Abstract
Purpose
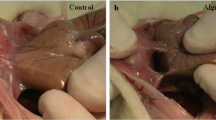
Postoperative intra-abdominal adhesion sometimes causes significant morbidity. The aim of this study was to compare the efficacy of our newly developed antiadhesive material, alginate flakes, to the most commonly used combination of hyaluronic acid and carboxymethyl cellulose film.
Methods
Sodium alginate was formed into a gel, powder, or flakes. In the ex vivo study, these different alginate forms were attached onto pig skin and their antisolubility properties in saline and attachment stability were compared. In the in vivo study, a rat surgical adhesion model was used to study the properties of the alginates, and the rats were euthanized on day 14 after surgery. The efficacy of the antiadhesive materials was evaluated using an adhesion scoring system, and the locations that were treated with the antiadhesives were histologically examined.
Results
In the alginate groups, the alginate flakes were superior with respect to the antisolubility and the attachment stability ex vivo as well as with respect to the antiadhesive efficacy in vivo. The adhesion score was almost the same as that observed in the alginate flake and cellulose film groups.
Conclusions
We developed an alginate flake material and demonstrated its antiadhesive effects both ex vivo and in vivo. This is the first reported study using this flake-like material, which has a unique characteristic in that it can be applied by spraying in compressed air. Alginate flakes may therefore be especially useful in the field of laparoscopic surgery.
Similar content being viewed by others
References
Beck DE, Opelka FG, Bailey HR, Rauh SM, Pashos CL. Incidence of small-bowel obstruction and adhesiolysis after open colorectal and general surgery. Dis Colon Rectum 1999;42:241–248.
Ellis H, Moran BJ, Thompson JN, Parker MC, Wilson MS, Menzies D, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: A retrospective cohort study. Lancet 1999;353:1476–1480.
Hershlag A, Diamond MP, DeCherney AH. Adhesiolysis. Clin Obstet Gynecol 1991;34:395–402.
Avital S, Bollinger TJ, Wilkinson JD, Marchetti F, Hellinger MD, Sands LR. Preventing intra-abdominal adhesions with polylactic acid film: An animal study. Dis Colon Rectum 2005;48:153–157.
Wiseman DM, Gottlick-Iarkowski L, Kamp L. Effect of different barriers of oxidized regenerated cellulose (orc) on cecal and sidewall adhesions in the presence and absence of bleeding. J Invest Surg 1999;12:141–146.
Burns JW, Colt MJ, Burgees LS, Skinner KC. Preclinical evaluation of seprafilm bioresorbable membrane. Eur J Surg Suppl 1997:40–48.
Beck DE, Cohen Z, Fleshman JW, Kaufman HS, van Goor H, Wolff BG. A prospective, randomized, multicenter, controlled study of the safety of seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum 2003;46:1310–1319.
Fazio VW, Cohen Z, Fleshman JW, van Goor H, Bauer JJ, Wolff BG, et al. Reduction in adhesive small-bowel obstruction by seprafilm adhesion barrier after intestinal resection. Dis Colon Rectum 2006;49:1–11.
Reijnen MM, Meis JF, Postma VA, van Goor H. Prevention of intra-abdominal abscesses and adhesions using a hyaluronic acid solution in a rat peritonitis model. Arch Surg 1999;134:997–1001.
Liu Y, Shu XZ, Prestwich GD. Reduced postoperative intraabdominal adhesions using carbylan-sx, a semisynthetic glycosaminoglycan hydrogel. Fertil Steril 2007;87:940–948.
Oncel M, Remzi FH, Senagore AJ, Connor JT, Fazio VW. Comparison of a novel liquid (adcon-p) and a sodium hyaluronate and carboxymethylcellulose membrane (seprafilm) in postsurgical adhesion formation in a murine model. Dis Colon Rectum 2003;46:187–191.
Rowley JA, Mooney DJ. Alginate type and rgd density control myoblast phenotype. J Biomed Mater Res 2002;60:217–223.
Li X, Liu T, Song K, Yao L, Ge D, Bao C, et al. Culture of neural stem cells in calcium alginate beads. Biotechnol Prog 2006;22:1683–1689.
Ponce S, Orive G, Hernandez R, Gascon AR, Pedraz JL, de Haan BJ, et al. Chemistry and the biological response against immunoisolating alginate-polycation capsules of different composition. Biomaterials 2006;27:4831–4839.
Groves AR, Lawrence JC. Alginate dressing as a donor site haemostat. Ann R Coll Surg Engl 1986;68:27–28.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hirasaki, Y., Fukunaga, M., Kidokoro, A. et al. Development of a novel antiadhesive material, alginate flakes, ex vivo and in vivo. Surg Today 41, 970–977 (2011). https://doi.org/10.1007/s00595-010-4410-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-010-4410-1