Abstract
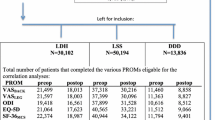
The Core Outcome Measures Index (COMI) is a short, multidimensional outcome instrument, with excellent psychometric properties, that has been recommended for use in monitoring the outcome of spinal surgery from the patient’s perspective. This study examined the feasibility of implementation of COMI and its performance in clinical practice within a large Spine Centre. Beginning in March 2004, all patients undergoing spine surgery in our Spine Centre (1,000–1,200 patients/year) were asked to complete the COMI before and 3, 12 and 24 months after surgery. The COMI has one question each on back (neck) pain intensity, leg/buttock (arm/shoulder) pain intensity, function, symptom-specific well being, general quality of life, work disability and social disability, scored as a 0–10 index. At follow-up, patients also rated the global effectiveness of surgery, and their satisfaction with their treatment in the hospital, on a five-point Likert scale. After some fine-tuning of the method of administration, completion rates for the pre-op COMI improved from 78% in the first year of operation to 92% in subsequent years (non-response was mainly due to emergencies or language or age issues). Effective completion rates at 3, 12 and 24-month follow-up were 94, 92 and 88%, respectively. The 12-month global outcomes (from N = 3,056 patients) were operation helped a lot, 1,417 (46.4%); helped, 860 (28.1%); helped only little, 454 (14.9%); did not help, 272 (8.9%); made things worse, 53 (1.7%). The mean reductions in COMI score for each of these categories were 5.4 (SD2.5); 3.1 (SD2.2); 1.3 (SD1.7); 0.5 (SD2.2) and −0.7 (SD2.2), respectively, yielding respective standardised response mean values (“effect sizes”) for each outcome category of 2.2, 1.4, 0.8, 0.2 and 0.3, respectively. The questionnaire was feasible to implement on a prospective basis in routine practice, and was as responsive as many longer spine outcome questionnaires. The shortness of the COMI and its multidimensional nature make it an attractive option to comprehensively assess all patients within a given Spine Centre and hence avoid selection bias in reporting outcomes.



Similar content being viewed by others
References
Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleas F (2000) Lumbar spinal stenosis: conservative or surgical management?: a prospective 10-year study. Spine 25:1424–1435. doi:10.1097/00007632-200006010-00016
Balague F, Mannion AF, Pellise F, Cedraschi C (2007) Clinical update: low back pain. Lancet 369:726–728. doi:10.1016/S0140-6736(07)60340-7
Beurskens AJHM, de Vet HCW, Köke AJA (1996) Responsiveness of functional status in low back pain: a comparison of different instruments. Pain 65:71–76. doi:10.1016/0304-3959(95)00149-2
Bombardier C (2000) Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine 25:3100–3103. doi:10.1097/00007632-200012150-00003
Carlson J, Youngblood R, Dalton JA, Blau W, Lindley C (2003) Is patient satisfaction a legitimate outcome of pain management? J Pain Symptom Manage 25:264–275. doi:10.1016/S0885-3924(02)00677-2
Deyo RA, Battie M, Beurskens AJHM, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G (1998) Outcome measures for low back pain research. A proposal for standardized use. Spine 23:2003–2013. doi:10.1097/00007632-199809150-00018
Ferrer M, Pellise F, Escudero O, Alvarez L, Pont A, Alonso J, Deyo R (2006) Validation of a minimum outcome core set in the evaluation of patients with back pain. Spine 31:1372–1379. doi:10.1097/01.brs.0000218477.53318.bc (discussion 1380)
George SZ, Hirsch AT (2005) Distinguishing patient satisfaction with treatment delivery from treatment effect: a preliminary investigation of patient satisfaction with symptoms after physical therapy treatment of low back pain. Arch Phys Med Rehabil 86:1338–1344. doi:10.1016/j.apmr.2004.11.037
Grob D, Kleinstuck F, Lattig F, Porchet F, Bartanusz V, Jeszenszky D, Mannion AF (2009) The patient’s perspective on complications after spine surgery. Eur Spine J (this issue)
Hakkinen A, Ylinen J, Kautiainen H, Airaksinen O, Herno A, Kiviranta I (2003) Does the outcome 2 months after lumbar disc surgery predict the outcome 12 months later? Disabil Rehabil 25:968–972. doi:10.1080/0963828031000122258
Mannion AF, Elfering A (2006) Predictors of surgical outcome and their assessment. Eur Spine J 15(Suppl 1):S93–S108. doi:10.1007/s00586-005-1045-9
Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, Jacobshagen N, Dvorak J, Boos N (2005) Outcome assessment in low back pain: how low can you go? Eur Spine J 14:1014–1026. doi:10.1007/s00586-005-0911-9
Mannion AF, Denzler R, Dvorak J, Muntener M, Grob D (2007) A randomised controlled trial of post-operative rehabilitation after surgical decompression of the lumbar spine. Eur Spine J 16:1101–1117. doi:10.1007/s00586-007-0399-6
Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Dvorak J, Jacobshagen N, Semmer NK, Boos N (2007) Predictors of multidimensional outcome after spinal surgery. Eur Spine J 16:777–786. doi:10.1007/s00586-006-0255-0
McGregor AH, Hughes SPF (2002) The evaluation of the surgical management of nerve root compression in patients with low back pain. Part 1: The assessment of outcome. Spine 27:1465–1470. doi:10.1097/00007632-200207010-00018
Ostelo RW, de Vet HC (2005) Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol 19:593–607. doi:10.1016/j.berh.2005.03.003
Stratford PW, Spadoni G, Kennedy D, Westaway C, Alcock GK (2002) Seven points to consider when investigating a measure’s ability to detect change. Physiother Can 54:16–24
White P, Lewith G, Prescott P (2004) The core outcomes for neck pain: validation of a new outcome measure. Spine 29:1923–1930. doi:10.1097/01.brs.0000137066.50291.da
Zanoli G, Strömqvist B, Padua R, Romanini E (2000) Lessons learned searching for a HRQoL instrument to asses the results of treatment in persons with lumbar disorders. Spine 25:3178–3185. doi:10.1097/00007632-200012150-00013
Conflict of interest statement
None of the authors has any potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mannion, A.F., Porchet, F., Kleinstück, F.S. et al. The quality of spine surgery from the patient’s perspective. Part 1: The Core Outcome Measures Index in clinical practice. Eur Spine J 18 (Suppl 3), 367–373 (2009). https://doi.org/10.1007/s00586-009-0942-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-0942-8