Abstract
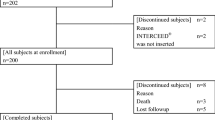
INTRODUCTION: Seprafilm® adhesion barrier (Seprafilm®) has been proven to prevent adhesion formation after abdominal and pelvic surgery. This article reports safety results, including the postoperative incidence of abdominal and pelvic abscess and pulmonary embolism, from a large, multicenter trial designed to evaluate the safety and effectiveness of Seprafilm® for reduction of adhesion-related postoperative bowel obstruction after abdominopelvic surgery. METHODS: A total of 1,791 patients participated in this prospective, randomized, multicenter, multinational, single-blind, controlled study in patients undergoing abdominopelvic surgery, the majority of whom had inflammatory bowel disease. Just before closure of the abdomen, patients were randomized to a Seprafilm® or no-treatment control group. Patients received an average of 4.4 and as many as 10 Seprafilm® adhesion barriers applied to organs and tissue surfaces that sustained direct surgical trauma and to suspected adhesiogenic surfaces. Complications that occurred within the first month after surgery were evaluated. RESULTS: During the safety evaluation period, the difference between the Seprafilm® and control groups for the incidence of abscess (4 vs. 3 percent, respectively) or pulmonary embolism (<1 percent in both groups) was not statistically significant (P > 0.05). Foreign body reaction was not reported in either group. Fistula (2 vs. <1 percent) and peritonitis (2 vs. <1 percent) occurred more frequently (P ≤ 0.05) in the Seprafilm® group. In a subpopulation of patients in whom Seprafilm® was wrapped around a fresh bowel anastomosis, leak-related events, which included anastomotic leak, fistula, peritonitis, abscess, and sepsis, occurred more frequently (P ≤ 0.05). There were no other differences in the incidence, severity, or causative relationship of complications between study groups. CONCLUSIONS: This study confirmed the safety of Seprafilm® adhesion barrier with respect to abdominal abscess, pelvic abscess, and pulmonary embolism when administered to patients undergoing abdominopelvic surgery. Foreign body reaction was not reported for any patient. However, wrapping the suture or staple line of a fresh bowel anastomosis with Seprafilm® should be avoided, because the data suggest that this practice may increase the risk of sequelae associated with anastomotic leak.
Similar content being viewed by others
References
NF Ray WG Denton M Thamer SC Henderson S Perry (1998) ArticleTitleAbdominal adhesiolysis J Am Coll Surg 186 1–9
JM Becker MT Dayton VW Fazio et al. (1996) ArticleTitlePrevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane J Am Coll Surg 183 297–306
MP Diamond . Seprafilm Adhesion Study Group (1996) ArticleTitleReduction of adhesions after uterine myomectomy by Seprafilm® membrane (HAL-F) Fertil Steril 66 904–910
DE Beck FG Opelka HR Bailey SM Rauh CL Pashos (1999) ArticleTitleIncidence of small-bowel obstruction and adhesiolysis after open colorectal and general surgery Dis Colon Rectum 42 241–248
AA Van Der Krabben FR Dijkstra M Nieuwenhuijzen MM Reijnen M Schaapveld H Van Goor (2000) ArticleTitleMorbidity and mortality of inadvertent enterotomy during adhesiotomy Br J Surg 87 467–471
MG Coleman AD McLain BJ Moran (2000) ArticleTitleImpact of previous surgery on time taken for incision and division of adhesions during laparotomy Dis Colon Rectum 43 1297–1299
DE Beck VW Fazio JM Becker et al. (1996) ArticleTitlePerioperative complications after restorative proctocolectomy and ileostomy closure in a prospective multicenter trial Dis Colon Rectum 39 37–1299
VW Fazio Y Ziv J Church et al. (1995) ArticleTitleIleal pouch-anal anastomosis complications and functions in 1005 patients Ann Surg 222 120–127
K Kelly J Pemberton B Wolff R Dozois (1992) ArticleTitleIleal pouch-anal anastomosis Curr Probl Surg 29 64–131
K McMullem TC Hicks JE Ray JB Gathright AE Timmcke (1991) ArticleTitleComplications associated with ileal pouch-anal anastomosis World J Surg 15 763–767
SD Wexner WD Wong DA Rothenberger SM Goldberg (1990) ArticleTitleThe ileoanal reservoir Am J Surg 159 178–185
JW Fleshman Z Cohen RS McLeod H Stern J Blair (1988) ArticleTitleThe ileal reservoir and ileoanal anastomosis procedure Dis Colon Rectum 31 10–16
DJ Schoetz JA Coller MC Veidenheimer (1986) ArticleTitleIleoanal reservoir for ulcerative colitis and familial polyposis Arch Surg 121 404–409
D Blumberg FG Opelka TC Hicks AE Timmcke DE Beck (2001) ArticleTitleRestorative proctocolectomy South Med J 94 467–471
F Merad JM Hay A Fingerhut Y Flamant JM Molkhou Y Laborde (1998) ArticleTitleOmentoplasty in the prevention of anastomotic leakage after colonic or rectal resection Ann Surg 227 179–186
JC Goligher PW Lee KC Simpkins DJ Lintott (1977) ArticleTitleA controlled comparison of one- and two-layer techniques of suture for high and low colorectal anastomosis Br J Surg 64 609–614
S Holzmann RJ Connolly SD Schwaitzberg (1994) ArticleTitleEffect of hyaluronic acid solution on healing of bowel anastomoses J Invest Surg 7 431–437
M Medina HN Paddock RJ Connolly SD Schwaitzberg (1995) ArticleTitleNovel antiadhesion barrier does not prevent anastomotic healing in a rabbit model J Invest Surg 8 179–186
JW Burns MJ Colt LS Burgess KC Skinner (1997) ArticleTitlePreclinical evaluation of Seprafilm™ bioresorbable membrane Eur J Surg 577 40–48
SC Hubbard JW Burns (2002) ArticleTitleEffects of a hyaluronan-based membrane (Seprafilm®) on intraperitoneally disseminated human colon cancer cell growth in a nude mouse model Dis Colon Rectum 45 334–344
I Oikonomakis P Gervaz YS You et al. (2002) ArticleTitleSeprafilm® does not compromise short term oncologic outcome in colorectal cancer Dis Colon Rectum 45 18–19
Author information
Authors and Affiliations
About this article
Cite this article
Beck, D.E., Cohen, Z., Fleshman, J.W. et al. A Prospective, Randomized, Multicenter, Controlled Study of the Safety of Seprafilm® Adhesion Barrier in Abdominopelvic Surgery of the Intestine. Dis Colon Rectum 46, 1310–1319 (2003). https://doi.org/10.1007/s10350-004-6739-2
Issue Date:
DOI: https://doi.org/10.1007/s10350-004-6739-2