Abstract
Reconstructive surgery of the clavicle using free vascularised fibula grafting (FVFG) is sometimes required for the management of severe bone loss or non-union. As the procedure is relatively rare, there is no universal agreement on the management and outcome. This systematic review aimed to first, identify the conditions for which FVFG has been applied; second, to gain an understanding of the surgical techniques used; and third, to report outcomes related to bone union, infection eradication, function and complications. A PRISMA strategy was used. Medline, Cochrane Central Register of Controlled Trials, Scopus and EMBASE library databases were interrogated using pre-defined MeSH terms and Boolean operators. Quality of evidence was evaluated based on OCEBM and GRADE systems. Fourteen studies based on 37 patients were identified with a mean follow-up time of 33.3 months. The most common reasons for the procedure were: fracture non-union; tumours requiring resection; post-radiation treatment osteonecrosis and osteomyelitis. The operation approaches were similar, involving graft retrieval, insertion and fixation and vessels chosen for reattachment. The mean clavicular bone defect size was 6.6 cm (± 1.5), prior to FVFG. Bone union occurred in 94.6% with good functional outcomes. Complete infection eradication occurred in those with preceding osteomyelitis. The main complications were broken metalwork, delayed union/non-union and fibular leg paraesthesia (n = 20). The mean re-operation number was 1.6 (range 0–5.0). The study demonstrates that FVFG is well tolerated and has a high success rate. However, patients should be advised about complication development and re-intervention requirement. Interestingly, overall data is sparse with no large cohort groups or randomised trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The clavicle is a double curved s-shaped long bone articulating with the sternum medially and acromion laterally, and is stabilised by strong ligaments at either end [1]. Maintaining the integrity of the clavicle is important for normal shoulder function, the avoidance of compression of underlying structures (e.g., brachial plexus and axillary artery) and for optimum respiratory function [2].
Injury and dysfunction of the clavicle most commonly follows a fracture occurring as a consequence of direct trauma to the shoulder [3, 4]. Clavicle fractures are fairly common and account for approximately 2.6–4% of all fractures [5, 6]. In many of these cases, management is non-surgical, but when surgery is required, an open reduction and internal fixation (ORIF) with a plate is most frequently used in the first stages to stabilise the bone and encourage healing [7, 8]. In the UK, surgical intervention for clavicular fractures ranges from 2 to 4% of all fractures [9].
If unsuccessful, the plate is removed and another inserted with an iliac crest autologous bone graft, for enhancement of the fracture healing response. On failing this, reconstructive surgery is then considered. A similar scenario may follow other clavicular disorders, such as tumour infiltration, osteomyelitis or bone necrosis secondary to radiotherapy [10,11,12], although in these latter cases, reconstructive surgery may be required as an earlier option.
Taylor et al., described a reconstructive approach known as the free vascularised fibula graft (FVFG) to manage significant long bone defects [13]. The principles of this technique relate to the abundant vascularity of the fibula, its similarity in bony shape to the clavicle, and its functional adaptation to the recipient site [14]. However, as the procedure is relatively uncommon [15], there is a paucity of literature specifically describing the outcomes.
The objectives of this review were to: first, identify the conditions for which FVFG has been applied; second, to gain an understanding of the types and choice of surgical techniques used; and third, to report outcomes related to bone union, infection eradication, functional and complications.
Methods
Search strategy and criteria
The protocol for this systematic review was based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [16], and was created prior to data extraction. A list of Medical Subject Headings (MeSH) terms and Boolean operators were compiled: (clavicle OR clavicular) AND (non-union OR pseudarthrosis) AND (management OR free vascularised fibular graft). These words were utilised to search Medline (through the PubMed search engine), Cochrane Central Register of Controlled Trials (CENTRAL), Scopus and EMBASE databases. The search strategies implemented are detailed in Appendix 1.
Study selection
Inclusion criteria were established using the population intervention comparison outcomes (PICO) approach [17]: Population: adults (over 18) with clavicular non-union and concomitant osseous defects. There were no limits on sex, ethnicity or co-morbidities of the individuals included. Intervention: FVFG. Comparator: management strategies used to treat clavicular non-union e.g., ORIF or bone grafting, excluding FVFG. Outcomes: the primary outcome measured was bone healing. Secondary outcomes included infection eradication; functional outcomes; and complications including unplanned re-operations. Exclusion criteria included: reviews, editorials and viewpoints, subjects aged 16 years or less, congenital cases of clavicular non-union and cases in which a complete neo-clavicle was required.
All studies were considered for eligibility, with no restrictions on publication date or language applied. Titles and abstracts were screened for relevance prior to full inspection. The reference lists of all eligible studies were reviewed to isolate any articles that may have been missed in the initial database search. Duplicate articles between the databases were removed and the full texts of all studies meeting the inclusion criteria were obtained. To increase the reliability of data extraction, two reviewers blindly performed the study selection and data extraction. Any disagreements between reviewers were resolved with discussion with the senior author.
Data collection
Data was extracted and collated using a purpose-designed Microsoft Excel spreadsheet. The following data were recorded: (1) study characteristics (study design, sample size); (2) patient demographics and baseline characteristics (age, sex, co-morbidities); (3) initial clavicular injury prior to FVFG intervention (cause of bone defect, presence of infection, number of surgical procedures, type of procedures, size of bone defect); (4) surgical procedure utilised to harvest and transfer FVFG (operation techniques for graft insertion and vascular anastomosis); (5) outcome measures (bone union, infection eradication, functional outcomes, complications).
Assessment of methodological quality
Methodological quality of the included studies was assessed and graded using the OCEBM ‘Levels of Evidence’ guidelines [18].
The overall quality of evidence in this systematic review was evaluated using the grading of recommendations, assessment, development and evaluation (GRADE) system [19]. Recommendations were classified as either high, moderate, low, or very low according to the authors’ interpretation of the true effect in the study compared to the estimated effect. This approach involved grading the evidence included based on the criteria for risk of bias, imprecision, inconsistency, indirectness and publication bias.
Statistical analysis
Descriptive statistical analysis (e.g., mean ± standard deviation (SD), mean ranges, ratios and percentages) was collated and reported in this study.
Results
Search results
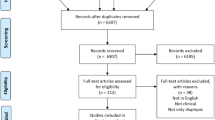
The PRISMA flowchart is shown in Fig. 1.
102 Medline articles, 11 CENTRAL articles, 154 Scopus articles and 121 EMBASE articles were obtained. In addition, a further search of records yielded an additional 4 studies; this provided a baseline of 392 studies in total. Upon removal of duplicates between the databases, the overall articles screened were 307. These were then narrowed to 67 upon title and abstract screening for relevance, with 52 articles assessed for eligibility into this study. The full texts of all 14 studies meeting the inclusion criteria were obtained [20,21,22,23,24,25,26,27,28,29,30,31,32,33].
Table 1 provides an overview of the studies included in the systematic review. Of the 14 studies included in the analysis, 5 were case series [21,22,23, 25, 30], 4 were case reports [26,27,28, 33], 4 were cases within research articles [20, 29, 31, 33], and 1 was a technical note [24]. Overall, 37 individuals treated with FVFG were included in our study. The mean participant age in the studies was 44.8 (± 12.8) years old (mean range 17–68), and the mean follow-up time was 33.3 (± 28.4) months (mean range 3 months–10 years) post-operatively.
Methodological quality
OCEBM ‘Levels of Evidence’ (Appendix 2) demonstrated the overall level of evidence of all 14 studies [20,21,22,23,24,25,26,27,28,29,30,31,32,33], included as “Level IV”. This is due to all research being case series [21,22,23, 25, 30], case reports [26,27,28, 33], case reports within research articles [20, 29, 31, 33], and a technical note [24].
In addition, Appendix 2 provides an overview of the GRADE analysis assessment, which demonstrated the quality of evidence to be Low for all analyses, as there were no large observational studies or randomised controlled trials on this subject.
Patient demographics and baseline characteristics
Of the 37 individuals reported in this review with a mean patient age of 44.8 (± 12.8) years old, 19 were men and 16 women; the sex of 2 cases was unreported (1.2:1 male to female ratio) (Table 1).
With regards to co-morbidities, there were 8 tobacco smokers [22, 24,25,26, 30, 31], 1 patient with excess alcohol consumption [22], 1 hypertensive patient [22], 1 individual living with depression [22] and another with hepatitis [22].
Initial clavicular injury and surgical procedures prior to FVFG intervention
The causes of clavicular bone defect have been classified into four main categories: fracture non-union, tumours, osteoradionecrosis following radiation therapy for tumour treatment and osteomyelitis.
In this review, there were 27 persistent non-unions secondary to fracture (e.g., from fall onto ipsilateral shoulder, road traffic accident, gunshot wound) [20,21,22,23,24,25, 28,29,30,31]; 3 tumours requiring resection (1 lung apex carcinoma, 1 recurrent dermatofibrosarcoma, 1 plasmacytoma) [25, 26, 32]; 2 cases of osteoradionecrosis (following radiotherapy of: 1 nasopharyngeal carcinoma, 1 breast cancer) [31, 33]; and six cases of clavicular osteomyelitis (1 tuberculosis, 1 Methicillin-resistant Staphylococcus aureus (MRSA), 1 Staphylococcus aureus, 1 Pseudomonas species, 2 further unidentified species) [22, 24, 25, 27, 29, 30], (Table 1).
Prior to surgical management using FVFG, the mean number of previous operations was 2.5 (± 1.8), with a mean range of 0.5–6 procedures, based on the information provided (Table 1). Management strategies of these cases prior to the fixation of the bone defect with fibular grafting varied, and included both conservative and surgical fixation. First-line conservative management of these clavicular injuries were reported in 8/37 cases [21, 22, 24, 26], through the use of a figure-of-8 splint. In contrast, ORIF was the most common surgical procedure, accounting for 70.3% (26/37) of all operative techniques attempted before FVFG [20,21,22,23,24,25,26, 28,29,30,31,32,33]. ORIF was performed using: a compression plate alone (n = 12) [22, 24, 25, 30], plate with iliac crest graft (ICG) (n = 9) [21, 22, 24, 25], plate with synthetic graft (n = 1) [22], plate with tibial cancellous graft (1) [22], or plate with ICG and the addition of a pectoralis muscle flap (n = 1) [22]. In addition, ORIF was also achieved with a wire, plate and graft (n = 1) [23] or a wire and plate alone (n = 1) [23], screw fixation (n = 2) [21, 29] and the implementation of bone morphogenetic protein-7 (BMP-7) (n = 1) [24]. Further techniques that were implemented were resection/tumour excision (n = 6) [21, 25, 26, 32, 33], debridement (n = 1) [27], intramedullary (IM) pin insertion with segmental allograft (n = 1) [21], and further grafting (n = 1) [21]. In five cases, precise detail describing the technique of primary fixation performed was not provided [27, 28, 31] (Table 1).
The mean clavicular bone defect size was 6.6 cm (± 1.5), prior to vascularised fibular grafting. The mean size of these defects in the sample ranged from 4.5 cm to 9.5 cm (Table 1).
Surgical procedure for FVFG harvesting and transfer
The reported surgical procedures followed similar principles but with some variations, (Table 2). All but one case reported the grafts being stabilised using internal fixation with plate and screws [20,21,22,23,24,25,26,27,28, 30,31,32,33]. The arterial and venous anastomoses are documented in Table 2.
Outcome measures
The primary outcome measure of successful bone union occurred in 35/37 (94.6%) individuals [20,21,22,23,24,25,26,27, 29,30,31,32,33]. When infection was a cause of non-union, the results demonstrated eradication in 100% of cases (6/6) [22, 24, 25, 27, 29, 30]. Table 3 demonstrates the range of scoring systems used to measure functional outcomes. The results of these functional scoring assessments are found in Table 2.
Complications and follow-up
There were a variety of post-operative complications noted in the reports included in this study (Table 2). 10 patients experienced pain (8 fibula, 2 clavicle) [21, 25, 28, 32], 8 paraesthesia (7 fibula, 1 ulnar nerve distribution) [21, 30] and 7 patients displayed weakness, in particular the long toe flexors and extensors [30]. Furthermore, 2 patients demonstrated persistent clavicular non-union [20, 28], 2 had delayed union (but eventually united) [24, 25] and 1 re-fracture was observed [21]. Additional complications included: 2 skin infections managed with antibiotics, 1 fistula formation, 1 scar dehiscence and 1 venous kinking [23, 25, 31]. The mean number of re-operations was 1.6 (± 2.0), with a range of 0–5.0 additional procedures. These further operations were due to broken metalwork, pain, infection, bleeding and cosmesis, and involved: plate removals (n = 7) [21, 28, 30, 32], screw removals (n = 3) [21, 25, 32], further cancellous grafting (n = 4) [24, 30], bleeding revisions (n = 3) [23] and the removal of an infected flap and debridement (n = 1) [25] (Table 2). The mean follow-up time was 33.3 months (± 28.4) (range 3 months–10 years).
Discussion
The treatment of large bone defects remains a challenge for reconstructive surgeons. Usually, this group of patients has been through a prolonged clinical journey having undergone several operations that have failed to address the original problem, usually being fracture non-union and/or chronic osteomyelitis. The need to resect the avascular, dead bone leads to bone loss and the development of bone defects.
Evidence was sought for the use of a vascularised fibular bone graft for the management of significant clavicular bone defects requiring reconstructive surgery. We examined the aetiology, patient characteristics, the variations in surgical technique and outcomes.
Overall, there was a slightly higher predisposition towards males requiring this surgery. The mean age was 44.8 years which may reflect a higher rate of falls, an increasing risk of bone pathologies or less preponderance to healing when compared to a younger age group [4]. Direct trauma accounted for approximately 80% (30/37) of the cases as the primary mechanism of injury. In these cases, fibular graft surgery often followed several preceding operative interventions (mean previous operations 2.5), such as an ORIF with plating, bone grafting (often from the iliac crest) and debridement. The remaining cases mostly related to infiltrative and/or destructive disease processes, such as that caused by tumour, radiotherapy or infection; in these situations, the procedure was more likely to be done as an earlier intervention [34, 35].
The mean cortical defect size across studies was 6.6 cm (range 4.5–9.5 cm); their relatively large size reflecting the need for a more aggressive approach. In some cases, the large size of the defect reflected the consequences of multiple previous operative resections and debridements of the bone ends from previous attempts at surgery or because the lesion was primarily large e.g. due to neoplasm.
Although the general principles of harvesting and implanting a graft was similar between studies, there were variations in the operation technique. The choice of a specific technique might be dependent on the degree of bone loss, underlying reasons for the bone loss as well as the personal preferences of the surgeon.
The reported overall outcome of a fibular graft was 94.6% (35/37) for a successful union. Eleven different functional outcome measures were employed across the studies highlighting a lack of standardisation. The reported complications related to either the clavicle itself (21 patients) or the fibular donor site (15 patients). With respect to the clavicle, most complications related to the metalwork and vascular tree. In contrast, paraesthesia and weakness were the main consequences of the fibular procedure [30]. The mean number of re-operations was 1.6, with a range of 0 to 5.0 additional procedures. It is therefore pertinent for surgeons to warn patients of an increased risk of re-interventions and chronic pain/ paraesthesia to the donor or recipient site.
The main limitation of the study is the relatively small sample size which has prevented formal statistical analysis. It is also unknown how common this procedure is performed within practice and whether only cases with a positive surgical outcome are published. It was also noted that there were differences in what data was reported within studies resulting in variability in some demographic and outcome data. The two cases that failed to unite did not provide data on co-morbidities or previous surgical procedures [20, 28].
The strengths of the paper relate to it being a systematic review which followed a structured strategy for data collection and analysis. Integrity of the data was optimised by discussions of the articles between authors. During preparation of this manuscript, another systematic review on the same topic was published [33]. This was based on data up to January 2020 from only 3 search engines (including Google scholar) and included contrary to our strategy, data on paediatric and congenital cases [33]. Despite this, we feel that our study provides further information to the subject area for reconstruction of clavicular defects in adult patients with similar aetiopathogeneses related to fracture non-union and chronic osteomyelitis.
In summary, this study has highlighted that the use of a FVFG, when applied in specific situations, often has successful clinical, functional and radiological outcomes. However, the lack of standardisation of procedures and outcome measurement, and the available small number of patients reported makes it challenging to provide a comprehensive evaluation of the technique. Further studies with larger patient sample sizes are desirable to provide more robust evidence and facilitate a meta-analysis in this field.
References
Matsumura N, Nakamichi N, Ikegami H, Nagura T, Imanishi N, Aiso S, Toyama Y (2013) The function of the clavicle on scapular motion: a cadaveric study. J Shoulder Elb Surg 22:333–339. https://doi.org/10.1016/j.jse.2012.02.006
Robinson CM (1998) Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 80:476–484. https://doi.org/10.1302/0301-620x.80b3.8079
Nordqvist A, Petersson C, Redlund-Johnell I (1993) The natural course of lateral clavicle fracture. 15 (11–21) year follow-up of 110 cases. Acta Orthop Scand 64:87–91. https://doi.org/10.3109/17453679308994539
Singh R, Rambani R, Kanakaris N, Giannoudis PV (2012) A 2-year experience, management and outcome of 200 clavicle fractures. Injury 43:159–163. https://doi.org/10.1016/j.injury.2011.04.008
Nordqvist A, Petersson C (1994) The incidence of fractures of the clavicle. Clin Orthop Relat Res 300:127–132
Postacchini F, Gumina S, De Santis P, Albo F (2002) Epidemiology of clavicle fractures. J Shoulder Elb Surg 11:452–456. https://doi.org/10.1067/mse.2002.126613
Kabak S, Halici M, Tuncel M, Avsarogullari L, Karaoglu S (2004) Treatment of midclavicular nonunion: comparison of dynamic compression plating and low-contact dynamic compression plating techniques. J Shoulder Elb Surg 13:396–403. https://doi.org/10.1016/j.jse.2004.01.033
Wolf S, Chitnis AS, Manoranjith A, Vanderkarr M, Plaza JQ, Gador LV, Holy E, Sparks C, Lambert SM (2022) Surgical treatment, complications, reoperations, and healthcare costs among patients with clavicle fracture in England. BMC Musculoskelet Disord 23:135. https://doi.org/10.1186/s12891-022-05075-5
Daniilidis K, Raschke MJ, Vogt B, Herbort M, Schliemann B, Günther N, Koesters C, Fuchs T (2013) Comparison between conservative and surgical treatment of midshaft clavicle fractures: outcome of 151 cases. Technol Health Case 21:143–147. https://doi.org/10.3233/THC-130714
Niikura T, Lee SY, Sakai Y, Nishida K, Kuroda R, Kurosaka M (2012) Radiation-associated fracture nonunion of the clavicle treated with locking plate fixation and autologous bone grafting. Case Rep Med. https://doi.org/10.1155/2012/407349
Rollo G, Pichierri P, Marsilio A, Filipponi M, Bisaccia M, Meccariello L (2017) The challenge of nonunion after osteosynthesis of the clavicle: Is it a biomechanical or infection problem? Clin Cases Miner Bone Metab 14:372–378. https://doi.org/10.11138/ccmbm/2017.14.3.372
Priemel MH, Stiel N, Zustin J, Luebke AM, Schlickewei C, Spiro AS (2019) Bone tumours of the clavicle: Histopathological, anatomical and epidemiological analysis of 113 cases. J Bone Oncol 16:100229. https://doi.org/10.1016/j.jbo.2019.100229
Taylor GI, Miller GD, Ham FJ (1975) The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg 55:533–544. https://doi.org/10.1097/00006534-197505000-00002
Bumbasirevic M, Stevanovic M, Bumbasirevic V, Lesic A, Atkinson HD (2014) Free vascularised fibular grafts in orthopaedics. Int Orthop 38:1277–1282. https://doi.org/10.1007/s00264-014-2281-6
Lazarus MD (2002) Fractures of the clavicle. In: Bucholz RW, Heckman JD (eds) Rockwood and greens fractures in adults, 5th edn. Lippincott-Wilkins, Philadelphia, pp 1041–1078
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical Research ed.) 339:2535. https://doi.org/10.1136/bmj.b2535
Higgins JPT, Thomas J, ChandlerJ CM, Li T, Page MJ, Welch VA (eds) (2019) Cochrane handbook for systematic reviews of interventions, 2nd edn. Wiley, Chichester
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H (2011) The 2011 Oxford CEBM levels of evidence (introductory document). https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. Accessed 30 Mar 2023
Siemieniuk R and Guyatt G (n.d.) What is GRADE? BMJ Best Practice. https://bestpractice.bmj.com/info/us/toolkit/learn-ebm/what-is-grade/. Accessed 30 Mar 2023
Wood MB (1987) Upper extremity reconstruction by vascularized bone transfers: results and complications. J Hand Surg Am 12:422–427. https://doi.org/10.1016/s0363-5023(87)80017-5
Momberger NG, Smith J, Coleman DA (2000) Vascularized fibular grafts for salvage reconstruction of clavicle nonunion. J Shoulder Elb Surg 9:389–394. https://doi.org/10.1067/mse.2000.107090
Erdmann D, Pu CM, Levin LS (2004) Nonunion of the clavicle: a rare indication for vascularized free fibula transfer. Plast Reconstr Surg 114:1859–1863. https://doi.org/10.1097/01.prs.0000142740.25283.c8
Krishnan KG, Mucha D, Gupta R, Schackert G (2008) Brachial plexus compression caused by recurrent clavicular nonunion and space-occupying pseudoarthrosis: definitive reconstruction using free vascularized bone flap-a series of eight cases. Neurosurgery 62:ONS461–ONS470. https://doi.org/10.1227/01.neu.0000326036.54714.17
Lenoir H, Williams T, Kerfant N, Robert M, Le Nen D (2013) Free vascularized fibular graft as a salvage procedure for large clavicular defect: a two cases report. Orthop Traumatol Surg Res 99:859–863. https://doi.org/10.1016/j.otsr.2013.06.004
Abarca J, Valle P, Valenti P (2013) Clavicular reconstruction with free fibula flap: a report of four cases and review of the literature. Injury 44:283–287. https://doi.org/10.1016/j.injury.2013.01.026
Ye L, Taylor GI (2017) A 10-year follow-up of a free vascularized fibula flap clavicle reconstruction in an adult. Plast Reconstr Surg Glob 5:e1317. https://doi.org/10.1097/GOX.0000000000001317
Choke A, Ou Yang Y, Koh JSB, Howe TS, Tan BK (2018) Restoring a functional and mobile shoulder following reconstruction of the sternoclavicular joint with a free vascularized fibular flap. JPRAS Open 16:73–77. https://doi.org/10.1016/j.jpra.2018.01.004
Arenas-Miquelez A, Karargyris O, Olariu R, Zumstein M (2019) Free Vascularized fibular graft for reconstruction of the lateral clavicle: a case report and review of the literature. JBJS Case Connect 9:e0330. https://doi.org/10.2106/JBJS.CC.18.00330
Goormans F, Vranckx J, Herteleer M, Onsea J, Noppe N, Depypere M, Nijs S, Metsemakers WJ (2019) Segmental bone loss of the clavicle due to fracture-related infection: a multidisciplinary challenge. J Bone Jt Infect 4:60–64. https://doi.org/10.7150/jbji.32580
Petje G, Kinsky RM, Girsh W (2020) A free vascularized fibular graft, open reduction and internal fixation for the treatment of non-union after middle-third clavicle fractures: a case series. SF J Orthop 1:1003
Lim KA, Lin CH, Lin CH (2021) A 19-year experience with clavicular defects: an algorithm for flap selection and surgical outcomes. Ann Plast Surg 86:562–567. https://doi.org/10.1097/SAP.0000000000002547
Claxton MR, Houdek MT, Tibbo ME, Wagner ER, Bakri K, Moran SL (2020) Utility of free vascularized fibular flaps to treat radiation-associated nonunions in the upper extremity. J Plast Reconstr Aesthet Surg 73:633–637. https://doi.org/10.1016/j.bjps.2019.11.015
Wu YHA, Riverol O, Lee KXA, Chang KH, Harnke B, Liao LY, Chen HC (2023) Free vascularized fibular flap for clavicle reconstruction: a systematic review with a new case. J Plast Reconstr Aesthet Surg 76:271–282. https://doi.org/10.1016/j.bjps.2022.08.078
Weiland AJ, Kleinert HE, Kutz JE, Daniel RK (1979) Free vascularized bone grafts in surgery of the upper extremity. J Hand Surg Am 4:129–144. https://doi.org/10.1016/s0363-5023(79)80129-x
Jupiter JB, Fernandez DL, Levin LS, Wysocki RW (2010) Reconstruction of posttraumatic disorders of the forearm. Instr Course Lect 59:283–293
Author information
Authors and Affiliations
Contributions
Conceptualisation and design: PVG; methodology: SMW, VPG; formal data collection, analysis and investigation: SMW; writing—original draft preparation: SMW; writing—review and editing: SMW, VPG, PVG; supervision: PVG]. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflict of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Tables showing the Medline, CENTRAL, Scopus and EMBASE database search protocols used
Search | Number of results |
|---|---|
Medline | |
(1) “clavicle” OR “clavicular” | 12,461 |
(2) “non-union” OR “pseudarthrosis” | 13,035 |
(3) “management” OR “free vascularised fibular graft” | 3,656,271 |
(4) 1, 2 AND 3 | 102 |
CENTRAL | |
(1) “clavicle” OR “clavicular” | 849 |
(2) “non-union” OR “pseudarthrosis” | 617 |
(3) “management” OR “free vascularised fibular graft” | 163,683 |
(4) 1, 2 AND 3 | 11 |
Scopus | |
(1) “clavicle” OR “clavicular” | 28,044 |
(2) “non-union” OR “pseudarthrosis” | 40,675 |
(3) “management” OR “free vascularised fibular graft” | 6767 |
(4) 1, 2 AND 3 | 154 |
EMBASE | |
(1) “clavicle” OR “clavicular” | 16,224 |
(2) “non-union” OR “pseudarthrosis” | 19,650 |
(3) “management” OR “free vascularised fibular graft” | 2,961,975 |
(4) 1, 2 AND 3 | 121 |
Appendix 2: OCEBM and GRADE methodological systems
All primary research articles obtained for this systematic review were case series, case reports, case reports within research studies or a technical note. There are no current large cohort studies or randomised controlled trials (RCTs) describing the surgical technique of free vascularised fibular grafting for clavicular bone defects.
Author | Design of study | OCEBM level of evidence [18] | GRADE assessment [19] |
|---|---|---|---|
Wood [20] | Cases within research article | Level IV | Low |
Momberger et al. [21] | Case series | Level IV | Low |
Erdmann et al. [22] | Case series | Level IV | Low |
Krishnan et al. [23] | Case series | Level IV | Low |
Lenoir et al. [24] | Technical note | Level IV | Low |
Abarca et al. [25] | Case series | Level IV | Low |
Ye et al. [26] | Case report | Level IV | Low |
Choke et al. [27] | Case report | Level IV | Low |
Arenas-Miquelez et al. [28] | Case report | Level IV | Low |
Goormans et al. [29] | Case within research article | Level IV | Low |
Petje et al. [30] | Case series | Level IV | Low |
Lim et al. [31] | Cases within research article | Level IV | Low |
Claxton et al. [32] | Case within research article | Level IV | Low |
Wu et al. [33] | Case report | Level IV | Low |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wakefield, S.M., Giannoudis, V.P. & Giannoudis, P.V. Clavicular bone defects managed with free vascularised fibular grafting: evidence to date. Eur J Orthop Surg Traumatol 33, 3307–3318 (2023). https://doi.org/10.1007/s00590-023-03598-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03598-8