Abstract
Background
To prevent iatrogenic damage, transfusions of red blood cells should be avoided. For this, specific and reliable transfusion triggers must be defined. To date, the optimal hematocrit during the initial operating room (OR) phase is still unclear in patients with severe traumatic brain injury (TBI). We hypothesized that hematocrit values exceeding 28%, the local hematocrit target reached by the end of the initial OR phase, resulted in more complications, increased mortality, and impaired recovery compared to patients in whom hematocrit levels did not exceed 28%.
Methods
Impact of hematocrit (independent variable) reached by the end of the OR phase on mortality and morbidity determined by the extended Glasgow outcome scale (eGOS; dependent variables) was investigated retrospectively in 139 TBI patients. In addition, multiple logistic regression analysis was performed to identify additional important variables.
Findings
Following severe TBI, mortality and morbidity were neither aggravated by hematocrit above 28% reached by the end of the OR phase nor worsened by the required transfusions. Upon multiple logistic regression analysis, eGOS was significantly influenced by the highest intracranial pressure and the lowest cerebral perfusion pressure values during the initial OR phase.
Conclusions
Based on this retrospective observational analysis, increasing hematocrit above 28% during the initial OR phase following severe TBI was not associated with improved or worsened outcome. This questions the need for aggressive transfusion management. Prospective analysis is required to determine the lowest acceptable hematocrit value during the OR phase which neither increases mortality nor impairs recovery. For this, a larger caseload and early monitoring of cerebral metabolism and oxygenation are indispensable.



Similar content being viewed by others
Abbreviations
- CPP:
-
Cerebral perfusion pressure
- FFP:
-
Fresh frozen plasma
- ICP:
-
Intracranial pressure
- ICU:
-
Intensive care unit
- RBC:
-
Red blood cells
- TBI:
-
Traumatic brain injury
References
Carlson AP, Schermer CR, Lu SW (2006) Retrospective evaluation of anemia and transfusion in traumatic brain injury. J Trauma 61:567–571
Cherry T, Steciuk M, Reddy VV, Marques MB (2008) Transfusion-related acute lung injury: past, present, and future. Am J Clin Pathol 129:287–297
Corwin HL, Gettinger A, Pearl RG, Fink MP, Levy MM, Abraham E, MacIntyre NR, Shabot MM, Duh MS, Shapiro MJ (2004) The CRIT Study: anemia and blood transfusion in the critically ill—current clinical practice in the United States. Crit Care Med 32:39–52
Duchesne JC, Hunt JP, Wahl G, Marr AB, Wang YZ, Weintraub SE, Wright MJ, McSwain NE Jr (2008) Review of current blood transfusions strategies in a mature level I trauma center: were we wrong for the last 60 years? J Trauma 65:272–276
Ekelund A, Reinstrup P, Ryding E, Andersson AM, Molund T, Kristiansson KA, Romner B, Brandt L, Säveland H (2002) Effects of iso- and hypervolemic hemodilution on regional cerebral blood flow and oxygen delivery for patients with vasospasm after aneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien) 144:703–712
Frietsch T, Lenz C, Kuschinsky W, Waschke KE (2004) Effects of chronic isovolaemic haemodilution on regional cerebral blood flow in conscious rats. Eur J Anaesthesiol 21:53–59
Ge YL, Lv R, Zhou W, Ma XX, Zhong TD, Duan ML (2007) Brain damage following severe acute normovolemic hemodilution in combination with controlled hypotension in rats. Acta Anaesthesiol Scand 51:1331–1337
George ME, Skarda DE, Watts CR, Pham HD, Beilman GJ (2008) Aggressive red blood cell transfusion: no association with improved outcomes for victims of isolated traumatic brain injury. Neurocrit Care 8:337–343
Gonzalez AM, Yazici I, Kusza K, Siemionow M (2007) Effects of fresh versus banked blood transfusions on microcirculatory hemodynamics and tissue oxygenation in the rat cremaster model. Surgery 141:630–639
Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah A (2003) Adverse effects of low hematocrit during cardiopulmonary bypass in the adult: should current practice be changed? J Thorac Cardiovasc Surg 125:1438–1450
Han SH, Ham BM, Oh YS, Bahk JH, Ro YJ, Do SH, Park YS (2004) The effect of acute normovolemic haemodilution on cerebral oxygenation. Int J Clin Pract 58:903–906
Hare GM, Mazer CD, Hutchison JS, McLaren AT, Liu E, Rassouli A, Ai J, Shaye RE, Lockwood JA, Hawkins CE, Sikich N, To K, Baker AJ (2007) Severe hemodilutional anemia increases cerebral tissue injury following acute neurotrauma. J Appl Physiol 103:1021–1029
Hébert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 340:409–417
Klein HG, Spahn DR, Carson JL (2007) Red blood cell transfusion in clinical practice. Lancet 370:415–426
Kroppenstedt SN, Thomale UW, Griebenow M, Sakowitz OW, Schaser KD, Mayr PS, Unterberg AW, Stover JF (2003) Effects of early and late intravenous norepinephrine infusion on cerebral perfusion, microcirculation, brain-tissue oxygenation, and edema formation in brain-injured rats. Crit Care Med 31:2211–2221
Leal-Noval SR, Muñoz-Gómez M, Arellano-Orden V, Marín-Caballos A, Amaya-Villar R, Marín A, Puppo-Moreno A, Ferrándiz-Millón C, Flores-Cordero JM, Murillo-Cabezas F (2008) Impact of age of transfused blood on cerebral oxygenation in male patients with severe traumatic brain injury. Crit Care Med 36:1290–1296
Leal-Noval SR, Múñoz-Gómez M, Murillo-Cabezas F (2008) Optimal hemoglobin concentration in patients with subarachnoid hemorrhage, acute ischemic stroke and traumatic brain injury. Curr Opin Crit Care 14:156–162
Leal-Noval SR, Rincón-Ferrari MD, Marin-Niebla A, Cayuela A, Arellano-Orden V, Marín-Caballos A, Amaya-Villar R, Ferrándiz-Millón C, Murillo-Cabeza F (2006) Transfusion of erythrocyte concentrates produces a variable increment on cerebral oxygenation in patients with severe traumatic brain injury: a preliminary study. Intensive Care Med 32:1733–1740
Madjdpour C, Spahn DR, Weiskopf RB (2006) Anemia and perioperative red blood cell transfusion: a matter of tolerance. Crit Care Med 34(5 Suppl):S102–S108
Marik PE, Corwin HL (2008) Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med 36:2667–2674
McHugh GS, Engel DC, Butcher I, Steyerberg EW, Lu J, Mushkudiani N, Hernández AV, Marmarou A, Maas AI, Murray GD (2007) Prognostic value of secondary insults in traumatic brain injury: results from the IMPACT study. J Neurotrauma 24:287–293
McIntyre LA, Fergusson DA, Hutchison JS, Pagliarello G, Marshall JC, Yetisir E, Hare GM, Hébert PC (2006) Effect of a liberal versus restrictive transfusion strategy on mortality in patients with moderate to severe head injury. Neurocrit Care 5:4–9
McIntyre LA, Hebert PC (2006) Can we safely restrict transfusion in trauma patients? Curr Opin Crit Care 12:575–583
McIntyre L, Hebert PC, Wells G, Fergusson D, Marshall J, Yetisir E, Blajchman MJ, Canadian Critical Care Trials Group (2004) Is a restrictive transfusion strategy safe for resuscitated and critically ill trauma patients? J Trauma 57:563–568
Meier R, Béchir M, Ludwig S, Sommerfeld J, Keel M, Steiger P, Stocker R, Stover JF (2008) Differential temporal profile of lowered blood glucose levels (3.5 to 6.5 mmol/l versus 5 to 8 mmol/l) in patients with severe traumatic brain injury. Crit Care 12:R98
Meixensberger J, Kunze E, Barcsay E, Vaeth A, Roosen K (2001) Clinical cerebral microdialysis: brain metabolism and brain tissue oxygenation after acute brain injury. Neurol Res 23:801–806
Meixensberger J, Renner C, Simanowski R, Schmidtke A, Dings J, Roosen K (2004) Influence of cerebral oxygenation following severe head injury on neuropsychological testing. Neurol Res 26:414–417
Rosenthal G, Hemphill JC, Sorani M, Martin C, Morabito D, Meeker M, Wang V, Manley GT (2008) The role of lung function in brain tissue oxygenation following traumatic brain injury. J Neurosurg 108:59–65
Sarrafzadeh AS, Kiening KL, Callsen TA, Unterberg AW (2003) Metabolic changes during impending and manifest cerebral hypoxia in traumatic brain injury. Br J Neurosurg 17:340–346
Smith MJ, Stiefel MF, Magge S, Frangos S, Bloom S, Gracias V, Le Roux PD (2005) Packed red blood cell transfusion increases local cerebral oxygenation. Crit Care Med 33:1104–1108
Thomale UW, Bender M, Casalis P, Rupprecht S, Griebenow M, Neumann K, Woiciechowsky C, Unterberg AW, Stover JF (2007) Tacrolimus depresses local immune cell infiltration but fails to reduce cortical contusion volume in brain-injured rats. Immunobiology 212:567–576
Thomale UW, Kroppenstedt SN, Beyer TF, Schaser KD, Unterberg AW, Stover JF (2002) Temporal profile of cortical perfusion and microcirculation after controlled cortical impact injury in rats. J Neurotrauma 19:403–413
Tinmouth A, Fergusson D, Yee IC, Hébert PC, ABLE Investigators; Canadian Critical Care Trials Group (2006) Clinical consequences of red cell storage in the critically ill. Transfusion 46:2014–2027
Tomiyama Y, Brian JE Jr, Todd MM (2000) Plasma viscosity and cerebral blood flow. Am J Physiol Heart Circ Physiol 279:H1949–H1954
Tomiyama Y, Jansen K, Brian JE Jr, Todd MM (1999) Hemodilution, cerebral O2 delivery, and cerebral blood flow: a study using hyperbaric oxygenation. Am J Physiol 276:H1190–H1196
Treggiari MM, Schutz N, Yanez ND, Romand JA (2007) Role of intracranial pressure values and patterns in predicting outcome in traumatic brain injury: a systematic review. Neurocrit Care 6:104–112
Tsai AG, Cabrales P, Intaglietta M (2004) Microvascular perfusion upon exchange transfusion with stored red blood cells in normovolemic anemic conditions. Transfusion 44:1626–1634
Tschuor C, Asmis LM, Lenzlinger PM, Tanner M, Härter L, Keel M, Stocker R, Stover JF (2008) In vitro norepinephrine significantly activates isolated platelets from healthy volunteers and critically ill patients following severe traumatic brain injury. Crit Care 12:R80
Van Beek JG, Mushkudiani NA, Steyerberg EW, Butcher I, McHugh GS, Lu J, Marmarou A, Murray GD, Maas AI (2007) Prognostic value of admission laboratory parameters in traumatic brain injury: results from the IMPACT study. J Neurotrauma 24:315–328
van Bommel J, Trouwborst A, Schwarte L, Siegemund M, Ince C, Henny ChP (2002) Intestinal and cerebral oxygenation during severe isovolemic hemodilution and subsequent hyperoxic ventilation in a pig model. Anesthesiology 97:660–670
Vincent JL, Baron JF, Reinhart K, Gattinoni L, Thijs L, Webb A, Meier-Hellmann A, Nollet G, Peres-Bota D, ABC (Anemia and Blood Transfusion in Critical Care) Investigators (2002) Anemia and blood transfusion in critically ill patients. JAMA 288:1499–1507
Weinberg JA, McGwin G Jr, Griffin RL, Huynh VQ, Cherry SA 3rd, Marques MB, Reiff DA, Kerby JD, Rue LW 3rd (2008) Age of transfused blood: an independent predictor of mortality despite universal leukoreduction. J Trauma 65:279–282
Weiskopf RB, Feiner J, Hopf H, Lieberman J, Finlay HE, Quah C, Kramer JH, Bostrom A, Toy P (2006) Fresh blood and aged stored blood are equally efficacious in immediately reversing anemia-induced brain oxygenation deficits in humans. Anesthesiology 104:911–920
Weiskopf RB, Kramer JH, Viele M, Neumann M, Feiner JR, Watson JJ, Hopf HW, Toy P (2000) Acute severe isovolemic anemia impairs cognitive function and memory in humans. Anesthesiology 92:1646–1652
Weiskopf RB, Toy P, Hopf HW, Feiner J, Finlay HE, Takahashi M, Bostrom A, Songster C, Aminoff MJ (2005) Acute isovolemic anemia impairs central processing as determined by P300 latency. Clin Neurophysiol 116:1028–1032
Zauner A, Daugherty WP, Bullock MR, Warner DS (2002) Brain oxygenation and energy metabolism: part I-biological function and pathophysiology. Neurosurgery 51:289–301
Acknowledgements
The help of the ER and ICU nursing staff in collecting clinical data is gratefully acknowledged.
Conflict of interest
None.
Funding
This study was supported in part by grants from the SUVA funds to JFS and RS.
Author information
Authors and Affiliations
Corresponding author
Additional information
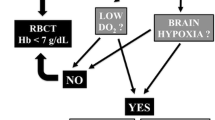
This paper addresses pertinent questions related with the acute, presumably cranial and extracranial, surgical management of traumatic brain injury (TBI) patients. How tolerable is the blood loss, due to traumatic loss or bleeding during surgical procedures, either in terms of blood volume or hemoglobin levels, without jeopardizing brain oxygen supply and, consequently, outcome? In addition, which objectives should be aimed for if the patient should be transfused?
The study design is very similar to the design of Clifton hypothermia trial, as it divides TBI patients in two predefined clusters based on the initial hematocrit level, using a hematocrit 28% as a cut-off. Further exploring the similitude between these two studies, it also evaluates the impact of blood transfusion or abstention of transfusion, in both cohorts of patients.
This study accrues a significant number of patients, and the statistical analysis is very robust, which altogether confers a considerable power to the conclusions. As shown by previous research, it demonstrates that substrate delivery, including oxygen, may not be the main problem in TBI pathophysiology, reason why increasing hematocrit, and thus oxygen-carrying capacity, is not necessarily associated with a decrease in morbidity and mortality.
In normal physiological conditions, the maximal capacity of oxygen transport and unload to the brain is achieved at a hemoglobin level around 10 mg/dl. In head-injured patients, this axiom is probably questionable because the injury itself carries changes in patterns of oxygen delivery and consumption, as well as cerebral microcirculation. Many of these patients are either on increased inspired fraction of oxygen or under the effect of drugs, as mannitol, that have favorable rheological properties, or are sedated to improve the flow/metabolism mismatch. Furthermore, the occurrence of extracranial injuries that often requires surgical repair adds to secondary brain lesions due to a higher incidence of hypoxia and hypotension in these patients.
I suppose that some interesting conclusions can be drawn from this study:
– It is better for head-injured patients if a blood transfusion is not needed.
– Raising the hematocrit is not a technical problem, but it does not translate into an increased outcome, probably because patients that need a transfusion are those with higher incidence of hypoxia and hypotension due to extracranial injuries or higher surgical blood loss. The importance of the severity of primary injuries is expressed in deceased patients with low hematocrit that fail to increase hematocrit with transfusion.
– As shown in the prolific Fig. 3, mortality tends to be higher in patients with low (28%) or in patients with higher (>36%) initial hematocrit levels, as well as mortality is independent of blood transfusion.
– The survival probability of non-transfused patient with <28% hematocrit by the end of the OR phase is similar to those transfused patients with >28% hematocrit, thus outshining the effect of transfusion on raising the hematocrit.
Oscar Alves
Porto, Portugal
Rights and permissions
About this article
Cite this article
Flückiger, C., Béchir, M., Brenni, M. et al. Increasing hematocrit above 28% during early resuscitative phase is not associated with decreased mortality following severe traumatic brain injury. Acta Neurochir 152, 627–636 (2010). https://doi.org/10.1007/s00701-009-0579-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-009-0579-8