium after elective vascular surgery in the elderly: a systematic review. Int J Surg 35:1–6
Saporito A, Sturini E (2013) Incidence of postoperative delirium is high even in a population without known risk factors. J Anesth 28(2):198–201
Scholz A, Oldroyd C, McCarthy K, Quinn T, Hewitt J (2015) Systematic review and meta-analysis of risk factors for postoperative delirium among older patients undergoing gastrointestinal surgery. Br J Surg 103(2):e21–e28
Shi C, Yang C, Gao R, Yuan W (2015) Risk factors for delirium after spinal surgery: a meta-analysis. World Neurosurg 84(5):1466–1472
Snaith R, Zigmond A (1986) The hospital anxiety and depression scale. BMJ 292(6516):344–344
Takeuchi M, Takeuchi H, Fujisawa D et al (2012) Incidence and risk factors of postoperative delirium in patients with esophageal cancer. Ann Surg Oncol 19(12):3963–3970
Ushida T, Yokoyama T, Kishida Y et al (2009) Incidence and risk factors of postoperative delirium in cervical spine surgery. Spine 34(23):2500–2504
Valenzuela MJ, Sachdev P (2005) Brain reserve and dementia: a systematic review. Psychol Med 36(04):441–454
van den Boogaard M, Schoonhoven L, van der Hoeven J, van Achterberg T, Pickkers P (2012) Incidence and short-term consequences of delirium in critically ill patients: a prospective observational cohort study. Int J Nurs Stud 49(7):775–783
van Swieten J, Koudstaal P, Visser M, Schouten H, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19(5):604–607
Vasunilashorn S, Dillon S, Inouye S et al (2017) High C-reactive protein predicts delirium incidence, duration, and feature severity after major noncardiac surgery. J Am Geriatr Soc 65(8):e109–e116
Wang L, Xu D, Wei X, Chang H, Xu G (2016) Electrolyte disorders and aging: risk factors for delirium in patients undergoing orthopedic surgeries. BMC Psychiatry 16(1):418
Acknowledgments
We would like to thank Dr. Marius Rimaitis, M.D., for his consultations regarding anesthesiology section of the paper.
Funding
The study was financially supported by the Research Council of Lithuania (grant number: MIP-044/2015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all patients included in the study.
Additional information
Comments
This study indicates that postoperative delirium occurs after surgery for brain tumours, albeit infrequently. Also, demographic rather than tumour-related factors are associated with the occurrence. Since the patients’ performance level was assessed at discharge, this study is unlikely to say much about how postoperative delirium affects long-term performance.
Kirsten Moeller
Denmark
This article is part of the Topical Collection on Brain Tumors
Rights and permissions
About this article
Cite this article
Budėnas, A., Tamašauskas, Š., Šliaužys, A. et al. Incidence and clinical significance of postoperative delirium after brain tumor surgery. Acta Neurochir 160, 2327–2337 (2018). https://doi.org/10.1007/s00701-018-3718-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3718-2