Abstract
Purpose
Robotic lateral lymph node dissection (LLND) has been described as a safe and feasible procedure for local advanced rectal cancer. The aim of this study was to evaluate the learning curve for robotic-assisted LLND.
Methods
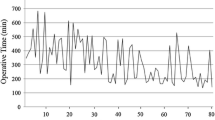
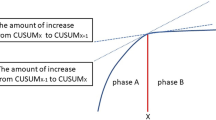
We collected data on 78 consecutive patients who underwent robotic-LLND at our hospital. The learning curve was analyzed using the cumulative sum (CUSUM) method to assess changes in the unilateral LLND operative times across the case sequence.
Results
Among the 78 patients, 52 underwent bilateral LLND and 26 underwent unilateral LLND. A total of 130 consecutive data were recorded. We arranged unilateral robotic-LLND operative times and calculated cumulative sum values, allowing the differentiation of three phases: phase I (learning period, cases 1–51); phase II (proficiency period, cases 52–83); and phase III (mastery period, cases 84–130). As the learning curve accumulated, the operation time and estimated blood loss of unilateral robotic-LLND decreased significantly with each phase (P < 0.05). By 12 months after surgery, the International Prostatic Symptom Score of patients at phase III was significantly lower than at phase I (P < 0.05).
Conclusion
The CUSUM curve shows three phases in the learning of robotic-LLND. The estimated learning curve for robotic-assisted rectal-LLND is achieved after 51 cases.






Similar content being viewed by others
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- nCRT:
-
Neoadjuvant chemoradiotherapy
- TME:
-
Total mesorectal excision
- LR:
-
Local recurrence
- LLND:
-
Lateral lymph node dissection
- CUSUM:
-
Cumulative sum
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- LLNs:
-
Lateral lymph nodes
- IPSS:
-
International Prostatic Symptom Score
- OS:
-
Overall survival
- RFS:
-
Relapse-free survival
- ASA:
-
American Society of Anesthesiologist
- BMI:
-
Body mass index
References
Bosset J, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, et al. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006;355(11):1114–23.
El-Khoury T, Solomon M, Young J. The incidence of lateral pelvic side-wall nodal involvement in low rectal cancer may be similar in Japan and the West. Br J Surg. 2008;95(6):801–2.
Akiyoshi T, Ueno M, Matsueda K, Konishi T, Fujimoto Y, Nagayama S, et al. Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol. 2014;21(1):189–96.
Tomita N, Ishida H, Tanakaya K, Yamaguchi T, Kumamoto K, Tanaka T, et al. Japanese society for cancer of the colon and rectum (JSCCR) guidelines 2020 for the clinical practice of hereditary colorectal cancer. Int J Clin Oncol. 2021;26(8):1353–419.
Sugihara K, Kobayashi H, Kato T, Mori T, Mochizuki H, Kameoka S, et al. Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum. 2006;49(11):1663–72.
Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Kinugasa Y, Komori K, et al. Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg. 2017;266(2):201–7.
Fujita S, Akasu T, Mizusawa J, Saito N, Kinugasa Y, Kanemitsu Y, et al. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012;13(6):616–21.
Simillis C, Lal N, Thoukididou S, Kontovounisios C, Smith J, Hompes R, et al. Open versus laparoscopic versus robotic versus transanal mesorectal excision for rectal cancer: a systematic review and network meta-analysis. Ann Surg. 2019;270(1):59–68.
Nakanishi R, Yamaguchi T, Akiyoshi T, Nagasaki T, Nagayama S, Mukai T, et al. Laparoscopic and robotic lateral lymph node dissection for rectal cancer. Surg Today. 2020;50(3):209–16.
Gofton W, Papp S, Gofton T, Beaulé P. Understanding and taking control of surgical learning curves. Instr Course Lect. 2016;65:623–31.
Liu Q, Zhang T, Hu M, Zhao Z, Zhao G, Li C, et al. Comparison of the learning curves for robotic left and right hemihepatectomy: a prospective cohort study. Int J Surg. 2020;81:19–25.
Kim M, Kim W, Hyung W, Kim H, Han S, Kim Y, et al. Comprehensive learning curve of robotic surgery: discovery from a multicenter prospective trial of robotic gastrectomy. Ann Surg. 2021;273(5):949–56.
Zhang Y, Liu S, Han Y, Xiang J, Cerfolio R, Li H. Robotic anatomical segmentectomy: an analysis of the learning curve. Ann Thorac Surg. 2019;107(5):1515–22.
Hu C, Zhang Z, Zhang L, Liu R, Yan J, Sun Q, et al. Robot-assisted total mesorectal excision and lateral pelvic lymph node dissection for locally advanced middle-low rectal cancer. J Vis Exp: JoVE. 2022;12(180): e62919.
Yap CH, Colson ME, Watters DA. Cumulative sum techniques for surgeons: a brief review. ANZ J Surg. 2007;77(7):583–6.
Wong C, Choi E, Chan S, Tsu J, Fan C, Chu P, et al. Use of the International Prostate Symptom Score (IPSS) in Chinese male patients with benign prostatic hyperplasia. Aging Male. 2017;20(4):241–9.
Kawai K, Hata K, Tanaka T, Nishikawa T, Otani K, Murono K, et al. Learning curve of robotic rectal surgery with lateral lymph node dissection: cumulative sum and multiple regression analyses. J Surg Educ. 2018;75(6):1598–605.
Sukumar V, Kazi M, Gori J, Ankathi S, Baheti A, Ostwal V, et al. Learning curve analysis for lateral pelvic lymph node dissection in rectal cancers - outcomes improve with experience. Eur J Surg Oncol. 2022;48(5):1110–6.
Jiménez-Rodríguez R, Díaz-Pavón J, de Juan FP, Prendes-Sillero E, Dussort H, Padillo J. Learning curve for robotic-assisted laparoscopic rectal cancer surgery. Int J Colorectal Dis. 2013;28(6):815–21.
Parisi A, Scrucca L, Desiderio J, Gemini A, Guarino S, Ricci F, et al. Robotic right hemicolectomy: analysis of 108 consecutive procedures and multidimensional assessment of the learning curve. Surg Oncol. 2017;26(1):28–36.
Park S, Choi G, Park J, Kim H, Ryuk J, Yun S. Urinary and erectile function in men after total mesorectal excision by laparoscopic or robot-assisted methods for the treatment of rectal cancer: a case-matched comparison. World J Surg. 2014;38(7):1834–42.
Funding
This project was supported by the National Natural Science Foundation of China (No. 81870380) and Shaanxi Province Science Foundation (2023-GHYB-13).
Author information
Authors and Affiliations
Contributions
LZ was responsible for the design of the study, statistical analysis, and drafting and revising of the manuscript; CH was involved in the design of the study and provided critical comments and review of the manuscript; CH, QQ, RL, JZ, ZZ, and ZW provided critical comments and review of the manuscript; JS and FS designed and supervised the study and revised the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare.
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Xi’an Jiaotong University (No. 2019ZD04).
Informed consent
This was obtained from all participants in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, L., Hu, C., Qin, Q. et al. Learning process analysis of robotic lateral pelvic lymph node dissection for local advanced rectal cancer: the CUSUM curve of 78 consecutive patients. Surg Today 54, 220–230 (2024). https://doi.org/10.1007/s00595-023-02725-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02725-6