Abstract
Background
There is no clear evidence on the number of cases required to master the techniques required in robot-assisted surgery for different surgical fields and techniques. The purpose of this study was to clarify the learning curve of robot-assisted rectal surgery for malignant disease by surgical process.
Method
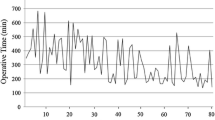
The study retrospectively analyzed robot-assisted rectal surgeries performed between April 2014 and July 2020 for which the operating time per process was measurable. The following learning curves were created using the cumulative sum (CUSUM) method: (1) console time required for total mesorectal excision (CUSUM tTME), (2) time from peritoneal incision to inferior mesenteric artery dissection (CUSUM tIMA), (3) time required to mobilize the descending and sigmoid colon (CUSUM tCM), and (4) time required to mobilize the rectum (CUSUM tRM). Each learning curve was classified into phases 1–3 and evaluated. A fifth learning curve was evaluated for robot-assisted lateral lymph node dissection (CUSUM tLLND).
Results
This study included 149 cases. Phase 1 consisted of 32 cases for CUSUM tTME, 30 for CUSUM tIMA, 21 for CUSUM tCM, and 30 for CUSUM tRM; the respective numbers were 54, 48, 45, and 61 in phase 2 and 63, 71, 83, and 58 in phase 3. There was no significant difference in the number of cases in each phase. Lateral lymph node dissection was initiated in the 76th case where robot-assisted rectal surgery was performed. For CUSUM tLLND, there were 12 cases in phase 1, 6 in phase 2, and 7 cases in phase 3.
Conclusions
These findings suggest that the learning curve for robot-assisted rectal surgery is the same for all surgical processes. Surgeons who already have adequate experience in robot-assisted surgery may be able to acquire stable technique in a smaller number of cases when they start to learn other techniques.




Similar content being viewed by others
References
Kang J, Yoon KJ, Min BS, Hur H, Baik SH, Kim NK, Lee KY (2013) The impact of robotic surgery for mid and low rectal cancer: a case-matched analysis of a 3-arm comparison–open, laparoscopic, and robotic surgery. Ann Surg 257:95–101
Dubeshter B, Angel C, Toy E, Thomas S, Glantz JC (2013) Current role of robotic hysterectomy. J Gynecol Surg 29:174–178
Coughlin GD, Yaxley JW, Chambers SK, Occhipinti S, Samaratunga H, Zajdlewicz L, Teloken P, Dunglison N, Williams S, Lavin MF, Gardiner RA (2018) Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: 24-month outcomes from a randomised controlled study. Lancet Oncol 19:1051–1060
Galata C, Vassilev G, Haas F, Kienle P, Büttner S, Reißfelder C, Hardt J (2019) Clinical, oncological, and functional outcomes of Da Vinci (Xi)-assisted versus conventional laparoscopic resection for rectal cancer: a prospective, controlled cohort study of 51 consecutive cases. Int J Colorectal Dis 34:1907–1914
Kestin IG (1995) A statistical approach to measuring the competence of anaesthetic trainees at practical procedures. Br J Anaesth 75:805–809
Cavill I (1971) Quality control in routine haemoglobinometry. J Clin Pathol 24:701–704
Yamaguchi T, Kinugasa Y, Shiomi A, Sato S, Yamakawa Y, Kagawa H, Tomioka H, Mori K (2015) Learning curve for robotic-assisted surgery for rectal cancer: use of the cumulative sum method. Surg Endosc 29:1679–1685
Bege T, Lelong B, Esterni B, Francon D, Turrini O, Guiramand J, Francon D, Mokart D, Houvenaeghel G, Giovannini M, Delpero JR (2010) The learning curve for the laparoscopic approach to conservative mesorectal excision for rectal cancer: lessons drawn from a single institution’s experience. Ann Surg 251:249–253
Jiménez-rodríguez RM, Díaz-pavón JM, de Juan FDLP, Prendes-Sillero E, Dussort HC, Padillo J (2013) Learning curve for robotic-assisted laparoscopic rectal cancer surgery. Int J Colorectal Dis 28:815–821
Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM (2011) Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc 25:855–860
Nasseri Y, Stettler I, Shen W, Zhu R, Alizadeh A, Lee A, Cohen J, Barnajian M (2021) Learning curve in robotic colorectal surgery. J Robot Surg 15:489–495
Parisi A, Scrucca L, Desiderio J, Gemini A, Guarino S, Ricci F, Cirocchi R, Palazzini G, D’Andrea V, Minelli L, Trastulli S (2017) Robotic right hemicolectomy: analysis of 108 consecutive procedures and multidimensional assessment of the learning curve. Surg Oncol 26:28–36
Park EJ, Kim CW, Cho MS, Baik SH, Kim DW, Min BS, Lee KY, Kim NK (2014) Multidimensional analyses of the learning curve of robotic low anterior resection for rectal cancer: 3-phase learning process comparison. Surg Endosc 28:2821–2831
Kagawa H, Kinugasa Y, Shiomi A, Tomohiro Yamaguchi T, Tsukamoto S, Tomioka H, Yamakawa Y, Sato S (2015) Robotic-assisted lateral lymph node dissection for lower rectal cancer: short-term outcomes in 50 consecutive patients. Surg Endosc 29:995–1000
Shiomi A, Kinugasa Y, Yamaguchi T, Tomioka H, Kagawa H (2014) Robot-assisted rectal cancer surgery: short-term outcomes for 113 consecutive patients. Int J Colorectal Dis 29:1105–1111
Zhang Y, Liu S, Han Y, Xiang J, Cerfolio RJ, Li H (2019) Robotic anatomical segmentectomy: an analysis of the learning curve. Ann Thorac Surg 107:1515–1522
Foo CC, Law WL (2016) The learning curve of robotic-assisted low rectal resection of a novice rectal surgeon. World J Surg 40:456–462
Kim HJ, Choi GS, Park JS, Park SY (2014) Multidimensional analysis of the learning curve for robotic total mesorectal excision for rectal cancer: lessons from a single surgeon’s experience. Dis Colon Rectum 9:1066–1074
Kuo LJ, Lin YK, Chang CC, Tai CJ, Chiou JF, Chang YJ (2014) Clinical outcomes of robot-assisted intersphincteric resection for low rectal cancer: comparison with conventional laparoscopy and multifactorial analysis of the learning curve for robotic surgery. Int J Colorectal Dis 29:555–562
Sammon J, Perry A, Beaule L, Kinkead T, Clark D, Hansen M (2010) Robot-assisted radical prostatectomy: learning rate analysis as an objective measure of the acquisition of surgical skill. BJU Int 106:855–860
Davis JW, Kreaden US, Gabbert J, Thomas R (2014) Learning curve assessment of robot-assisted radical prostatectomy compared with open-surgery controls from the premier perspective database. J Endourol 28:560–566
Galfano A, Secco S, Dell’Oglio P, Rha K, Eden C, Fransis K, Sooriakumaran P, De La Muela PS, Kowalczyk K, Miyagawa T, Assenmacher C, Matsubara A, Chiu KY, Boylu U, Lee H, Bocciardi AM (2021) Retzius-sparing robot-assisted radical prostatectomy: early learning curve experience in three continents. BJU Int 127:412–417
Seamon LG, Fowler JM, Richardson DL, Carlson MJ, Valmadre S, Phillips GS, Cohn DE (2009) A detailed analysis of the learning curve: robotic hysterectomy and pelvic-aortic lymphadenectomy for endometrial cancer. Gynecol Oncol 114:162–167
Schreuder HWR, Zweemer RP, Van Baal WM, Van De Lande J, Dijkstra JC, Verheijen RHM (2010) From open radical hysterectomy to robot-assisted laparoscopic radical hysterectomy for early stage cervical cancer: aspects of a single institution learning curve. Gynecol Surg 7:253–258
Hall JB (2013) The learning curve of robotic hysterectomy. Obstet Gynecol 121:1109
Zhou J, Shi Y, Qian F, Tang B, Hao Y, Zhao Y, Yu P (2015) Cumulative summation analysis of learning curve for robot-assisted gastrectomy in gastric cancer. J Surg Oncol 111:760–767
Kim MS, Kim WJ, Hyung WJ, Kim HI, Han SU, Ryu KW, Kim YW, Ryu KW, Park S (2021) Comprehensive learning curve of robotic surgery discovery from a multicenter prospective trial of robotic gastrectomy. Ann Surg 273:949–956
Lu J, Zheng HL, Li P, Xie JW, Wang JB, Lin JX, Chen QY, Cao LL, Lin M, Tu RH, Huang ZN, Huang CM, Zheng CH (2018) A propensity score-matched comparison of robotic versus laparoscopic gastrectomy for gastric cancer: oncological, cost, and surgical stress analysis. J Gastrointest Surg 22:1152–1162
Shakir M, Boone BA, Polanco PM, Zenati MS, Hogg ME, Tsung A, Choudry HA, Moser AJ, Bartlett DL, Zeh HJ, Zureikat AH (2015) The learning curve for robotic distal pancreatectomy : an analysis of outcomes of the first 100 consecutive cases at a high-volume pancreatic centre. HPB 17:580–586
Shyr BU, Chen SC, Shyr YM, Wang SE (2018) Learning curves for robotic pancreatic surgery-from distal pancreatectomy to pancreaticoduodenectomy. Medicine 97:e13000
Chao YK, Wen YW, Chuang WY, Cerfolio RJ (2020) Transition from video-assisted thoracoscopic to robotic esophagectomy: a single surgeon’s experience. Dis Esophagus 33:doz33
Hernandez JM, Dimou F, Weber J, Almhanna K, Hoffe S, Shridhar R, Karl R, Meredith K (2013) Defining the learning curve for robotic-assisted esophagogastrectomy. J Gastrointest Surg 17:1346–1351
Zhang H, Chen L, Wang Z, Zheng Y, Geng Y, Wang F, Liu D, He A, Ma L, Yuan Y, Wang Y (2018) The learning curve for robotic mckeown esophagectomy in patients with esophageal cancer. Ann Thorac Surg 105:1024–1030
Zhu P, Liao W, Ding ZY, Chen L, Zhang WG, Zhang BX, Chen XP (2019) Learning curve in robot-assisted laparoscopic liver resection. J Gastrointest Surg 23:1778–1787
Zhang T, Zhao ZM, Gao YX, Lau WY, Liu R (2019) The learning curve for a surgeon in robot-assisted laparoscopic pancreaticoduodenectomy: a retrospective study in a high-volume pancreatic center. Surg Endosc 33:2927–2933
Yamaguchi T, Kinugasa Y, Shiomi A, Tomioka H, Kagawa H (2016) Robotic-assisted laparoscopic versus open lateral lymph node dissection for advanced lower rectal cancer. Surg Endosc 30:721–728
Kim HJ, Choi GS, Park JS, Park SY, Lee HJ, Woo IT, Park IK (2018) Selective lateral pelvic lymph node dissection: a comparative study of the robotic versus laparoscopic approach. Surg Endosc 32:2466–2473
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Tetsuo Sugishita, Shunsuke Tsukamoto, Jun Imaizumi, Yasuyuki Takamizawa, Manabu Inoue, Konosuke Moritani, Yusuke Kinugasa, and Yukihide Kanemitsu have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sugishita, T., Tsukamoto, S., Imaizumi, J. et al. Evaluation of the learning curve for robot-assisted rectal surgery using the cumulative sum method. Surg Endosc 36, 5947–5955 (2022). https://doi.org/10.1007/s00464-021-08960-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08960-7