Abstract
Introduction
Most of the techniques described in the literature for the repair of chronic partial ACL tears do not spare the intact portion of the ligament. Aim of this study was to perform a retrospective analysis of the results obtained from the same ACL reconstructive surgical technique applicated by sparing or not AM bundle in a population of 42 sports patients.
Materials and methods
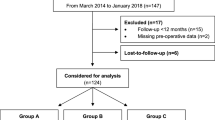
From 2010 to 2012, 42 patients who suffered ACL partial tear injury with rupture of posterolateral bundle were randomly divided in two groups homogenous for sex, age and sport-level activities. The first group with 22 patients performed ACL reconstruction with ST-GR over-the-top technique sacrificing the anteromedial (Removing AMT Group) remaining bundle intact; otherwise, the second group with 20 patients performed the same ACL reconstruction using only ST and maintaining AM bundle (Sparing AMT Group). All the patients were followed up by MRI evaluation at 12 months and clinical evaluation with IKDC score, Tegner score at 6, 12, 24, 36, 48 and 60 months. KT-1000 instrument was performed at 12 months. The results were analyzed statistically to evaluate differences between the two groups in terms of subjective outcome, and stability and for all the tests P < 0.05 was considered significant.
Results
We did not observe any failure at final follow-up. IKDC subjective score at final follow-up in Removing AMT Group was 91.2 ± 2.3 in Sparing AMT Group was 92.4 ± 2.7. Tegner score at final follow-up was 7.2 ± 2.1 for Removing AMT Group and 7.8 ± 1.8 for Sparing AMT Group. Arthrometric evaluation performed with KT-1000 at final follow-up showed a side-to-side difference of 0.9 ± 1.3 mm in the Removing AMT Group against 0.8 ± 1.0 mm in the Sparing AMT Group. Return time to the sport was 7.1 months for Removing AMT Group otherwise 6.1 months for the Sparing AMT Group.
Conclusions
Both the described techniques in this study demonstrated to be able to guarantee a successful outcome. However, although no statistically significant differences were evident in terms of subjective and objective outcome between these techniques some evident benefits were evident using the sparing bundle technique in Sparing AMT Group such as better clinical scores at the final follow-up and an earlier return to sport activity.








Similar content being viewed by others
References
Adachi N, Ochi M, Uchio Y, Sumen Y (2000) Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg 120:128–133
Ahn JH, Wang JH, Lee YS, Kim JG, Kang JH, Koh KH (2011) Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: clinical and magnetic resonance imaging results. Arthroscopy 27:1079–1089
Amis AA, Dawkins GP (1991) Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br 73:260–267
Bak K, Scavenius M, Hansen S et al (1997) Isolated partial rupture of the anterior cruciate ligament. Long term follow-up of 56 cases. Knee Surg Sports Traumatol Arthrosc. 5(2):66–71
Bali K, Dhillon MS, Vasistha RK, Kakkar N, Chana R, Prabhakar S (2012) Efficacy of immunohistological methods in detecting functionally viable mechanoreceptors in the remnant stumps of injured anterior cruciate ligaments and its clinical importance. Knee Surg Sports Traumatol Arthrosc 20:75–80
Barrack RL, Buckley SL, Bruckner JD et al (1990) Partial versus complete acute anterior cruciate ligament tears. The results of nonoperative treatment. J Bone Joint Surg Br. 72(4):622–624
Buda R, Ferruzzi A, Vannini F, Zambelli L, Di Caprio F (2006) Augmentation technique with semitendinosus and gracilis tendons in chronic partial lesions of the ACL: clinical and arthrometric analysis. Knee Surg Sports Traumatol Arthrosc 14(11):1101–1107
Buda R, Ruffilli A, Vannini F, Parma A, Giannini S (2013) Anatomic anterior cruciate ligament reconstruction using distally inserted doubled hamstrings tendons. Orthopedics 36(6):445–449
Chen J, Chen S, Weitao Z, Yinghui H, Yunxia L (2008) Technique of arthroscopic anterior cruciate ligament reconstruction with preserved residual fibers as a graft envelope. Tech Knee Surg 7:70–77
Colombet P, Dejour D, Panisset JC, Siebold R (2010) Current concept of partial anterior cruciate ligament ruptures. Orthop Traumatol Surg Res 96:S109–S118
Crain EH, Fithian DC, Paxton EW, Luetzow WF (2005) Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy 21(1):19–24
Crawford R, Walley G, Bridgman S, Maffulli N (2007) Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull 84:5–23
Dhillon MS, Bali K, Vasistha RK (2010) Immunohistological evaluation of proprioceptive potential of the residual stump of injured anterior cruciate ligaments. Int Orthop 34:737–741
Georgoulis AD, Pappa L, Moebius U, Malamou-Mitsi V, Pappa S, Papageorgiou CO et al (2001) The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervation of the ACL autograft. Knee Surg Sports Traumatol Arthrosc 9:364–368
Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE et al (2000) Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 8:141–150
Kazusa H, Nakamae A, Ochi M (2013) Augmentation technique for anterior cruciate ligament injury. Clin Sports Med 32:127–140
Kim SJ, Jeong JH, Ko YG (2003) Synovitic cyclops syndrome caused by a Kennedy ligament augmentation device. Arthroscopy 19:38
Lee BI, Kwon SW, Kim JB, Choi HS, Min KD (2008) Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy 24:560–568
Lee BI, Min KD, Choi HS et al (2009) Immunohistochemical study of mechanoreceptors in the tibial remnant of the ruptured anterior cruciate ligament in human knees. Knee Surg Sports Traumatol Arthrosc 17:1095–1101
Lee BI, Min KD, Choi HS, Kim JB, Kim ST (2006) Arthroscopic anterior cruciate ligament reconstruction with the tibial-remnant preserving technique using a hamstring graft. Arthroscopy 22(3):340
Liljedahl SO, Lindvall N, Wetterfors J (1965) Early diagnosis and treatment of acute ruptures of the anterior cruciate ligament; a clinical and arthrographic study of forty-eight cases. J Bone Joint Surg Am 47(8):1503–1513
Liu W, Maitland ME, Bell GD (2002) A modeling study of partial ACL injury: simulated KT-2000 arthrometer tests. J Biomech Eng 124(3):294–301
Locherbach C, Zayni R, Chambat P, Sonnery-Cottet B (2010) Biologically enhanced ACL reconstruction. Orthop Traumatol Surg Res 96:810–815
Lopomo N, Signorelli C, Bonanzinga T, Marcheggiani Muccioli GM, Visani A, Zaffagnini S (2012) Quantitative assessment of pivot-shift using inertial sensors. Knee Surg Sports Traumatol Arthrosc 20(4):713–717
Muneta T, Koga H, Mochizuki T et al (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628
Noyes FR, Mooar LA, Moorman CT, McGinniss GH (1989) Partial tears of the anterior cruciate ligament. Progression to complete ligament deficiency. J Bone Joint Surg Br 71(5):825–833
Ochi M, Adachi N, Deie M, Kanaya A (2006) Anterior cruciate ligament augmentation procedure with a 1-incision technique: anteromedial bundle or posterolateral bundle reconstruction. Arthroscopy 22(4):463
Ochi M, Adachi N, Uchio Y et al (2009) A minimum 2-year follow-up after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy 25:117–122
Park SY, Oh H, Park SW, Lee JH, Lee SH, Yoon KH (2012) Clinical outcomes of remnant-preserving augmentation versus double-bundle reconstruction in the anterior cruciate ligament reconstruction. Arthroscopy 28:1833–1841
Phelan N, Rowland P, Galvin R, O’Byrne JM (2016) A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthrosc 24(5):1525–1539
Ramjug S, Ghosh S, Walley G, Maffulli N (2008) Isolated anterior cruciate ligament deficiency, knee scores and function. Acta Orthop Belg 74:643–651
Ruffilli A, Pagliazzi G, Ferranti E, Busacca M, Capannelli D, Buda R (2016) Hamstring graft tibial insertion preservation versus detachment in anterior cruciate ligament reconstruction: a prospective randomized comparative study. Eur J Orthop Surg Traumatol 26(6):657–664. https://doi.org/10.1007/s00590-016-1812-9
Siebold R, Fu FH (2008) Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy 24:1289–1298
Sonnery-Cottet B, Barth J, Graveleau N, Fournier Y, Hager JP, Chambat P (2009) Arthroscopic identification of isolated tear of the posterolateral bundle of the anterior cruciate ligament. Arthroscopy 25:728–732
Sonnery-Cottet B, Chambat P (2007) Arthroscopic identification of the anterior cruciate ligament posterolateral bundle: the figure-of four position. Arthroscopy 23(10):1128.e1–1128.e3
Sonnery-Cottet B, Lavoie F, Ogassawara R, Scussiato RG, Kidder JF, Chambat P (2010) Selective anteromedial bundle reconstruction in partial ACL tears: a series of 36 patients with mean 24 months follow-up. Knee Surg Sports Traumatol Arthrosc 18:47–51
Van Eck CF, Schreiber VM, Liu TT, Fu FH (2010) The anatomic approach to primary, revision and augmentation anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18(9):1154–1163
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22:240–251
Zaffagnini S, Golanó P, Farinas O, Depasquale V, Strocchi R, Cortecchia S, Marcacci M, Visani A (2003) Vascularity and neuroreceptors of the pes anserinus: anatomic study. Clin Anat 16(1):19–24
Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, Roberti di Sarsina T, Raggi F, Signorelli C, Urrizola F, Spinnato P, Rimondi E, Marcacci M (2017) Over-the top ACL reconstruction plus extra-articular lateral tenodesis with hamstring tendon grafts: prospective evaluation with 20-year minimum follow-up. Am J Sports Med 45(14):3233–3242
Zantop T, Brucker PU, Vidal A, Zelle BA, Fu FH (2007) Intraarticular rupture pattern of the ACL. Clin Orthop Relat Res 454:48–53
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Informed consent
The study was approved by the ethics committee of the authors’ institution, and all patients signed an informed consent form to participate in the study.
Rights and permissions
About this article
Cite this article
Buda, R., Baldassarri, M., Perazzo, L. et al. The biological respect of the posterolateral bundle in ACL partial injuries. Retrospective analysis of 2 different surgical management of ACL partial tear in a population of high-demanding sport patients. Eur J Orthop Surg Traumatol 29, 651–658 (2019). https://doi.org/10.1007/s00590-018-2312-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2312-x