Abstract
Purpose
To develop and test synthetic vertebral stabilization techniques (“vertebropexy”) that can be used after decompression surgery and furthermore to compare them with a standard dorsal fusion procedure.
Methods
Twelve spinal segments (Th12/L1: 4, L2/3: 4, L4/5: 4) were tested in a stepwise surgical decompression and stabilization study. Stabilization was achieved with a FiberTape cerclage, which was pulled through the spinous process (interspinous technique) or through one spinous process and around both laminae (spinolaminar technique). The specimens were tested (1) in the native state, after (2) unilateral laminotomy, (3) interspinous vertebropexy and (4) spinolaminar vertebropexy. The segments were loaded in flexion–extension (FE), lateral shear (LS), lateral bending (LB), anterior shear (AS) and axial rotation (AR).
Results
Interspinous fixation significantly reduced ROM in FE by 66% (p = 0.003), in LB by 7% (p = 0.006) and in AR by 9% (p = 0.02). Shear movements (LS and AS) were also reduced, although not significantly: in LS reduction by 24% (p = 0.07), in AS reduction by 3% (p = 0.21). Spinolaminar fixation significantly reduced ROM in FE by 68% (p = 0.003), in LS by 28% (p = 0.01), in LB by 10% (p = 0.003) and AR by 8% (p = 0.003). AS was also reduced, although not significantly: reduction by 18% (p = 0.06). Overall, the techniques were largely comparable. The spinolaminar technique differed from interspinous fixation only in that it had a greater effect on shear motion.
Conclusion
Synthetic vertebropexy is able to reduce lumbar segmental motion, especially in flexion–extension. The spinolaminar technique affects shear forces to a greater extent than the interspinous technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most frequently used surgical treatment modalities for spinal disorders is spinal fusion, which involves internal rigid fixation of the spine with screws and rods and bony fusion. Posterior spinal fusion produces reliable short-term results with rapid pain relief and positive effects on patient outcome [1]. However, they inherit the disadvantages of implant-related complications, painful pseudarthrosis, screw loosening and adjacent segment disease [2,3,4,5], with one-third of patients requiring reoperation within 15 years [6].
In the past, the increasing biomechanical understanding of the problems associated with fusion surgery has led to a growing interest in the use of motion preserving implants [7]. However, so far, neither lumbar intervertebral prostheses nor dynamic stabilization techniques [8, 9] provided convincing long-term results, superior to those of spinal fusion. Their surgical approach also proved to be more difficult than for spinal fusion. Some recent studies showed high reoperation rates and low cost-effectiveness of motion preserving spinal procedures [7, 8], which is why these techniques have not gained acceptance in clinical practice broadly.
With the knowledge of the above-mentioned disadvantages and problems, a new treatment modality was recently developed by Farshad et al. [10], based on orthopedic principles of soft tissue stabilization of bony structures and joints: ligamentous reinforcement of vertebral bodies, the so called “vertebropexy”. The goal of vertebropexy is to achieve targeted stabilization of the spine by inserting ligamentous grafts to counteract degeneration-related or iatrogenic (e.g., decompression) instability, but without immobilizing the segment. In particular, this is intended to achieve passive stability in clinically important directions of motion such as flexion–extension and shear movements, but without stiffening other directions of motion. Because instability is associated with excessive motion and pain [11], the stabilizing procedure should achieve clinically good results without the disadvantages of implant- and fusion-related complications. First clinical cases have shown very promising results, but reports on long-term outcome are missing. A similar technique was first successfully applied to the cervical spine to stabilize the head of a patient with dropped head syndrome [12]. Also in the lumbar spine, the biomechanical goal of selective stabilization has been successfully demonstrated in cadaveric experiments [10].
If the concept of ligamentous and “soft” reinforcement of spinal segments becomes established, an alternative to allografts is needed, as these are not widely available. We therefore asked: (1) can comparable results be achieved with available synthetic material, (2) can vertebral segmental stability be further improved by a different fixation technique and (3) how does the segmental range of motion after semi-rigid fixation with synthetic material compare with a standard dorsal fusion procedure?
These questions were addressed biomechanically with use of a validated experimental setup.
Materials and methods
Dissection, preparation and storage
The study was approved by the responsible investigational review board. Twelve spinal segments (Th12/L1: 4, L2/3: 4, L4/5: 4) originating from five fresh frozen cadavers (Table 1; Science Care, Phoenix, AZ, USA) were tested. Except for age-appropriate changes, the specimens were free of any osseous defects or deformities based on computed tomography scans (SOMATOM Edge Plus, Siemens Healthcare GmbH, Erlangen, Germany). After thawing, the cadavers were each separated into the vertebral segments Th12-L1, L2-L3 and L4–L5. The specimens were denuded of the surrounding muscle and connective tissue without harming the intersegmental ligamentous structures, facet joints or intervertebral discs. After preparation, the segments were mounted on a testing machine (Fig. 1) with individualized 3D-printed clamps [13].
Description of the stepwise surgical decompression and techniques of the synthetic vertebropexies
Microsurgical decompression with unilateral laminotomy and interspinous synthetic vertebropexy
A unilateral approach was used with sparing laminotomy of the overlying and underlying lamina. Then a flavectomy was performed from cranial to caudal followed by a recessotomy in a standard fashion.
For interspinous fixation, the technique of interspinous vertebropexy was followed [12], with the exception that synthetic material was used in the present biomechanical tests. Both spinous processes were prepared by drilling a 3.2-mm hole from one side to the other through the middle of the spinous process (Fig. 2). A FiberTape cerclage (Arthrex, Naples, Florida) was pulled through the previously drilled holes in a double loop technique (Fig. 2). An extension load of 5 Nm was applied via the static testing machine to simulate a prone position with physiological extension of the lumbar spine. The cerclage was then tightened in a standardized manner with the corresponding tensioner, applying a force of approximately 40 pounds in each case (corresponds to the second marking on the tensioner). This value was chosen arbitrarily. However, the manufacturer recommends a maximum force of 60 pounds for fracture treatment, which we did not want to exceed in order to avoid overtensioning. Afterward, the cerclage was secured with five knots, using the tensioner to tighten the first knot.
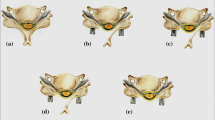
Spinolaminar synthetic vertebropexy
A FiberTape cerclage was first passed through the preexisting hole in the spinous process of the distal vertebra and then passed cranially anterior of the lamina of the proximal. The cerclage was then looped around the lamina and passed again through the hole in the spinous process of the distal vertebra. The same procedure was followed on the opposite side of the vertebra (Fig. 3). The FiberTape cerclage was then tightened as described above and secured with five knots.
Biomechanical experiments
Biomechanical testing of the twelve specimens was performed on a biaxial (linear and torsion) static testing machine (Zwick/ Roell Allroundline 10kN and testXpert III Software, ZwickRoell GmbH & Co. KG, Germany; Fig. 1). The system is based on a traverse: vertical compression and tension can be generated, and torque can be generated in the horizontal plane using a torsion motor. The machine was complemented with a test setup. It consisted of an x–y table and holding arms, allowing specimens to be fixed in horizontal orientation for flexion–extension (FE), lateral shear (LS), lateral bending (LB) and anteroposterior shear (AS), and in vertical orientation for axial rotation (AR). A customized mounting jig was used for the clamped specimens [12]. In each case, the cranial vertebra was loaded while the caudal vertebra was fixed on the x–y table. This allowed translational motion orthogonal to the loading direction, generating pure bending moments and shear forces. The setup allowed specimen fixation with extremely high reproducibility (variability < 0.005°) [11].
Biomechanical testing protocol
Each specimen was tested load-controlled (1) in the native state, after (2) unilateral laminotomy, (3) interspinous vertebropexy and (4) spinolaminar vertebropexy. After each surgical step, the segments were loaded in FE, LS, LB, AS and AR (in the order listed). For each loading case, five preloading cycles were performed before recording the relative motion between the cranial and caudal vertebral bodies in the sixth cycle. Data were recorded throughout the loading cycle, and the amplitude of translational motion of the markers (LS, AS) and projected angulation in the plane of motion (FE, LB, AR) were evaluated.
The segments were initially loaded with ± 10 Nm in the bending planes and ± 200 N in the shear loading. Slightly higher loads than in the physiological range were chosen to test the fixation techniques at extreme loading. Loading was applied at a rate of 1°/sec for flexion–extension and lateral bending, 0.5°/sec for axial rotation, and 0.5 mm/sec for anterior, posterior and lateral shear [13]. During testing, specimens were kept moist by frequent spraying with phosphate-buffered saline.
The following comparisons of segmental ROM were undertaken: (1) microsurgical decompression with unilateral laminotomy versus synthetic vertebropexies, (2) synthetic interspinous versus spinolaminar vertebropexy, (3) ligamentous interspinous vertebropexy versus synthetic interspinous vertebropexy and (4) synthetic vertebropexies versus dorsal fusion. For this purpose, data sets from previously published studies [12] were used.
Data analysis
The statistical evaluation was performed with MATLAB (MATLAB 2020b, MathWorks, Massachusetts, USA). Nonparametric tests were used for statistical analysis because the assumptions of a normal distribution were not always met. The difference in range of motion (ROM) relative to the native condition is reported with the median and interquartile range. The Wilcoxon signed rank test was used for the statistical comparison of matched relative ROM values. Specifically, for the obtained results in each of the five loading directions, the relative ROM after the synthetic vertebropexies was compared with the movement after microsurgical decompression with unilateral laminotomy and a third comparison consisted of the assessment of possible differences between the two synthetic vertebropexies. Unpaired comparisons of the relative ROM after the synthetic vertebropexies and measurements of the same parameter after microsurgical decompression and instrumentation were performed with Wilcoxon rank sum tests. Furthermore, interspinous synthetic vertebropexy was compared with the ROM after interspinous ligamentous vertebropexy. The significance level alpha was set to 0.05 and the p-values were corrected according to Bonferroni to adjust for multiple comparisons.
Results
Effect of synthetic vertebropexies after microsurgical decompression with unilateral laminotomy
Microsurgical decompression increased native ROM in all loading cases (Fig. 4): in FE by 2%, in LS by 5%, in LB by 1%, in AS by 4% and in AR by 2%.
Interspinous fixation significantly reduced ROM after microsurgical decompression in FE by 66% (p = 0.003), in LB by 7% (p = 0.006) and in AR by 9% (p = 0.02). Shear movements (LS and AS) were also reduced, although not significantly: in LS reduction by 24% (p = 0.07), in AS reduction by 3% (p = 0.21).
Spinolaminar fixation significantly reduced ROM after microsurgical decompression in FE by 68% (p = 0.003), in LS by 28% (p = 0.01), in LB by 10% (p = 0.003) and AR by 8% (p = 0.003). AS was also reduced, although not significantly: reduction by 18% (p = 0.06).
Comparison of interspinous and spinolaminar vertebropexy using synthetic material
The effect of the two techniques was comparable (Fig. 4): FE 34.6% versus 32.9%, n.s. (median; relative ROM after interspinous vs. spinolaminar fixation; native = 100%); LS 79.9% versus 75.2%, n.s.; LB 94% versus 91.2%, n.s.; AS 100.8% versus 86%, n.s.; and AR 93.1% versus 93.3%, n.s..
Overall, both techniques decreased vertebral body segment ROM in all loading cases beyond the native state, except for the interspinous fixation technique, which did not affect AS movement.
One specimen showed a gigli saw effect in the interspinous technique after testing, involving the hole in the spinous process of the caudal vertebral body. This is probably the reason for the greater median ROM in AS motion with this technique.
The spinolaminar technique had a higher effect on shear motion compared to interspinous fixation. Overall, both techniques mainly influenced ROM in FE.
Comparison of ligamentous interspinous fixation (ligamentous vertebropexy) and interspinous fixation using a fibercerclage (synthetic vertebropexy)
The effect of the two techniques was comparable and thus largely independent of the material used for stabilization (Fig. 5): FE 34.6% versus 36.8%, n.s. (median; relative ROM after interspinous vs. ligamentous interspinous fixation; native = 100%); LS 79.9% versus 81.7%, n.s.; LB 94% versus 95.9%, n.s.; AS 100.8% versus 96.3%, n.s.; and AR 93.1% versus 93.5%, n.s..
Comparison of synthetic vertebropexies and dorsal fusion
Both synthetic vertebropexies affected all loading cases, but significantly less than fusion by connecting the inserted pedicle screws (Fig. 4). After fusion, all loading cases, except LS (LS 14% vs. 24% (n.s.) vs. 28% (n.s.)), showed significantly higher median relative reductions compared to interspinous and spinolaminar synthetic vertebropexy: FE 83.3% versus 66% (median; relative reduction after fusion vs. interspinous fixation, p = 0.026) versus 68% (relative reduction after fusion vs. spinolaminar fixation, p = 0.04); LB 73.3% versus 7% (p < 0.001) versus 10% (p < 0.001); AS 34.9% versus 3% (p = 0.02) versus 18% (p = 0.02); and AR 49% versus 9% (p = 0.02) versus 8% (p = 0.02).
Discussion
The main findings of the present study are that the two fixation techniques achieved comparable results to ligamentous vertebropexy—they not only restored the native stability of the segment after surgical decompression, but also placed the segment in a more stable state without complete immobilization of the segment. According to the concept of vertebropexy, the greatest effect was obtained with flexion–extension. In addition, some, although not significant, increase in a-p stability was achieved with the spinolaminar technique.
The biomechanical understanding of the human body is of utmost importance in orthopedic surgery and especially in spine surgery. When degeneration occurs, the stability of the disc [14] and ligaments [15] decreases, which can lead to instability of the segment and thus pain [11]. However, iatrogenic interventions such as common decompression and fusion procedures also result in injury to the passive stabilizers of the target segment or adjacent segment, with similar negative consequences. While it is known from previous cadaveric reduction studies that decompression risks destabilizing the segment and further advancing the degenerative cascade [11, 16, 17], instrumentation with pedicle screws restricts segmental mobility to a minimum. The resulting redistribution of loads may lead to adverse mechanical consequences within the spine, which are associated with negative consequences for the patient [18]. Overall, spinal fusion exhibits a high rate of complications [2, 4, 5, 19] with one-third of patients requiring reoperation within 15 years [6]. Nevertheless, posterior spinal fusion (PSF) represents the current gold standard.
Since various alternative stabilization techniques have not reached clinical acceptance in the past, the present study aims to perform basic research on a novel surgical technique—the technique of vertebropexy. Within this frame, this paper presents two semi-rigid fixation techniques, interspinous and spinolaminar synthetic vertebropexy, based on the concept of previously published ligamentous vertebropexy [10] as an alternative to the commonly used dorsal fusion.
As with ligamentous vertebropexy, the technique aims to stabilize primarily flexion–extension and, to some degree, shear motion. All other directions of motion should remain flexible and correspond to the preoperative ROM. Since allografts are not available for the immensely large spine surgery market, are very expensive, and may be rejected by patients, synthetic material was used in this specific work and tested for the first time.
Both synthetic vertebropexy techniques increased segmental stability for all directions of movement compared to prior microsurgical decompression. Considering flexion–extension, the ROM was reduced with both techniques by more than 60% compared to the native segment. This effect was even more pronounced, although not statistically significant, with synthetic interspinous vertebropexy than with ligamentous stabilization. The reason for this is probably the easier tensioning of the cerclage with a tensioning system designed specifically for this purpose. However, the higher stiffness of the construct also plays a role. In this study, commercially available products specifically designed for long-term care were used. In the long term, however, synthetic ligaments developed specifically for vertebropexy that replicate the properties of allografts as closely as possible will be of great importance.
When comparing the two synthetic vertebropexy techniques, the stabilizing effect was almost comparable. Interestingly, however, shear forces were slightly controlled better with the spinolaminar technique: the ROM was reduced in LS by 28% and in AS by 18% (relative values, microsurgical decompression = 100%). Interspinous fixation reduced ROM in LS by 24% in the LS and in AS by 3%. This difference can be explained by the fact that the fixation of the segment with the spinolaminar technique happens not purely in the cranio-caudal direction, but also in the anteroposterior direction (Fig. 3) and can thus absorb forces in this direction.
The synthetic vertebropexies generate stability, not only more "conservatively" than dorsal fusion, but also more targeted: they mainly restrict flexion–extension and, to a lesser extent, lateral shear; the other directions of motion are closely restored to the native state. Fusion resulted in significantly higher median relative reductions in ROM, only in LS the vertebropexies showed greater effects. This should be considered beneficial, as pronounced restrictions are detrimental to force redistribution in the lumbar segment [3].
Clinical implications
Considering the previous attempts of dynamic stabilization in the cervical and lumbar spine has failed and could not achieve sufficient stability despite technical innovations and improvements [20,21,22], the techniques presented here appear encouraging. First, they are reversible, in other words, stabilization can be reversed and the option to convert to the current gold standard, dorsal fusion, remains. Second, application in different indications is possible: for example, interspinous fixation can be added after microsurgical decompression if the surgeon wishes to achieve more stability, such as in existing low-grade spondylolisthesis. When the posterior structures are omitted, such as after midline decompression, the spinolaminar technique can be used. Of note, the proposed fixation techniques are mainly relevant in cases where it is unclear whether spinal decompression alone is the appropriate surgical treatment or whether fusion should be pursued.
Degenerative lumbar spinal stenosis undergoing lumbar decompression alone results in a high reoperation rate (up to 30%) [23]. Previously identified risk factors include facet effusion, disc degeneration and preoperative amount of lumbar back pain [23,24,25]. Fusion, in contrast, is associated with longer postoperative recovery, more surgical-related complications, and greater costs [26], independent of the complications described above. In summary, a good surgical alternative for affected patients is still pending and a middle ground is being sought to neither destabilize nor fix too rigidly. The goal must be at least the restoration of native stability.
Limitations
This biomechanical study inherits some limitations. First, force-driven pure moments allow precise comparisons between different surgical steps, but represent very gross simplifications of the complex motion and force patterns of the human spine in vivo. It is unclear to what extent the effects shown will persist over the long term in a mobile individual. However, the experimental setup used here can be considered as close as possible to simulating reality ex vivo. Second, the ROM reported here most likely corresponds to the postoperative baseline condition. Over time, the formation of scar tissue is to be expected, and further changes must be anticipated due to the progression of the degenerative process. However, we believe that scarring will enhance the effect of vertebropexy. In addition, material fatigue may reduce the stabilizing effect. The extent to which this could be clinically relevant can only be determined in clinical trials. Third, when synthetic material such as the fibercerclage is used, no relevant loss of tension due to creep must be expected; however, the operating surgeon should be aware of a possible gigli saw effect in osteoporotic bone. In the present study, this was observed in one specimen. To avoid this complication, the material used can be guided around the spinous process, if the bone quality is known to be poor, thus eliminating the need for drilling holes in the spinous process. This adapted technique was also tested on a trial basis and resulted in similar reductions in ROM.
Conclusion
Synthetic vertebropexy is able to reduce lumbar segmental motion, especially in flexion–extension. The spinolaminar technique affects shear forces to a greater extent than the interspinous technique.
References
Reisener M-J, Pumberger M, Shue J et al (2020) Trends in lumbar spinal fusion—a literature review. J Spine Surg 6:752–761. https://doi.org/10.21037/jss-20-492
Park P, Garton HJ, Gala VC et al (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine 29:1938–1944. https://doi.org/10.1097/01.brs.0000137069.88904.03
Chen Z, Zhao J, Xu H et al (2008) Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J 17:1476–1480. https://doi.org/10.1007/s00586-008-0776-9
Marie-Hardy L, Pascal-Moussellard H, Barnaba A et al (2020) Screw loosening in posterior spine fusion: prevalence and risk factors. Global Spine J 10:598–602. https://doi.org/10.1177/2192568219864341
Chrastil J, Patel AA (2012) Complications associated with posterior and transforaminal lumbar interbody fusion. J Am Acad Orthop Sur 20:283–291. https://doi.org/10.5435/jaaos-20-05-283
Maruenda JI, Barrios C, Garibo F, Maruenda B (2016) Adjacent segment degeneration and revision surgery after circumferential lumbar fusion: outcomes throughout 15 years of follow-up. Eur Spine J 25:1550–1557. https://doi.org/10.1007/s00586-016-4469-5
Regan JJ (2005) Clinical results of charité lumbar total disc replacement. Orthop Clin N Am 36:323–340. https://doi.org/10.1016/j.ocl.2005.03.005
Wiseman CM, Lindsey DP, Fredrick AD, Yerby SA (2005) The effect of an interspinous process implant on facet loading during extension. Spine 30:903–907. https://doi.org/10.1097/01.brs.0000158876.51771.f8
Lafage V, Gangnet N, Sénégas J et al (2007) New interspinous implant evaluation using an in vitro biomechanical study combined with a finite-element analysis. Spine 32:1706–1713. https://doi.org/10.1097/brs.0b013e3180b9f429
Farshad M, Tsagkaris C, Widmer J et al (2023) Vertebropexy as a semi-rigid ligamentous alternative to lumbar spinal fusion. Eur Spine J. https://doi.org/10.1007/s00586-023-07647-y
Widmer J, Cornaz F, Scheibler G et al (2020) Biomechanical contribution of spinal structures to stability of the lumbar spine—novel biomechanical insights. Spine J 20:1705–1716. https://doi.org/10.1016/j.spinee.2020.05.541
Farshad M, Burkhard MD, Spirig JM (2021) Occipitopexy as a fusionless solution for dropped head syndrome: a case report. JBJS Case Connect. https://doi.org/10.2106/jbjs.cc.21.00049
Cornaz F, Fasser M-R, Spirig JM et al (2019) 3D printed clamps improve spine specimen fixation in biomechanical testing. J Biomech 98:109467. https://doi.org/10.1016/j.jbiomech.2019.109467
Cornaz F, Widmer J, Farshad-Amacker NA et al (2020) Biomechanical contributions of spinal structures with different degrees of disc degeneration. Spine 46:E869–E877. https://doi.org/10.1097/brs.0000000000003883
Cornaz F, Widmer J, Farshad-Amacker NA et al (2021) Intervertebral disc degeneration relates to biomechanical changes of spinal ligaments. Spine J 21:1399–1407. https://doi.org/10.1016/j.spinee.2021.04.016
Grunert P, Reyes PM, Newcomb AGUS et al (2016) Biomechanical evaluation of lumbar decompression adjacent to instrumented segments. Neurosurgery 79:895–904. https://doi.org/10.1227/neu.0000000000001419
Smith ZA, Vastardis GA, Carandang G et al (2014) Biomechanical effects of a unilateral approach to minimally invasive lumbar decompression. Plos One 9:e92611. https://doi.org/10.1371/journal.pone.0092611
Borgeaud T, Huec J-CL, Faundez A (2022) Pelvic and spinal postural changes between standing-sitting positions following lumbosacral fusion: a pilot study. Int Orthop. https://doi.org/10.1007/s00264-022-05365-6
Kim HJ, Iyer S (2016) Proximal junctional kyphosis. J Am Acad Orthop Sur 24:318–326. https://doi.org/10.5435/jaaos-d-14-00393
Jung J-M, Hyun S-J, Kim K-J, Jahng T-A (2021) Dynamic stabilization surgery in patients with spinal stenosis: long-term outcomes and the future. Spine 46:E893–E900. https://doi.org/10.1097/brs.0000000000004049
Brooks AL, Jenkins EB (1978) Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am 60:279–284. https://doi.org/10.2106/00004623-197860030-00001
Dickman CA, Sonntag VK, Papadopoulos SM, Hadley MN (1991) The interspinous method of posterior atlantoaxial arthrodesis. J Neurosurg 74:190–198. https://doi.org/10.3171/jns.1991.74.2.0190
Hwang H-J, Park H-K, Lee G-S et al (2016) Predictors of reoperation after microdecompression in lumbar spinal stenosis. Korean J Spine 13:183–189. https://doi.org/10.14245/kjs.2016.13.4.183
Chaput C, Padon D, Rush J et al (2007) The significance of increased fluid signal on magnetic resonance imaging in lumbar facets in relationship to degenerative spondylolisthesis. Spine 32:1883–1887. https://doi.org/10.1097/brs.0b013e318113271a
Kleinstück FS, Grob D, Lattig F et al (2009) The influence of preoperative back pain on the outcome of lumbar decompression surgery. Spine 34:1198–1203. https://doi.org/10.1097/brs.0b013e31819fcf35
Machado GC, Ferreira PH, Harris IA et al (2015) Effectiveness of surgery for lumbar spinal stenosis: a systematic review and meta-analysis. Plos One 10:e0122800. https://doi.org/10.1371/journal.pone.0122800
Acknowledgements
Imaging was performed with support of the Swiss Center for Musculoskeletal Imaging, SCMI, Balgrist Campus AG, Zurich.
Funding
Open access funding provided by University of Zurich. The authors, their immediate families and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Contributions
AKC contributed to design of the study, results interpretation, manuscript writing and editing; AF contributed to data collection; JW contributed to results interpretation and manuscript editing; MRF contributed to data analysis and manuscript editing; MF contributed to conception and manuscript editing.
Corresponding author
Ethics declarations
Competing interests
The last author (MF) reports being a Consultant for Incremed (Balgrist University Hospital Startup), Zimmer Biomet, Medacta, and 25 Segments (Balgrist University Hospital Startup). All the other authors report no conflicts of interest.
Ethics approval
Kantonale Ethikkommission Zürich had given the approval for the study. (Basec No. KEK-ZH-Nr. 2022–00715).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Calek, AK., Altorfer, F., Fasser, MR. et al. Interspinous and spinolaminar synthetic vertebropexy of the lumbar spine. Eur Spine J 32, 3183–3191 (2023). https://doi.org/10.1007/s00586-023-07798-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07798-y