Abstract
Purpose
Postoperative delirium is a recognized complication in populations at risk. The aim of this study is to assess the prevalence of early postoperative delirium in a population without known risk factors admitted to the ICU for postoperative monitoring after elective major surgery. The secondary outcome investigated is to identify eventual independent risk factors among demographic data and anesthetic drugs used.
Methods
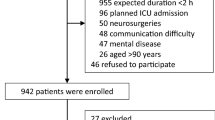
An observational, prospective study was conducted on a consecutive cohort of patients admitted to our ICU within and for at least 24 h after major surgical procedures. Exclusion criteria were any preexisting predisposing factor for delirium or other potentially confounding neurological dysfunctions. Patients were assessed daily using the confusion assessment method for the ICU scale for 3 days after the surgical procedure. Early postoperative delirium incidence risk factors were then assessed through three different multiple regression models.
Results
According to the confusion assessment method for the ICU scale, 28 % of patients were diagnosed with early postoperative delirium. The use of thiopentone was significantly associated with an eight-fold-higher risk for delirium compared to propofol (57.1 % vs. 7.1 %, RR = 8.0, χ 2 = 4.256; df = 1; 0.05 < p < 0.02).
Conclusion
In this study early postoperative delirium was found to be a very common complication after major surgery, even in a population without known risk factors. Thiopentone was independently associated with an increase in its relative risk.
Similar content being viewed by others
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th edn (DSM IV). Washington, DC: American Psychiatric Association; 1994.
Meagher DJ, O'Hanlon D, O'Mahony E, Casey PR, Trzepacz PT. Relationship between symptoms and motoric subtype of delirium. J Neuropsychiatry Clin Neurosci. 2000;12:51–6.
Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalised elderly medical patients. Am J Med. 1994;97:278–88.
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, Hart RP, Dittus R. Delirium in mechanically ventilated patients: validity and reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). JAMA. 2001;286:2703–10.
Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautam S, Bernard GR, Inouye SK. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med. 2001;29:1370–9.
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27:859–64.
McNicoll L, Pisani MA, Zhang Y, Ely EW, Siegel MD, Inouye SK. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51:591–8.
Thomas RI, Cameron DJ, Fahs MC. A prospective study of delirium and prolonged hospital stay. Arch Gen Psychiatry. 1988;45:937–40.
Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13:234–42.
American Psychiatric Association. Practice guidelines for the treatment of patients with delirium. Am J Psychiatry. 1999;156:1–20.
Pandharipande P, Jackson J, Ely EW. Delirium: acute cognitive dysfunction in the critically ill. Curr Opin Crit Care. 2005;11:360–8.
Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalised elderly patients: predictive model and interrelationship with the baseline vulnerability. JAMA. 1996;275:852–7.
Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalised elderly. JAMA. 1990;263:1097–101.
Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, Truman B, Dittus R, Bernard R, Inouye SK. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001;27:1892–900.
Blachly P, Starr A. Post-cardiotomy delirium. Am J Psychiatry. 1964;121:371–5.
Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, Aggarwal A, Marschall K, Graham SH, Ley C. Adverse cerebral outcomes after coronary bypass surgery. Multicenter study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. NEJM. 1996;335:1857–63.
Layne O, Yudofsky S. Postoperative psychosis in cardiotomy patients. N Engl J Med. 1971;284(10):518–20.
Sadler P. Incidence, degree and duration of postcardiotomy delirium. Heart Lung. 1981;10(6):1084–92.
Herrmann M, Ebert AD, Tober D, Hann J, Huth C. A contrastive analysis of release patterns of biochemical markers of brain damage after coronary artery bypass grafting and valve replacement and their association with the neurobehavioral outcome after cardiac surgery. Eur J Cardiothor Surg. 1999;16:513–8.
Kazmierski J, Kowman M, Banach M, Pawelczyk T, Okonski P, Iwaszkiewicz A, Zaslonka J, Sobow T, Kloszewska I. Incidence of and preoperative predictors for delirium after cardiac surgery. J Psychosom Res. 1999;46(5):479–83.
Sockalingam S, Parekh N, Bogoch II, Sun J, Mahtani R, Beach C, Bollegalla N, Turzanski S, Seto E, Kim J, Dulay P, Scarrow S, Bhalerao S. Delirium in the postoperative cardiac patient: a review. J Cardiac Surg. 2005;20:560–7.
Litaker D, Locala J, Franco K, Bronson DL, Tannous Z. Preoperative risk factors for postoperative delirium. Gen Hosp Psychiatry. 2001;23:84–9.
Dyer CB, Ashton CM, Teasdale TA. Postoperative delirium: a review of 80 primary data-collection studies. Arch Intern Med. 1995;155:461–5.
Wang H, Wang G, Wang C, Wei Y, Wen Z, Wang C, Zhu A. The early stage formation of PI3K-AMPAR GluR2 subunit complex facilitates the long-term neuroprotection induced by propofol post-conditioning in rats. PLoS One. 2013;8(6):e65187.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Saporito, A., Sturini, E. Incidence of postoperative delirium is high even in a population without known risk factors. J Anesth 28, 198–201 (2014). https://doi.org/10.1007/s00540-013-1706-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-013-1706-5