Abstract
Background
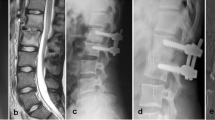
To date, there is growing consensus that PEEK material may be used for interbody fusion in spinal infections. Data supporting that claim are however restricted to a few very small clinical series. The aim of this study is to evaluate the outcome of surgical treatment of pyogenic spinal infections with PEEK cages in combination with posterior pedicel screw fixation.
Methods
Between 2006 and 2013, a total of 211 patients suffering from spondylodiscitis underwent surgical debridement and instrumentation. There were 52 cases where PEEK cages were used. Laboratory and physical examinations were assessed at a 3-month follow-up. Last follow-up was performed with at a minimum of 12 months after surgery via a telephone interview.
Results
Mean age at presentation was 67 years, with 19 (37 %) male patients and 33 (63 %) female. Distribution of the infection was lumbar in 29 (56 %%), thoracic in 3 (6 %) and cervical in 11 (21 %) cases. Nine patients (17 %) had concomitant non-contiguous spondylodiscitis. Epidural abscess was found in 17 patients (33 %); 48 (92 %%) had pain; neurological deficits were found in 20 patients (38 %). All patients in this series underwent surgical debridement with instrumentation of the spine. Postoperative intravenous antibiotics were administered for 15.4 ± 6.8 days followed by 2.9 ± 0.5 months of oral antibiotics. Complete resolution of the infection was achieved in all cases. Of the 28 patients with neurological deficits, 6 had full recovery and 10 had improved incompletely after surgery. One patient suffered from a pulmonary embolism postoperatively. There were no mortalities.
Conclusions
Use of PEEK cages for interbody fusion is feasible and safe in patients suffering from a pyogenic spinal infection.



Similar content being viewed by others
References
Belzunegui J, Intxausti JJ, De Dios JR, Del Val N, Rodriguez Valverde V, Gonzalez C, Queiro R, Figueroa M (2000) Haemtigenous vertebral osteomyelitis in the elderly. Clin Rheumatol 19:344–347
Berbari EF, Kanj SS, Kowalski TJ, Darouiche RO, Widmer AF, Schmitt SK, Hendershot EF, Holtom PD, Huddleston PM 3rd, Petermann GW, Osmon DR (2015) Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Clin Infect Dis 61:e26–e46
Bernard L, Dinh A, Ghout I, Simo D, Zeller V, Issartel B, Le Moing V, Belmatoug N, Lesprit P, Bru JP, Therby A, Bouhour D, Dénes E, Debard A, Chirouze C, Fèvre K, Dupon M, Aegerter P, Mulleman D, Duration of Treatment for Spondylodiscitis (DTS) study group (2015) Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Lancet 385(9971):875–882
Brantigan JW, Steffee AD, Lewis ML, Quinn LM, Persenaire JM (2000) Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system: two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine (Phila Pa 1976) 25:1437–1446
Brase A, Ringel F, Stüer C, Meyer B, Stoffel M (2010) Debridement and fusion with polyetheretherketone implants in purulent spondylodiscitis: a clinical experience with nine patients. Acta Neurochir (Wien) 152:2001–2004
Chou YC, Chen DC, Hsieh WA, Chen WF, Yen PS, Harnod T, Chiou TL, Chang YL, Su CF, Lin SZ, Chen SY (2008) Efficacy of anterior cervical fusion: comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci 15:1240–1245
Cutler AR, Siddiqui S, Mohan AL, Hillard VH, Cerabona F, Das K (2006) Comparison of polyetheretherketone cages with femoral cortical bone allograft as a single- piece interbody spacer in transforaminal lumbar interbody fusion. J Neurosurg Spine 5:534–539
Duarte RM, Vaccaro AR (2013) Spinal infection: state of the art and management algorithm. Eur Spine J 22:2787–2799
Gorth DJ, Puckett S, Ercan B, Webster TJ, Rahaman M, Bal BS (2012) Decreased bacteria activity on Si3N4 surfaces compared with PEEK or titanium. Int J Nanomedicine 7:4829–4840
Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ (2000) Haematogenous pyogenic spinal infections and their surgical management. Spine 25:1668–1679
Hahnel S, Wieser A, Lang R, Rosentritt M (2015) Biofilm formation on the surface of modern implant abutment materials. Clin Oral Implants Res 26:1297–1301
Kehrer M, Pedersen C, Jensen TG, Lassen AT (2014) Increasing incidence of pyogenic spondylodiscitis: a 14-year population-based study. J Infect 68:313–320
Linhardt O, Matussek J, Refior HJ, Krödel A (2007) Long-term results of ventro-dorsal versus ventral instrumentation fusion in the treatment of spondylitis. Int Orthop 31:113–119
Mondorf Y, Gaab MR, Oertel JM (2009) PEEK cage cervical ventral fusion in spondylodiscitis. Acta Neurochir (Wien) 151:1537–1541
Murillo O, Grau I, Lora-Tamayo J, Gomez-Junyent J, Ribera A, Tubau F, Ariza J, Pallares R (2015) The changing epidemiology of bacteraemic osteoarticular infections in the early 21st century. Clin Microbiol Infect 3:254.e1-8
Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A (2009) Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum 39:10–17
Patel NB, Dodd ZH, Voorhies J, Horn EM (2015) Minimally invasive lateral transpsoas approach for spinal discitis and osteomyelitis. J Clin Neurosci 22(11):1753–1757
Pee YH, Park JD, Choi YG, Lee SH (2008) Anterior debridement and fusion followed by posterior pedicle screw fixation in pyogenic spondylodiscitis: autologous iliac bone strut versus cage. J Neurosurg Spine 8:405–412
Pigrau C, Almirante B, Flores X, Falco V, Rodríguez D, Gasser I, Villanueva C, Pahissa A (2005) Spontaneous pyogenic vertebral osteomyelitis and endocarditis: incidence, risk factors, and outcome. Am J Med 118:1287
Pola E, Rossi B, Nasto LA, Colangelo D, Logroscino CA (2012) Surgical treatment of tuberculous spondylodiscitis. Eur Rev Med Pharmacol Sci 6(Suppl 2):79–85
Przybylski GJ, Sharan AD (2001) Single-stage autogenous bone grafting and internal fixation in the surgical management of pyogenic discitis and vertebral osteomyelitis. J Neurosurg Spine 94:1–7
Rochford ET, Poulsson AH, Salavarrieta Varela J, Lezuo P, Richards RG, Moriarty TF (2014) Bacterial adhesion to orthopaedic implant materials and a novel oxygen plasma modified PEEK surface. Colloids Surf B: Biointerfaces 113:213–222
Rutges JP, Kempen DH, van Dijk M, Oner FC (2016) Outcome of conservative and surgical treatment of pyogenic spondylodiscitis: a systematic literature review. Eur Spine J 25(4):983–999
Sakkas LI, Davas EM, Kapsalaki E, Boulbou M, Makaritsis K, Alexiou I, Tsikrikas T, Stathakis N (2009) Hematogenous spinal infection in central Greece. Spine (Phila Pa 1976) 34:E513–E518
Schomacher M, Finger T, Koeppen D, Süss O, Vajkoczy P, Kroppenstedt S, Cabraja M (2014) Application of titanium and polyetheretherketone cages in the treatment of pyogenic spondylodiscitis. Clin Neurol Neurosurg 127:65–70
Shiban E, Janssen I, Wostrack M, Krieg SM, Horanin M, Stoffel M, Meyer B, Ringel F (2014) Spondylodiscitis by drug-multiresistant bacteria: a single-center experience of 25 cases. Spine J 14:2826–2834
Shiban E, Janssen I, Wostrack M, Krieg SM, Ringel F, Meyer B (2014) A retrospective study of 113 consecutive cases of surgically treated spondylodiscitis patients. A single-center experience. Acta Neurochir 156:1189–1196
Sobottke R, Csecsei G, Kaulhausen T, Delank S, Franklin J, Aghayev E, Zweig T, Eysel P (2008) Spinal surgery in the elderly: does age have an influence on the complication rate? Orthopade 37:367–373
Stoffel M, Stüer C, Ringel F, Meyer B (2011) Treatment of infections of the spine. Adv Tech Stand Neurosurg 37:213–243
Stüer C, Stoffel M, Hecker J, Ringel F, Meyer B (2013) A staged treatment algorithm for spinal infections. J Neurol Surg A Cent Eur Neurosurg 74:87–95
Tschöke SK, Fuchs H, Schmidt O, Gulow J, von der Hoeh NH, Heyde CE (2015) Single-stage debridement and spinal fusion using PEEK cages through a posterior approach for eradication of lumbar pyogenic spondylodiscitis: a safe treatment strategy for a detrimental condition. Patient Saf Surg 9:35
Valancius K, Hansen ES, Høy K, Helmig P, Niedermann B, Bünger C (2012) Failure modes in conservative and surgical management of infectious spondylodiscitis. Eur Spine J 22:1837–1844
Walter J, Kuhn SA, Reichart R, Kalff R, Ewald C (2010) PEEK cages as a potential alternative in the treatment of cervical spondylodiscitis: a preliminary report on a patient series. Eur Spine J 19:1004–1009
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Disclosure
The study was completly financed by the department of neurosurgery of technical university of munich.
Additional information
Ehab Shiban and Insa Janssen contributed equally to this work.
Rights and permissions
About this article
Cite this article
Shiban, E., Janssen, I., da Cunha, P.R. et al. Safety and efficacy of polyetheretherketone (PEEK) cages in combination with posterior pedicel screw fixation in pyogenic spinal infection. Acta Neurochir 158, 1851–1857 (2016). https://doi.org/10.1007/s00701-016-2924-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2924-z