Abstract
Introduction
The decision to instrument to L5 or ilium, in NMS, is usually based on radiologic factors, including pelvic obliquity (PO) > 15°, apex of curvature < L3, and Cobb angle > 60°. Since scoliosis in these patients is caused by a neurologic disease, we based our decision to stop at L5 on the presence of spasticity or flaccidity.
Patients & Methods
The senior author did 109 primary fusions in NMS. Of those with DMD or SMA only 16% were instrumented to the ilium. The main factor for our decision was the correction potential of the truncal shift and PO in the supine traction radiographs and the absence of severe spasticity.
Results
The 57 patients with DMD/SMA had a mean preoperative curvature of 68°, PO of 17°, and truncal shift of 20°. 74% should have been instrumented to the pelvis, but only 16% were. Those instrumented shorter as the rule, were corrected from 74° to 26° and had a postoperative PO of 8°. There was no significant difference in postoperative correction and PO compared to those instrumented to L5 on standard protocol. Subsequent extension to the pelvis was needed in 1 CP patient. There were no significant changes after 2 years. Of the 20 patients instrumented to the pelvis 11 had cerebral palsy and a preop curvature of 89°, a PO of 21° and a truncal shift of 25°.
Discussion
The decision on instrumentation length should take flexibility and disease into consideration. If the trunk is centred over the pelvis, deterioration will not occur in absence of spasticity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The goal of scoliosis correction in neuromuscular scoliosis is a straight spine over a level pelvis in order to maintain sitting balance in a mostly wheelchair-bound population. An old controversy is whether to include the pelvis in the fusion [1,2,3,4]. The pelvis is a strong basis for the spinal fusion and its inclusion facilitates the control of the pelvic obliquity and makes it predictable [5,6,7,8,9]. On the other hand it prolongs the operation, increases blood loss [10] and reduces mobility. Also it increases the risk for infection due to proximity to the rectum in a population where incontinence is a frequent problem [11]. Thus some authors advocate shorter fusions to L5 [3, 12,13,14,15]. Luk et al. already mentioned in 1986 that fusion to L5 could be sufficient to correct the main proportion of the pelvic obliquity in NMS due to the role of the iliolumbar ligament which holds the L5 vertebra in a relatively constant relationship with the sacrum [16]. Takaso et al. postulated that fusion to L5 is safe in patients with SMA in absent of high preoperative pelvic obliquity, but the amount of PO that can be considered safe remains unclear [15]. Takaso et al. suggested that segmental pedicle screw instrumentation to L5 was safe in patients with DMD with stable L5/S1 articulation and a minimal L5 tilt of 15° or less [14].
Most surgeons base their decision on radiologic parameters. It is recommended to include the pelvis if the curve exceeds 60°, the apex is L4 or lower or the pelvic obliquity is above 15° [1, 4, 12,13,14, 17]. These recommendations do not consider the cause and origin of the curvature. Often cases of neuromuscular scoliosis are regarded as a single entity and are only looked upon in contrast to idiopathic or congenital types. This neglects the fact that the deformity of the spine is only a symptom of the underlying neurological and muscular disease and that there is a difference between spastic paralysis or muscular diseases.
The Scoliosis Research Society Classification of Neuromuscular Spinal Deformities differentiates between primary neuropathies caused by lesions of the upper or lower motor neuron and myopathies like muscular dystrophies (Table 1) [18, 19]. A lesion of the upper motor neuron as in CP patients comes with a loss of inhibitory input causing spasticity [20, 21]. In patients with lesions of the lower motor neuron (e.g. SMA) or in myopathic conditions (e.g. DMD) the descending inhibitory tracts are still intact resulting in a reduced muscle tone. Therefore, it is sensible to divide neuromyopathic patients in those with spasticity (like CP) and those with a flaccid condition like DMD and SMA.
Furthermore, there was a development and improvement of the surgical techniques and implants since these recommendations to include the pelvis in the fusion were published. Even in textbooks of 2008 [22] the unit rod and Galveston or Dunn-Mc Carthy technique were described to correct NMS. Now that segmental pedicle screws and either ilium screws or S2AI screws are the new standard, we must rethink this. Especially the added value of pelvic fixation surgery remains unclear and patients which are fused to the pelvis have a higher risk for complications [23]. But secondary revision to the pelvis has even more complications than including the pelvis at the index surgery [11]. Thus the question whether to include the pelvis or not still is open to discussion. In a Cochrane review of 2015 Cheuck et al. wrote on this matter that in absence of evidence clinicians may need to consider anecdotal evidence and their personal experience as well as expert opinion as guidance for their decision on the best care for an individual patient [24].
In our hospital we started to base our decision more on the flexibility of the curve and on the muscle tone. In patients with lowered tonicity as in SMA and DMD, we usually stop at L5 and in patients with high tonicity as in CP we usually include the pelvis. After doing so for several years we want to describe our decision pathway and experiences in order to help other surgeons in their decision pathway.
Patients and methods
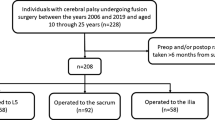
Between 2014 and 2021 the senior author operated on 127 cases of neuromuscular scoliosis in outgrown patients. Inclusion criteria were a primary fusion due to scoliosis and a distinct assignment to either spasticity or flaccid palsy. Excluded were revision cases, all prepubertal patients with non-fusion procedures like growing rods and VEPTR, diseases with predominant kyphosis like MMC or rare syndromes. Seventy-six patients remained, of which 57 had a muscle weakness (53% DMD, 21% SMA, 26% other muscle dystrophies) and 19 patients had CP. Two groups as described in Table 2 were compared.
The average age of our patients was 15 years (min 9y, max 28 y, SD 3.2y). On average they weighed 48 kg and were 154 cm tall, the mean BMI was 20 kg/m [2]. Patients with degenerative muscle disease or SMA were significantly younger, heavier and taller than those with CP (Table 2). This can be explained by the nutritional status as well as corticoid medication.
In a subgroup analysis we looked at those patients which traditionally should have been fused to the ilium but were only fused to L5. They had a pelvic obliquity > 15°, a curve > 60° and an apex lower than L4. 87% of these patients had muscular dystrophy and only 13% CP.
Radiological parameters and data analysis
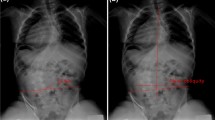
The spinal images were measured preoperatively, immediate postoperatively, as well as 1 and 2 years after the procedure. Preoperative images were taken in all patients, sitting or lying down, depending on their mobility. In addition, we arranged for a traction image to estimate the flexibility and possible correction. INFINITT PACS was used to measure the pelvic obliquity, the truncal shift, the main curvature with the corresponding apex and the L4-take-off (Fig. 1).
Example of a 15 y old boy with a NMS of 71° in sitting position due to muscular dystrophy (a). Curvature corrects to 36° under traction, while PO corrects from 20° to 8° (b) Directly postop (c) the scoliosis is corrected to 25° and the PO to 7°. After 3 years of follow-up (d) the correction is maintained in sitting position
Subsequently, the flexibility, the postoperative correction and the Cincinnati Correction Index were calculated as proposed by Vora et al.: [25]
The analysis of the data was done with IBM SPSS Statistics (Version 20). The Chi-square test, the Independent-Samples T-test and the ANOVA for mean comparisons of more than 2 groups were applied. Significance was set at p < 0.05.
Follow-up
All patients were seen for follow-up at least after 3 month, one and two years for clinical evaluation. X-rays in sitting position after one and two years were evaluated by two independent doctors. A change of the sitting position of > 10° was considered clinically relevant. Additionally, a clinical change in sitting position was evaluated and all those patients which were not satisfied and demanded revision and secondary lengthening to the pelvis were counted as failures.
Results
Most patients showed the large C-shaped curvatures typical for neuromuscular scoliosis. The apex of the main curve was thoracic (higher than Th12) in 26.3% of the cases, thoracolumbar (Th12/L1) in 30.0% and lumbar (lower than L1) in 43.8% of the cases.
Primary posterior pedicle screw-based spondylodesis was performed in all patients. In 76 of the 79 cases, instrumentation to the lower lumbar spine (L4/5) or to the pelvis was done. In 3 of the patients, the lowest instrumented vertebra (LIV) was chosen above the L4 level. As these were rather short thoracic curvatures, they were excluded from further analysis.
As shown in Table 3 there was a tendency for patients with cerebral palsy to have a slightly lower apex of curvature than those with DMD or SMA. However, this difference was not statistically significant (p = 0.536). Patients with flaccid palsy had an average major curve of 68° preoperatively in the sitting position, which corrected to an average of 46° in traction images. In patients with CP, the Cobb angle of the major curve was 89° preoperatively in sitting position and 60° under bending/traction. The difference in preoperative curvature between sitting (p = 0.001) and bending/traction (p = 0.021) was statistically significant. Patients with flaccid palsy had a preoperative pelvic obliquity of 16.6° in sitting position and 11.6° under bending/traction. This was similar with CP patients (20.6° in sitting and 11.1° under bending/traction).
The L4-take-off was significantly higher in patients with CP (39.9°) than with flaccid palsy (30.5°) and was corrected to similar values of 25.4° and 21.6° under traction. The truncal shift was higher in CP patients in the sitting position (25.4° to 19.0°) but smaller under traction (10.1° to 12.4°). All in all there were no significant preoperative differences between patients with DMD or SMA and CP concerning truncal shift.
When traction and sitting films were compared, patients with flaccid palsy had a slightly higher flexibility, although the differences did not reach the significance level (Table 3).
Of the patients with degenerative muscle disease or SMA, 84.2% were instrumented to the lower lumbar spine and only 15.8% to the ilium, whereas those with spastic palsy were instrumented to the ilium in 58%. Patients with degenerative muscle diseases had an average postoperative major curve (in sitting) of 27° compared to 40° in CP patients. Although the pelvis was not included in the majority of the patients, the PO and the truncal shift could be corrected to an average of 8°. While patients with CP had an average pelvic obliquity of 12° and a trunk shift of 17°.
In addition, the percentage of operative correction (POC) and the Cincinnati correction index (CCI) were calculated for the main curve (Table 2). Although there was a significant difference in postoperative major curve and trunk shift, there was no statistically significant difference in POC and CCI. This means that the extent of correction was comparable in both subgroups, which can be explained by the fact that CP patients also had a greater initial spinal deformity.
For SMA and DMD patients instrumented to L5 the mean operative time was 202 min, for those instrumented to the ilium it was 258 min and for CP patients instrumented to the ilium we needed an average cut-suture-time of 289 min.
A subgroup analysis was performed on patients who were instrumented to L5 although according to previous criteria fusion to the pelvis should have been done (we called it the “new lumbar group”). This subgroup was compared to patients who were stabilized to the ilium (pelvic group) and those who even according to conventional criteria only required correction to the lower lumbar spine (traditional lumbar group).
This “new lumbar group” of 38 patients was analysed more closely regarding preoperative conditions and postoperative outcome (Table 4). 33 of these patients (87%) had a flaccid palsy and only 5 had cerebral palsy with spasticity (13%).
Patients of the “new lumbar group” had mainly DMD or SMA and were more flexible in traction radiographs. The preoperative curvature of 74° ranged between pelvic group (90°) and traditional lumbar group (50°). Flexibility was not significantly higher in the new lumbar group than in the other two. But the remaining curve in the traction film was still 46° and thus higher than in the traditional lumbar group 5. In patients we fused to the ilium the main curvature remained above the critical mark of 60° even under traction (62°). The difference in the 3 groups was significant (p = 0.002).
The pelvic obliquity under traction corrected to 11° in the “new lumbar group” and thus ranged clearly below the cut-off of 15°. Those who were only corrected to a mean of 14.5° under traction were fused to the pelvis. Similarly clear values were shown regarding the L4 take-off and the trunk shift in bending/traction images (Table 4).
In the “new lumbar group” a correction of 66% to a mean of 26,8° was achieved. This resulted in balanced spine with a pelvic obliquity of 8,1° and a postoperative trunk shift of 8,3°. The postop results were similar to those of the patients which primarily met the criteria to fusion to L5 (Table 4).
After one and two years of follow-up no significant change in the pelvic parameters was seen in one of the three groups (Table 4). The influence of the spasticity is displayed in the boxplot (Fig. 2). None of the patients had an increase in pelvic obliquity of more than 10° after one- or two-year follow-up. One patient with CP had to be revised and fused to the pelvis due to screw loosening in L5. As radiography only reflects a moment, we asked all patients how they get along in daily life and whether they feel stable. None felt an increasing instability or worsening of the sitting position and thus wished for secondary lengthening. An example is given in Fig. 1.
Discussion
Our experience showed instrumentation and fusion can be performed shorter than the sacrum or pelvis more often than previously assumed, provided that the spine can be centred over the pelvis, good correction is achieved, and high muscle tension or spasticity are absent. As revision surgery shows higher rates of implant failure [11] a thorough consideration of the extent of stabilization is paramount. The criteria commonly used to decide whether to include the pelvis or not only considered the static conditions and the preoperative X-rays [26]. Radiological parameters that are suggested are the pelvic obliquity, L5 tilt, apex of the curve and trunk shift [1, 2, 4, 7, 12,13,14, 17, 27,28,29]. Mehta et al. also suggest to take the age of the patient into consideration [13]. Takaso et al. also measured preop flexibility but did not draw any conclusions from it concerning the extent of stabilization [14]. Modi et al. and Whitaker et al. suggested to go to the pelvis in patients with pelvic obliquity > 15° or in the presence of severe lower extremity contractures, but did not regard the flexibility and possibility of the patient to stay centred [4, 26]. Ahmady et al. suggest to differentiate between ambulatory and non-ambulatory patients when deciding between distal spinal and pelvic anchors of growth-friendly implants in children with hypotonic NMS [30]. Douleh et al. in their 2021 literature review concluded that fusion shorter than the pelvis can be considered in minimally ambulatory patients with NMS with adequate head control, the absence of hip subluxation or dislocation and with a pelvic obliquity of less than 15° [31]. Moon et al. emphasized the importance of the correction of the pelvic obliquity to address and improve the patients primary needs like sitting and walking and combine posterior correction to the sacrum with anterior lumbosacral junction release and fusion [32].
However, the patient as an entity must be regarded, and this includes both the underlying disease and the flexibility of the deformity. We were able to show in our study that taking these aspects into account, an instrumentation to the lumbar spine is possible in selected patients without having to compromise the sitting balance and the correction.
The traditional recommendation was to fuse from the upper thoracic spine to the pelvis in non-ambulatory patients [3, 5, 6]. In former days correction was achieved mainly by Luque wires and hooks and the pelvis was needed as a base for correction. Those who stayed shorter than the pelvis advocated for very early surgery, as smaller and flexible curves could balance over the pelvis even with shorter fusion [1, 27]. We now showed that this is not limited to early stages and small curvatures of < 30° but is possible even in later surgery if the spine can be centred over the pelvis.
Former publications up to the beginning of this century recommend the unit rod or Galveston technique for NMS [22]. Pedicle screw instrumentation was used in the last decade, but long surgical time and high complication rates were described [2, 4, 27, 28, 33,34,35]. With growing experience operative time and complications decreased so these recommendations need a re-evaluation. In our group of patients with lowered muscle tension (mostly DMD or SMA) the segmental pedicle screw constructs down to L5 took an average of 202 min, ranging from 139 to 315 min. The procedure was prolonged by extension to the pelvis using mostly S2AI screws to 258 ± 39 min. This is longer than for most AIS surgeries which we contribute mainly to the more complex preparation in NMS patients. Especially in DMD the thoracic spine is sometimes hard to reach as it is superimposed by the ribs on both sides. But surgical time and blood loss was lower in our all-screw constructs than in earlier reports of screws in NMS. Stiehl et al. (who operated mainly on CP patients) reported an operative time of 344 ± 99 and blood loss of 1503 ml while Modi et al. who reported only on flaccid NMS in DMD and SMA, had 358 min cut-suture-time and 3003 ± 1634 ml blood loss, respectively [28]. The higher blood loss in DMD is typical due to the absence of dystrophin in in arterial smooth muscle and the resulting decrease in contractile function [36]. Bleeding often starts when osteotomies are done or pedicles are opened. Therefore, a quick and subtle technique is necessary. Although our surgical time was quicker, and similar to those reported with Luque wires, [1] we still had an estimated blood loss of 1405 ± 735 ml. Stopping at L5 reduces surgical time and blood loss but should not impair the outcome.
If ilium fixation is not used, a good pre-selection of the patients is necessary considering the flexibility and the expected correction of the main curve and PO. The underlying disease should also be considered, especially whether it is a disease with rather atonic flaccid paralysis (Duchenne muscular dystrophy, SMA, etc.) or with spasticity (cerebral palsy). In our experience, instrumentation can usually be shorter for degenerative muscle diseases or SMA than for spastic paralyses. In our follow-ups 1 and 2 years after the procedure so far, we did not observe any significant deterioration in sitting balance or pelvic obliquity with the exception of one CP patient which had to be fused to the pelvis due to screw loosening in L5.
Unlike idiopathic scoliosis, where the curvature is the result of a mostly pubertal growth disorder, in NMS it is the secondary result of the underlying disease. Patients with SMA or DMD are unable to stabilize themselves. Due to low muscle tone, the spine collapses and the patient tilts to the side. However, the curvature is often flexible, especially if surgery is not performed too late. In these cases, by correction of NMS the spine centres itself over the pelvis and the pelvic obliquity corrects spontaneously. This can be simulated by preop traction radiographs. In 33 of the 42 patients who had a severe pelvic obliquity while sitting, we were able to centre the patient over the pelvis by straightening the spine without including the pelvis in the fusion.
Patients instrumented to the lumbar spine had a mean postop pelvic obliquity of only 8°. This was independent of the preoperative pelvic obliquity in sitting position which was 8° in the L5 subgroup and 19° in the “new lumbar” subgroup. Other authors, which used pelvic fixation on a regular basis reported on similar postop obliquity but longer surgical time [28]. Likewise we did not find a significant difference in the two subgroups in postoperative L4 take-off and trunk shift, which indicates that the preop X-ray in sitting position is a poor prognostic factor for postop balance and pelvic obliquity in patients with flaccid NMS. In this population curvature and pelvic obliquity are a result of the collapse of the spine and not so much of the spine shape itself if surgery is not done too late.
This is different in CP with strong muscular tone and spasticity. In these patients the spine is pulled into a curve by the muscle contractions. Since the muscles are attached to the pelvis and lower limbs, straightening of the spine can increase the pelvic obliquity. Therefore, in these patients, the pelvis must usually be included in the fusion. In our collective their curvatures were more pronounced (89°) and more rigid. Only in a few cases with little and well-treated spasticity instrumentation to L5 was possible. However, of the 54 cases we fused to L5, one had to be lengthened to the pelvis within 2 years due to screw loosening and to improve sitting ability. A big problem with CP patients is that they are often operated on rather late, although it is known that the scoliosis cannot be influenced by conservative measures such as bracing or physiotherapy. This delay causes an increased surgery time. In addition, these patients often have multiple concomitant diseases and a poor nutritional status, which prohibits overly extensive osteotomies. Together with the high rigidity, this explains the poorer correction rate and outcome in these deformities.
Including the pelvis does not only affect surgical time and blood loss but may lead to other complications such as screw impingement, pressure sores, painful hardware, pseudarthrosis of the lumbosacral junction and “windshield wipering” as well as deep wound infections caused by a dissection of muscles reaching down in the diaper area of the patient [3, 23, 28, 33]. Complication rates of up to 59% [37] and even 79% [23] were reported. Therefore, it is paramount to select those patients who really need pelvic fixation surgery carefully.
Some authors advocate that instrumentation to L5 was safe in flaccid NMS [15, 38]. Takaso et al. reported on a spontaneous correction of PO from 13 to 5° in a small series of 20 patients with DMD [14]. But these recommendations are merely based on ap sitting x-rays and they only use this technique for mild curves with apex above L2 and L5 tilt < 15° [38] and low PO [15]. In their small series of 16 patients with SMA Takei et al. could not determine a cut-off value for Cobb angle or PO in which instrumentation to L5 would be effective [15].
Nielsen et al. compared primary and revision surgery to the pelvis and found a similar correction of PO in secondary revision but a higher complication rate [11]. They state that for these patients with borderline PO the benefits of improved lumbosacral mobility may outweigh the risk of future revision surgery, for those which might progress they still recommend fusion to the pelvis. But they cannot define where this border might be [11]. We think that our work can help in defining those patients by taking flexibility, muscle tone and the primary disease into account.
Mubarak et al. had similar PO in fusion to the pelvis or L5 in a small group of patients with DMD with only 29° Cobb angle and thus recommend early surgery [1], as well as Sengupta et al. who fused 19 patients to L5 with an average cobb angle of 19.8° and significantly younger than those instrumented to the pelvis [27]. Mehta et al. found a spontaneous correction of PO from 10.5 to 8.5° when pelvic fixation was not performed and from 25.8° to 11° with pelvic fusion. 15° was used as cut off point for their decision [13]. All available studies report on a relatively small patient population [8, 15, 17] or included patients from different surgeons [27].
The strength of our study is the relatively high number of patients operated on by a single surgeon in a short period compared to other papers. Furthermore, we had a preoperative plan to when to include the pelvis or not and could evaluate this in a prospective manner rather than evaluating ex-post on which group of patients excluding the pelvis worked out or not. Third we distinguished between patients with spasticity and flaccid NMS which we did not see in other papers. Either only DMD patients were considered, or all NMS were seen as a uniform group but the surgical considerations were not based on the primary disease.
The weakness is the short follow-up with a minimum of 2 years and as always larger numbers of patients would be of advantage. Nevertheless, we will progress on our way of selecting fusion levels according to primary disease and flexibility and will hopefully be able to report on long-time results and bigger populations soon.
Conclusion
We showed that if a good correction of the scoliosis in patients with flaccid paralysis was achieved this results in a stable sitting position with a centred spine over a levelled pelvis. This can be simulated with preop traction films. Patients with spasticity or insufficient correction of curve and pelvic obliquity on traction films will still benefit from fusion to the pelvis. But a static x-ray in sitting or prone position is not sufficient to decide on this matter. The underlying disease, flexibility and a clinical examination including subpelvic reasons for obliquity must always be included (Table 5).
References
Mubarak SJ, Morin WD, Leach J (1993) Spinal fusion in Duchenne muscular dystrophy: fixation and fusion to the sacropelvis? J Pediatr Orthop 13:752–757
Stiel N, Özden J, Ridderbusch K et al (2020) Pedicle screw instrumentation with or without pelvic fixation in neuromuscular scoliosis: outcome and complications in a series of 37 patients with a minimum 2-year follow-up. The Surgeon 18(5):1–12
Anari JB, Spiegel DA, Baldwin KD (2015) Neuromuscular scoliosis and pelvic fixation in 2015: where do we stand? World J Orthop. 6(8):564–566. https://doi.org/10.5312/wjo.v6.i8.564
Modi HN, Suh SW, Song HR, Fernandez HM, Yang JH (2008) Treatment of neuromuscular scoliosis with posterior-only pedicle screw fixation. J Orthop Surg 3(23):1–8
Sponseller PD, Zimmerman RM, Ko PS et al (2010) Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine 35(20):1887–1892
Chang TL, Sponseller PD, Kebaish KM, Fishman EK (2009) Low profile pelvic fixation anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine 34(5):436–440
Ravindra VM, Mazur MM, Brockmeyer DL et al (2020) Clinical effectiveness of S2-alar iliac screws in spinopelvic fixation in pediatric neuromuscular scoliosis: systematic literature review. Glob Spine J 10(8):1066–1074
Hahn F, Hauser D, Espinosa D, Blumenthal S, Min K (2008) Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J 17:255–261
Drake L, Sukkarieh H, McDonald T et al (2022) Effect of pelvic fixation on ambulation in children with neuromuscular scoliosis. World J Orthop 13(8):753–759
Weissmann KA, Lafage V, Pitaque CB et al (2021) Neuromuscular scoliosis: comorbidities and complications. Asian Spine J 15(6):778–790
Nielsen E, Andras LM, Bellaire LL et al (2018) Don’t you wish you had fused to the pelvis the first time: a comparison of reoperation rate and correction of pelvic obliquity. Spine 44(8):465–469
Mc Call RE, Hayes B (2005) Long-term outcome in neuromuscular scoliosis fused only to lumbar 5. Spine 30(18):2056–2060
Mehta SS, Modi HN, Srinivasalu S et al (2009) Pedicle screw-only constructs with lumbar or pelvic fixation for spinal stabilization in patients with Duchenne muscular dystrophy. J Spinal Disord Tech 22(6):428–433
Takaso M, Nakazawa T, Imura T et al (2010) Can the caudal extent of fusion in the surgical treatment of scoliosis in Duchenne muscular dystrophy be stopped at lumbar 5? Eur Spine J 19:787–796
Takei S, Miyagi M, Saito W et al (2018) Safety and efficacy of treatment for scoliosis is secondary to spinal muscular atrophy fused to lumbar 5 level. Spine Surg Relat Res 2(4):294–298
Luk KDK, Ho HC, Leong JCY (1986) The iliolumbar ligament: a study of its anatomy, development and clinical significance. J Bone Jt Surg Br 68(2):197–200
Takaso M, Nakazawa T, Imura T et al (2010) Two-year results for scoliosis secondary to Duchenne muscular dystrophy fused to lumbar 5 with segmental pedicle screw instrumentation. J Orthop Sci 15:171–177
Newton P (2023) Neuromuscular scoliosis. etext.srs.org/book/Accessed May 31, 2023
Allam AM, Schwabe AL (2013) Neuromuscular scoliosis. Am Acad Phys Med Rehabil 5(11):957–963
Koman AL, Paterson Smith B, Shilt JS (2004) Cerebral palsy. Lancet 363(9421):1619–1631
Sanger TD, Delgado MR, Gaebler-Spira D, Hallet M, Mink JW (2003) Classification and definition of disorders causing hypertonia in childhood. Pediatrics 111(1):89–97
Kim DH (2008) Surgery of the pediatric spine, 5th edn. Thieme Medical Publishers, Inc, New York
Strom SF, Hess MC, Jardaly AH, Conklin MJ, Gilbert SR (2022) Is it necessary to fuse to the pelvis when correcting scoliosis in cerebral palsy? World J Orthop 13(4):365–372
Cheuk D, Wong V, Wraige E, Baxter P, Cole A (2015) Surgery for scoliosis in Duchenne muscular dystrophy (Review). Cochrane Database Syst Rev 10
Vora V, Crawford A, Babekhir N et al (2007) A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs. Spine 32(17):1869–1874
Whitaker C, Burton DC, Asher M (2000) Treatment of selected neuromuscular patients with posterior instrumentation and arthrodesis ending with lumbar pedicle screw anchorage. Spine 25(18):2312–2318
Sengupta DK, Mehdian SH, McConnell JR, Eisenstein SM, Webb JK (2002) Pelvic or lumbar fixation for the surgical management of scoliosis in Duchenne muscular dystrophy. Spine 27(18):2072–2079
Modi HN, Suh SW, Hong JY, Cho JW, Park JH, Yang JH (2010) Treatment and complications in flaccid neuromuscular scoliosis (Duchenne muscular dystrophy and spinal muscular atrophy) with posterior-only pedicle screw instrumentation. Eur Spine J 19:384–393
Smucker JD, Miller F (2001) Crankshaft effect after posterior spinal fusion and unit rod instrumentation in children with cerebral palsy. J Pediatr Orthop 21:108–112
Ahmady A, Rosenthal L, Abraham AC, et al. (2023) Comparison of distal spine anchors and distal pelvic anchors in children with hypotonic neuromuscular scoliosis treated with growth-friendly instrumentation. J Pediatr Orthop Online ahead of print.
Douleh DG, Greig D, Thompson R, Garg S (2021) When should instrumentation to the pelvis be considered in minimally ambulatory adolescents with neuromuscular scoliosis? J Pediatr Orthop 41(Suppl 1):53–58
Moon ES, Nanda A, Park JO et al (2011) Pelvic obliquity in neuromuscular scoliosis. Spine 36(2):146–152
Matsumoto M, Miyagi M, Saito W et al (2018) Perioperative complications in posterior spinal fusion surgery for neuromuscular scoliosis. Spine Surg Relat Res 2(4):278–282
Modi HN, Suh SW, Yang JH et al (2009) Surgical complications in neuromuscular scoliosis operated with posterior- only approach using pedicle screw fixation. Scoliosis 4(11):1–9
Sharma S, Wu C, Andersen T, Wang Y, Hansen ES, Bünger CE (2013) Prevalence of complications in neuromuscular scoliosis surgery: a literature meta-analysis from the past 15 years. Eur Spine J 22:1230–1249
Noordeen MHH, Haddad FS, Muntoni F, Gobbi P, Hollyer JS, Bentley G (1999) Blood loss in duchenne muscular dystrophy: vascular smooth muscle dysfunction? J Pediatr Orthop 8(3):212–215
Phillips JH, Gutheil JP, Knapp DR (2007) Iliac screw fixation in neuromuscular scoliosis. Spine 32(14):1566–1570
Saito W, Inoue G, Shirasawa E, et al. Limitations of posterior spinal fusion to L5 for flaccid neuromuscular scoliosis focusing on pelvic obliquity. Scoliosis Res Soc
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received for this report.
Author information
Authors and Affiliations
Contributions
AH, AW, JE and FG participated in the conception and design of this paper and were involved in drafting and revising the manuscript. JE, AF and FG performed the final revisions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Geiger, F., Eberl, J., Wirries, A. et al. The indication of fusion to the pelvis in neuromuscular scoliosis is based on the underlying disease rather than on pelvic obliquity. Eur Spine J 32, 4063–4072 (2023). https://doi.org/10.1007/s00586-023-07943-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07943-7