Abstract
Purpose
To evaluate the usefulness of a novel MRI sequence strategy in the assessment of the periprosthetic anatomical structures after primary total knee arthroplasty.
Methods
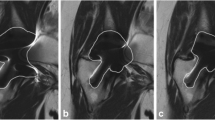
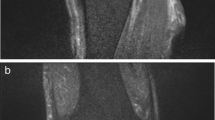
Two MR sequences were retrospectively compared for the imaging of 15 patients with implanted cruciate-retaining/fixed-bearing TKAs (DePuy, PFC Sigma): a slice encoding sequence for metal artifact correction (SEMAC) and a standard sequence. Images were acquired on a 1.5-T system. The degree of artifact reduction was assessed using several qualitative (Likert-type scale) (artifact size, distorsion, blur, image quality, periprosthetic bone, posterior cruciate ligament, lateral collateral ligament, medial collateral ligament, patella tendon, popliteal vessels) and quantitative (artifact volume, Insall–Salvati index, length of patella/tendon, prosthesis dimensions) parameters by blinded reads performed by four investigators. The SEMAC sequences were statistically compared with the standard sequence using Wilcoxon test. Additionally, the intraclass correlation coefficient (ICC) for interobserver agreement was calculated.
Results
Higher levels of blurring were found with SEMAC compared to standard sequences (p < 0.001). All other qualitative parameters improved significantly with the application of SEMAC. In comparison with conventional sequences, the artifact volume was reduced by 59% utilizing SEMAC. Thus, the artifact reduction improved the precision of measurements such as Insall–Salvati index and length of patella/tendon (p < 0.001). The dimension of the tibial component (Ti alloy/polyethylene) revealed accurate values with both MRI sequences. A sufficient interobserver agreement among all readers was found with SEMAC, qualitatively ICC 0.9 (range 0.8–1) as well as quantitatively ICC 0.95 (range 0.92–0.98).
Conclusions
SEMAC effectively reduces artifacts caused by metallic implants after total knee arthroplasty relative to standard imaging. This allows for an improved assessment of periprosthetic anatomical structures. This might enable an improved detectability of postoperative complications in the future.
Level of evidence
Diagnostic Study Level III.





Similar content being viewed by others
References
Agten CA, Del Grande F, Fucentese SF, Blatter S, Pfirrmann CW, Sutter R (2015) Unicompartmental knee arthroplasty MRI: impact of slice-encoding for metal artefact correction MRI on image quality, findings and therapy decision. Eur Radiol 25:2184–2193
Bachschmidt TJ, Sutter R, Jakob PM, Pfirrmann CW, Nittka M (2015) Knee implant imaging at 3 Tesla using high-bandwidth radiofrequency pulses. J Magn Reson Imaging 41:1570–1580
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Fritz J, Ahlawat S, Demehri S, Thawait GK, Raithel E, Gilson WD, Nittka M (2016) Compressed sensing SEMAC: 8-fold accelerated high resolution metal artifact reduction MRI of cobalt-chromium knee arthroplasty implants. Invest Radiol 51:666–676
Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR (2014) A new method for defining balance: promising short-term clinical outcomes of sensor-guided TKA. J Arthroplasty 29:955–960
Jawhar A, Sohoni S, Shah V, Scharf HP (2014) Alteration of the patellar height following total knee arthroplasty. Arch Orthop Trauma Surg 134:91–97
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89:780–785
Lee MJ, Janzen DL, Munk PL, MacKay A, Xiang QS, McGowen A (2001) Quantitative assessment of an MR technique for reducing metal artifact: application to spin-echo imaging in a phantom. Skeletal Radiol 30:398–401
Lu W, Pauly KB, Gold GE, Pauly JM, Hargreaves BA (2009) SEMAC: slice encoding for metal artifact correction in MRI. Magn Reson Med 62:66–76
Math KR, Zaidi SF, Petchprapa C, Harwin SF (2006) Imaging of total knee arthroplasty. Semin Musculoskelet Radiol 10:47–63
Meneghini RM, Ritter MA, Pierson JL, Meding JB, Berend ME, Faris PM (2006) The effect of the Insall–Salvati ratio on outcome after total knee arthroplasty. J Arthroplasty 21:116–120
Mont MA, Serna FK, Krackow KA, Hungerford DS (1996) Exploration of radiographically normal total knee replacements for unexplained pain. Clin Orthop Relat Res 331:216–220
Montgomery RL, Goodman SB, Csongradi J (1993) Late rupture of the posterior cruciate ligament after total knee replacement. Iowa Orthop J 13:167–170
Reichert M, Ai T, Morelli JN, Nittka M, Attenberger U, Runge VM (2015) Metal artefact reduction in MRI at both 1.5 and 3.0 T using slice encoding for metal artefact correction and view angle tilting. Br J Radiol 88:20140601
Schnurr C, Eysel P, Konig DP (2012) Is the effect of a posterior cruciate ligament resection in total knee arthroplasty predictable? Int Orthop 36:83–88
Schulze A, Scharf HP (2013) Satisfaction after total knee arthroplasty. Comparison of 1990–1999 with 2000–2012. Orthopade 42:858–865
Seon JK, Song EK, Park SJ, Lee DS (2011) The use of navigation to obtain rectangular flexion and extension gaps during primary total knee arthroplasty and midterm clinical results. J Arthroplasty 26:582–590
Sofka CM, Potter HG, Figgie M, Laskin R (2003) Magnetic resonance imaging of total knee arthroplasty. Clin Orthop Relat Res 406:129–135
Sutter R, Hodek R, Fucentese SF, Nittka M, Pfirrmann CW (2013) Total knee arthroplasty MRI featuring slice-encoding for metal artifact correction: reduction of artifacts for STIR and proton density-weighted sequences. AJR Am J Roentgenol 201:1315–1324
Takahashi T, Wada Y, Yamamoto H (1997) Soft-tissue balancing with pressure distribution during total knee arthroplasty. J Bone Joint Surg Br 79:235–239
Weale AE, Murray DW, Newman JH, Ackroyd CE (1999) The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br 81:790–795
Zotti MG, Campbell DG, Woodman R (2012) Detection of periprosthetic osteolysis around total knee arthroplasties an in vitro study. J Arthroplasty 27:317–322
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mathias Nittka is an employee of Siemens Healthcare GmbH. The remaining authors declare that there were no conflicts of interest.
Rights and permissions
About this article
Cite this article
Jawhar, A., Reichert, M., Kostrzewa, M. et al. Usefulness of slice encoding for metal artifact correction (SEMAC) technique for reducing metal artifacts after total knee arthroplasty. Eur J Orthop Surg Traumatol 29, 659–666 (2019). https://doi.org/10.1007/s00590-018-2322-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2322-8