Abstract
Aims
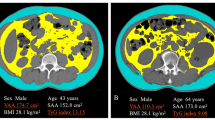
To quantify epicardial adipose tissue (EAT) and visceral adipose tissue (VAT) in Chinese adults with impaired glucose regulation (IGR) or diabetes and compare the contributions of EAT and VAT to the occurrence of IGR and diabetes with those of traditional obesity indices.
Methods
Cardiac and abdominopelvic noncontrast computed tomographic images of 668 individuals were used to measure EAT and VAT volume. Multivariable logistic regression and area under the receiver operating characteristic (ROC) curve were used to illustrate the contributions of these tissues.
Results
Patients with IGR or diabetes had larger EAT and VAT volumes than did the controls, and the VAT volume was significantly different between the IGR and diabetic groups. In multivariable models, higher EAT or VAT volume was positively associated with the presence of IGR and diabetes. After adjusting further for body mass index (BMI) and waist-to-hip ratio (WHR), a higher EAT volume was still positively associated with IGR (odds ratio (OR) = 1.46; 95% confidence interval (CI), 1.04–2.03), and a higher VAT volume was positively associated with IGR (OR = 1.86; 95% CI, 1.15–3.02) and diabetes (OR = 1.86; 95% CI, 1.16–2.99). The areas under the curve (AUCs) of the association of EAT (AUC = 0.751; 95% CI, 0.712–0.789) and VAT (AUC = 0.752; 95% CI, 0.713–0.792) with dysglycemia (IGR + diabetes) were significantly larger than those of the traditional obesity indices (all P < 0.05).
Conclusions
High EAT or VAT volume is positively associated with IGR and diabetes in Chinese adults. With a given WHR and BMI, such an association still exists to some extent. The correlation may be stronger than those of the traditional obesity indices.


Similar content being viewed by others
Abbreviations
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine transaminase
- ANOVA:
-
One-way analysis of variance
- AST:
-
Plasma aspartate transaminase
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- BUN:
-
Blood urea nitrogen
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- CVD:
-
Cardiovascular diseases
- DBP:
-
Diastolic blood pressure
- EAT:
-
Epicardial adipose tissue
- EATHtR:
-
EAT volume-to-height ratio
- ECG:
-
Electrocardiogram
- FDR:
-
False discovery rate
- FFA:
-
Free fatty acid
- FPG:
-
Fasting plasma glucose
- HbA1c:
-
Glycated hemoglobin A1c
- HBP:
-
High blood pressure
- HDL:
-
High-density lipoprotein
- Hs-CRP:
-
High-sensitivity C-reactive protein
- HU:
-
Hounsfield unit
- IFG:
-
Impaired fasting glucose
- IGR:
-
Impaired glucose regulation
- IGT:
-
Impaired glucose tolerance
- IR:
-
Insulin resistance
- LDL:
-
Low-density lipoprotein
- MetS:
-
Metabolic syndrome
- OGTT:
-
75-g oral glucose tolerance test
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristic (curve)
- SAT:
-
Subcutaneous adipose tissue
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- TC:
-
Total cholesterol
- TG:
-
Total triglyceride
- VAT:
-
Visceral adipose tissue
- VATHtR:
-
VAT volume-to-height ratio
- VIF:
-
Variance inflation factor
- WC:
-
Waist circumference
- WHR:
-
Waist-to-hip ratio
- WHtR:
-
Waist-to-height ratio
- γ-GT:
-
Gamma-glutamyl transferase
- 2hPG:
-
2 h plasma glucose
References
Hu C, Jia W (2018) Diabetes in China: epidemiology and genetic risk factors and their clinical utility in personalized medication. Diabetes 67:3–11
Aldworth J, Patterson C, Jacobs E, Misra A, Snouffer EB, Piemonte L et al (2017) International diabetes federation, 8th edn. IDF Diabetes Atlas, Brussels
James C, Bullard KM, Rolka DB, Geiss LS, Williams DE, Cowie CC et al (2011) Implications of alternative definitions of prediabetes for prevalence in U.S. adults. Diabetes Care 34:387–391
Nathan DM, Davidson MB, Defronzo RA, Heine RJ, Henry RR, Pratley R et al (2007) Impaired fasting glucose and impaired glucose tolerance implications for care. Diabetes Care 30:753–759
Xu Y, Wang L, He J, Bi Y, Li M, Wang T et al (2013) Prevalence and control of diabetes in Chinese adults. JAMA 310:948–959
Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M (2012) Prediabetes: a high-risk state for diabetes development. Lancet 379:2279–2290
Neeland IJ, Turer AT, Ayers CR, Powell-Wiley TM, Vega GL, Farzaneh-Far R et al (2012) Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA 308:1150–1159
Smith U (2015) Abdominal obesity: a marker of ectopic fat accumulation. J Clin Investig 125:1790–1792
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horval P, Liu CY et al (2007) Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116:39–48
Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H et al (2003) Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 108:2460–2466
Haslam DW, James WPT (2005) Obesity: the lancet. Lancet 366:1197–1209
American Diabetes Association (2019) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 42(Suppl. 1):S13–S28
World Health Organization (2006) Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia. World Health Organization, Geneva
Yoshizumi T, Nakamura T, Yamane M, Islam AH, Menju M, Yamasaki K et al (1999) Abdominal fat: standardized technique for measurement at CT. Radiology 211:283–286
Tian Y, Jiang C, Wang M, Cai R, Zhang Y, He Z et al (2016) BMI, leisure-time physical activity, and physical fitness in adults in China: results from a series of national surveys, 2000-14. Lancet Diabetes Endocrinol 4:487–497
World Health Organization (1999) Definition, diagnosis and classification of diabetes mellitus and its complication. Part 1: diagnosis and classification of diabetes mellitus. WHO/NCD/NCS, Geneva
Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS et al (2008) Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample the Framingham Heart Study. Circulation 117:605–613
Mahabadi AA, Masaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA et al (2009) Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur Heart J 30:850–856
Iacobellis G (2015) Local and systemic effects of the multifaceted epicardial adipose tissue depot. Nat Rev Endocrinol 11:363–371
Huxley R, Barzi F, Woodward M (2006) Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ Brit Med J 332:73–78
Bays HE (2011) Adiposopathy is “sick fat” a cardiovascular disease? J Am Coll Cardiol 57:2461–2473
Borel AL, Nazare JA, Smith J, Aschner P, Barter P, Van Gaal L et al (2015) Visceral, subcutaneous abdominal adiposity and liver fat content distribution in normal glucose tolerance, impaired fasting glucose and/or impaired glucose tolerance. Int J Obes (Lond) 39:495–501
Smith JD, Borel AL, Nazare JA, Haffner SM, Balkau B, Ross R et al (2012) Visceral adipose tissue indicates the severity of cardiometabolic risk in patients with and without type 2 diabetes: results from the INSPIRE ME IAA study. J Clin Endocrinol Metab 97:1517–1525
Schwenzer NF, Machann J, Schraml C, Springer F, Ludescher B, Stefan N et al (2010) Quantitative analysis of adipose tissue in single transverse slices for estimation of volumes of relevant fat tissue compartments: a study in a large cohort of subjects at risk for type 2 diabetes by MRI with comparison to anthropometric data. Investig Radiol 45:788–794
Acknowledgements
The authors are thankful to JY and XZ from Siemens Healthcare and other members who have participated in this project for their excellent technical support. Permissions were obtained from all contributors to this work. The study received no support in the form of funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the ethics committee of Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China.
Informed consent
All patients signed written informed consent forms before the initiation of the study procedure.
Additional information
Managed by Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Subanalysis of males
Appendix: Subanalysis of males
Rights and permissions
About this article
Cite this article
Wang, S., Wang, Z., Chen, C. et al. Contribution of epicardial and abdominopelvic visceral adipose tissues in Chinese adults with impaired glucose regulation and diabetes. Acta Diabetol 56, 1061–1071 (2019). https://doi.org/10.1007/s00592-019-01348-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01348-z