Abstract
Purpose
A main concern of patients with back problems is pain and its impact on function and quality of life. These are subjective phenomena, and should be probed during the clinical consultation so that the physician can ascertain the extent of the problem. This study evaluated the agreement between clinicians’ and patients’ independent ratings of patient status on the Core Outcome Measures Index (COMI).
Methods
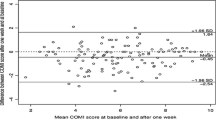
This was an analysis of the data from 5 spine specialists and 108 patients, in two centres. Prior to the consultation, the patient completed the COMI. After the consultation, the clinician (blind to the patient’s version) also completed a COMI. Concordance was assessed by % agreement, Kappa values, Bland–Altman plots, Spearman rank, Intraclass Correlation Coefficients and comparisons of mean values, as appropriate.
Results
Agreement regarding the “main problem” (back pain, leg/buttock pain, sensory disturbances, other) was 83%, Kappa = 0.70 (95%CI 0.58–0.81). Moderate/strong correlations were found between the doctors’ and patients’ COMI-item ratings (0.48–0.74; p < 0.0001), although compared with the patients’ ratings the doctors systematically underestimated absolute values for leg pain (p = 0.002) and dissatisfaction with symptom state (p = 0.002), and overestimated how much the patient’s function was impaired (p = 0.029).
Conclusion
The doctors were able to ascertain the location of the main problem and the multidimensional outcome score with good accuracy, but some individual domains were systematically underestimated (pain, symptom-specific well-being) or overestimated (impairment of function). More detailed/direct questioning on these domains during the consultation might deliver a better appreciation of the impact of the back problem on the patient’s daily life.


Similar content being viewed by others
References
Dorr Goold S, Lipkin M Jr (1999) The doctor–patient relationship: challenges, opportunities, and strategies. J Gen Intern Med 14(Suppl 1):S26-33. https://doi.org/10.1046/j.1525-1497.1999.00267.x
Tongue JR, Epps HR, Forese LL (2005) Communication skills. Instr Course Lect 54:3–9
Becerra Fontal JA, Bago Granell J, Garre Olmo J, Roig Busquets R, Peris Prats F, Villanueva Leal C (2013) Evaluation of health-related quality of life in patients candidate for spine and other musculoskeletal surgery. Eur Spine J 22:1002–1009. https://doi.org/10.1007/s00586-012-2617-0
Crawford RW, Murray DW (1997) Total hip replacement: indications for surgery and risk factors for failure. Ann Rheum Dis 56:455–457. https://doi.org/10.1136/ard.56.8.455
Quintana JM, Bilbao A, Escobar A, Azkarate J, Goenaga JI (2009) Decision trees for indication of total hip replacement on patients with osteoarthritis. Rheumatology (Oxford) 48:1402–1409. https://doi.org/10.1093/rheumatology/kep264
Allepuz A, Quintana JM, Espallargues M, Escobar A, Moharra M, Arostegui I (2011) Relationship between total hip replacement appropriateness and surgical priority instruments. J Eval Clin Pract 17:18–25. https://doi.org/10.1111/j.1365-2753.2010.01362.x
Mannion AF, Mariaux F, Pittet V, Steiger F, Aepli M, Fekete TF, Jeszenszky D, O’Riordan D, Porchet F (2021) Association between the appropriateness of surgery, according to appropriate use criteria, and patient-rated outcomes after surgery for lumbar degenerative spondylolisthesis. Eur Spine J 30:907–917. https://doi.org/10.1007/s00586-021-06725-3
Reitman CA, Hills JM, Standaert CJ, Bono CM, Mick CA, Furey CG, Kauffman CP, Resnick DK, Wong DA, Prather H, Harrop JS, Baisden J, Wang JC, Spivak JM, Schofferman J, Riew KD, Lorenz MA, Heggeness MH, Anderson PA, Rao RD, Baker RM, Emery SE, Watters WC 3rd, Sullivan WJ, Mitchell W, Tontz W Jr, Ghogawala Z (2021) Cervical fusion for treatment of degenerative conditions: development of appropriate use criteria. Spine J. https://doi.org/10.1016/j.spinee.2021.05.023
Muller D, Haschtmann D, Fekete TF, Kleinstuck F, Reitmeir R, Loibl M, O’Riordan D, Porchet F, Jeszenszky D, Mannion AF (2022) Development of a machine-learning based model for predicting multidimensional outcome after surgery for degenerative disorders of the spine. Eur Spine J 31:2125–2136. https://doi.org/10.1007/s00586-022-07306-8
Staub L, Aghayev E, Skrivankova V, Lord SJ, Haschtmann D, Mannion A, F. (2020) Development and temporal validation of a prognostic model for 1-year clinical outcome after decompression surgery for lumbar disc herniation. Eur Spine J 29:1742–1751
McGirt MJ, Bydon M, Archer KR, Devin CJ, Chotai S, Parker SL, Nian H, Harrell FE Jr, Speroff T, Dittus RS, Philips SE, Shaffrey CI, Foley KT, Asher AL (2017) An analysis from the quality outcomes database, Part 1. Disability, quality of life, and pain outcomes following lumbar spine surgery: predicting likely individual patient outcomes for shared decision-making. J Neurosurg Spine 27:357–369. https://doi.org/10.3171/2016.11.SPINE16526
Coran JJ, Koropeckyj-Cox T, Arnold CL (2013) Are physicians and patients in agreement? Exploring dyadic concordance. Health Educ Behav 40:603–611. https://doi.org/10.1177/1090198112473102
Lattig F, Fekete TF, O'Riordan D, Mannion AF (2010) Expectations of spinal surgery from the surgeon's and patient's perspectives. In: Swiss Society of Orthopaedics. St Gallen, Switzerland, pp 1040–1048
Ruben MA, Blanch-Hartigan D, Shipherd JC (2018) To Know another’s pain: a meta-analysis of caregivers’ and healthcare providers’ pain assessment accuracy. Ann Behav Med 52:662–685. https://doi.org/10.1093/abm/kax036
Perreault K, Dionne CE (2005) Patient-physiotherapist agreement in low back pain. J Pain 6:817–828. https://doi.org/10.1016/j.jpain.2005.07.008
Pierre U, Wood-Dauphinee S, Korner-Bitensky N, Gayton D, Hanley J (1998) Proxy use of the Canadian SF-36 in rating health status of the disabled elderly. J Clin Epidemiol 51:983–990. https://doi.org/10.1016/s0895-4356(98)00090-0
Kwoh CK, O’Connor GT, Regan-Smith MG, Olmstead EM, Brown LA, Burnett JB, Hochman RF, King K, Morgan GJ (1992) Concordance between clinician and patient assessment of physical and mental health status. J Rheumatol 19:1031–1037
Sneeuw KC, Sprangers MA, Aaronson NK (2002) The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease. J Clin Epidemiol 55:1130–1143. https://doi.org/10.1016/s0895-4356(02)00479-1
Hewlett SA (2003) Patients and clinicians have different perspectives on outcomes in arthritis. J Rheumatol 30:877–879
Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, Jacobshagen N, Dvorak J, Boos N (2005) Outcome assessment in low back pain: how low can you go? Eur Spine J 14:1014–1026
Ferrer M, Pellise F, Escudero O, Alvarez L, Pont A, Alonso J, Deyo R (2006) Validation of a minimum outcome core set in the evaluation of patients with back pain. Spine 31:1372–1379; discussion 1380
Deyo RA, Battié M, Beurskens AJHM, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G (1998) Outcome measures for low back pain research. A proposal for standardized use. Spine 23:2003–2013
Fankhauser C, Mutter U, Aghayev E, Mannion AF (2012) Validity and responsiveness of the Core Outcome Measures Index (COMI) for the neck. Eur Spine J 21:101–114
Mannion AF, Porchet F, Kleinstück F, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D (2009) The quality of spine surgery from the patient’s perspective: part 1. The Core Outcome Measures Index (COMI) in clinical practice. Eur Spine J 18:367–373
Abdeldaiem A, Saweeres ESB, Shehab-Eldien AA, Mannion AF, Rehan Youssef A (2020) Cross-cultural adaptation and validation of the Arabic version of the Core Outcome Measures Index for the back (COMI-back) in patients with non-specific low back pain. Eur Spine J 29:2413–2430. https://doi.org/10.1007/s00586-020-06530-4
Cohen J (1968) Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 70:213–220. https://doi.org/10.1037/h0026256
Ranganathan P, Pramesh CS, Aggarwal R (2017) Common pitfalls in statistical analysis: measures of agreement. Perspect Clin Res 8:187–191. https://doi.org/10.4103/picr.PICR_123_17
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Sullivan GM, Feinn R (2012) Using effect size-or why the P value is not enough. J Grad Med Educ 4:279–282. https://doi.org/10.4300/JGME-D-12-00156.1
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC (2007) Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 60:34–42
Bland JM, Altman DG (1995) Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet 346:1085–1087
Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW (1990) Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. JBJS A 72A:403–408
Aaen J, Austevoll IM, Hellum C, Storheim K, Myklebust TA, Banitalebi H, Anvar M, Brox JI, Weber C, Solberg T, Grundnes O, Brisby H, Indrekvam K, Hermansen E (2022) Clinical and MRI findings in lumbar spinal stenosis: baseline data from the NORDSTEN study. Eur Spine J 31:1391–1398. https://doi.org/10.1007/s00586-021-07051-4
Tabolli S, Sampogna F, Pagliarello C, Paradisi A, Spagnoli A, Abeni D (2012) Disease severity evaluation among dermatological out-patients: a comparison between the assessments of patients and physicians. J Eur Acad Dermatol Venereol 26:213–218. https://doi.org/10.1111/j.1468-3083.2011.04038.x
Frymoyer JW, Frymoyer NP (2002) Physician-patient communication: a lost art? J Am Acad Orthop Surg 10:95–105. https://doi.org/10.5435/00124635-200203000-00005
Tongue JR, Jenkins L, Wade A (2009) Low-touch surgeons in a high-touch world. In: AAOS Now. American Academy of Orthopaedic Surgeons
de Vet HC, Terwee CB, Knol DL, Bouter LM (2006) When to use agreement versus reliability measures. J Clin Epidemiol 59:1033–1039
Marquie L, Raufaste E, Lauque D, Marine C, Ecoiffier M, Sorum P (2003) Pain rating by patients and physicians: evidence of systematic pain miscalibration. Pain 102:289–296
Sari O, Temiz C, Golcur M, Aydogan U, Tanoglu A, Ezgu MC, Tehli O (2015) Pain perception differences between patients and physicians: a pain severity study in patients with low back pain. Turk Neurosurg 25:461–468. https://doi.org/10.5137/1019-5149.JTN.13481-14.1
Crocker JC, Ricci-Cabello I, Parker A, Hirst JA, Chant A, Petit-Zeman S, Evans D, Rees S (2018) Impact of patient and public involvement on enrolment and retention in clinical trials: systematic review and meta-analysis. BMJ 363:k4738. https://doi.org/10.1136/bmj.k4738
Müller D, Haschtmann D, Fekete TF, Kleinstück F, Reitmeir R, Loibl M, O’Riordan D, Porchet F, Jeszenszky D, Mannion AF (2022) Development of a machine-learning based model for predicting multidimensional outcome after surgery for degenerative disorders of the spine. Eur Spine J 31:2125–2136. https://doi.org/10.1007/s00586-022-07306-8
Macnab I (1973) Chapter 14. Pain and disability in degnerative disc disease. Clin Neurosurg 20:193–196
Lattig F, Grob D, Kleinstueck FS, Porchet F, Jeszenszky D, Bartanusz V, O’Riordan D, Mannion AF (2009) Ratings of global outcome at the first post-operative assessment after spinal surgery: how often do the surgeon and patient agree? Eur Spine J 18:386–439
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zaina, F., Mutter, U., Donzelli, S. et al. How well can the clinician appraise the patient’s perception of the severity and impact of their back problem?. Eur Spine J 33, 39–46 (2024). https://doi.org/10.1007/s00586-023-08023-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08023-6