Abstract
Purpose
To develop ligamentous vertebral stabilization techniques (“vertebropexy”) that can be used after microsurgical decompression (intact posterior structures) and midline decompression (removed posterior structures) and to elaborate their biomechanical characteristics.
Methods
Fifteen spinal segments were biomechanically tested in a stepwise surgical decompression and ligamentous stabilization study. Stabilization was achieved with a gracilis or semitendinosus tendon allograft, which was attached to the spinous process (interspinous vertebropexy) or the laminae (interlaminar vertebropexy) in form of a loop. The specimens were tested (1) in the native state, after (2) microsurgical decompression, (3) interspinous vertebropexy, (4) midline decompression, and (5) interlaminar vertebropexy. In the intact state and after every surgical step, the segments were loaded in flexion–extension (FE), lateral shear (LS), lateral bending (LB), anterior shear (AS) and axial rotation (AR).
Results
Interspinous vertebropexy significantly reduced the range of motion (ROM) in all loading scenarios compared to microsurgical decompression: in FE by 70% (p < 0.001), in LS by 22% (p < 0.001), in LB by 8% (p < 0.001) in AS by 12% (p < 0.01) and in AR by 9% (p < 0.001). Interlaminar vertebropexy decreased ROM compared to midline decompression by 70% (p < 0.001) in FE, 18% (p < 0.001) in LS, 11% (p < 0.01) in LB, 7% (p < 0.01) in AS, and 4% (p < 0.01) in AR. Vertebral segment ROM was significantly smaller with the interspinous vertebropexy compared to the interlaminar vertebropexy for all loading scenarios except FE. Both techniques were able to reduce vertebral body segment ROM in FE, LS and LB beyond the native state.
Conclusion
Vertebropexy is a new concept of semi-rigid spinal stabilization based on ligamentous reinforcement of the spinal segment. It is able to reduce motion, especially in flexion–extension. Studies are needed to evaluate its clinical application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal fusion has become a very common surgical procedure, among others in the treatment of degenerative disorders of the spine. The indications for this surgical procedure are diverse and include low-back pain due to facet joint osteoarthritis, degenerative spondylolisthesis, degenerative scoliosis and segmental instability. The latter can also be a result of iatrogenic destabilization following surgical resection of ligamentous structures as well as the facet joint. However, spinal fusion is associated with serious long-term complications, such as adjacent segment degeneration (ASD), screw loosening, pseudoarthrosis, implant failure, and, in rare cases, neurovascular injury during implant insertion [1,2,3,4,5]. The redistribution of loads with subsequently increased biomechanical stress are believed to act as accelerators of ASD [1, 2, 6] and proximal junctional kyphosis [7]. Further, long fusions can lead to a relevant, irreversible loss of motion, which can cause postural changes [8].
Although these challenges are well-known, alternative techniques of spinal stabilizations have not yet yielded satisfactory results with broad clinical impact. Semi-rigid fixation techniques have been proposed to overcome the above-mentioned challenges, but resulted in new complications at the implant–bone interface, such as device breakage, dislocation or screw loosening [9,10,11].
A promising concept that utilizes the orthopedic principles of ligament reinforcement for joint stabilization has already been successfully applied to the treatment of dropped head syndrome, resulting in a fusion-free stabilization of the head [12]. Therefore, we inquired if such ligamentous fixation of the vertebra, would be feasible in the lumbar spine. Further, we aimed to elaborate on the biomechanical characteristics of two ligamentous vertebral stabilization techniques usable after microsurgical decompression (intact posterior structures) and midline decompression (removed posterior structures).
Materials and methods
Dissection, preparation and storage
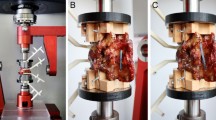
The study was approved by the responsible investigational review board. Fifteen spinal segments (TH12/L1: 3, L1/2: 3, L2/3: 3, L3/4: 3, L4/5: 3) originating from seven fresh frozen cadavers (Table 1; Science Care, Phoenix, AZ, USA) were tested. After thawing, CT scans (SOMATOM Edge Plus, Siemens Healthcare GmbH, Erlangen, Germany) were performed to exclude bony defects. The specimens were carefully dissected without harming bony processes, paraspinal ligaments or the intervertebral discs. After preparation, the segments were mounted on a testing machine (Fig. 4a) using custom 3D-printed-clamps [13].
Description of the stepwise surgical decompression and techniques of vertebropexy
Microsurgical decompression and interspinous vertebropexy
A bilateral approach was used with sparing laminotomy of the overlying and underlying lamina. Then a flavectomy was performed from cranial to caudal followed by a standard recessotomy.
Both spinous processes were prepared for allograft passage by predrilling a 3.2-mm hole from one side to the other through the middle of the spinous process. The holes were overdrilled using a 5-mm drill bit, taking care not to create an iatrogenic fracture (Fig. 1). A gracilis or semitendinosus tendon allograft (AlloSource, Centennial, Colorado) was prepared, thinning the allograft to a maximum diameter of 4 mm and reinforcing one end of the tendon with a Fiberwire No. 2 (Arthrex, Naples, Florida) using a 2-cm-long Krackow suture [14] (Fig. 1). For vertebropexy, the tendon graft was looped twice. The other end of the tendon was similarly reinforced with a Fiberwire No. 2, creating a loop in addition to the Krackow suture (Fig. 1). Thereafter, the allograft was pulled through the previously drilled holes in a double loop technique (Fig. 2a–c). An extension load of 5Nm was applied via the static testing machine to simulate a prone position with physiological extension of the lumbar spine. The Fiberwire was knotted using the cow hitch technique (Fig. 2d): a double-stranded knot configuration with a loop on one side, secured by four half hitches. This technique is biomechanically stronger and stiffer compared to several other conventional knots [15]. The knot was tightened with a force of 70N using a needle holder (Fig. 2e). The applied force was objectified with a force gauge. Finally, the second end of the tendon was sutured to the loop (Figs. 2f, and 4b).
The same surgical approach is used for both steps (decompression and fixation) so no additional muscle attachments need to be released for fixation of the vertebral segment.
Midline decompression and interlaminar vertebropexy
The supraspinous and interspinous ligaments were sharply removed with a Leksell rongeur, and the two spinous processes were partially removed. Midline decompression was performed with the osteotome, taking care not to harm the facet joints. The remaining ligamentum flavum was exposed and removed from cranial to caudal.
Two tendon allografts were reinforced in the same manner as described above (Fig. 1). Then the reinforced ends of the tendons were carefully passed under the laminae on both sides from cranial to caudal (Fig. 3a). A rongeur was used to pull the tips of both tendons up through the distal interlaminar window or above the inferior lamina (Fig. 3b). The segment was reloaded with 5Nm extension and the Fiberwire was knotted bilaterally using a cow hitch and tightened with a force of 70N (Fig. 3c). The remaining part of the tendon was sutured to the loop (Fig. 3D, Fig. 4c).
The two ligamentous stabilization techniques are used for different indications. Additional soft tissue disruption can therefore be avoided as the same approach is used for decompression.
Biomechanical experiments
Biomechanical testing of the 15 specimens was performed on a biaxial (linear & torsion) static testing machine (Zwick/ Roell Allroundline 10kN and testXpert III Software, ZwickRoell GmbH & Co. KG, Germany; Fig. 1a). The system is based on a traverse to generate vertical compression and tension and a torsion motor to generate torque in the horizontal plane. The machine was complemented with a testing setup consisting of an x–y-table and holding arms that allow for specimen fixation in a horizontal orientation for flexion–extension (FE), lateral shear (LS), lateral bending (LB), and anteroposterior shear (AS), and in a vertical orientation for axial rotation (AR). A customized mounting apparatus for the clamped specimens was used [13], consisting of high-precision fitting rings, pins, and a mechanism to compress the connection with a defined load before tightening. Loading was applied to the cranial vertebra while the caudal vertebra was fixed to the x–y-table allowing for translational movement orthogonal to the loading direction. Coupled motions around the x- and y-axis were prevented, restricting all motions to the test plane. With this configuration, translation forces, as might occur with a fully constrained setup, are eliminated, resulting in pure moments and pure forces in the plane of interest. Further details on the test setup, including images of all loading configurations, are provided in a previously published study [16].
Biomechanical testing protocol
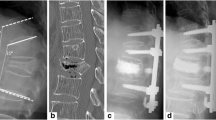
Each specimen was tested load-controlled (1) in the native state, after (2) microsurgical decompression, (3) interspinous vertebropexy, (4) midline decompression and (5) interlaminar vertebropexy. The surgical steps are illustrated in Fig. 5. After every surgical step, the segments were loaded in FE, LS, LB, AS and AR (in the listed order). For each loading case, five preloading cycles were conducted before the relative motion between the cranial and caudal vertebral bodies was recorded in the sixth cycle.
The segments were initially loaded with ± 10 Nm in the bending planes and ± 200 N in shear loading. In order to test the fixation techniques on extreme loads, slightly higher loads were chosen than the physiological range. Loading was applied with a velocity of 1°/s in flexion–extension and lateral bending, 0.5°/s in axial rotation, and 0.5 mm/s in anterior, posterior and lateral shear [17]. During testing, specimens were kept moist by frequently spraying them with phosphate buffered saline.
Data analysis
The 3D motion data of the vertebrae (Atracsys Fusion Track 500, recording frequency 10 Hz, tracking accuracy 0.09 mm [RMS]) were used to correct the load–deflection curves of the testing machine. The centerline of the load–deflection hysteresis was fitted using a fifth-order polynomial. A standardized method [16] was used to separate positive/negative load directions in the load–deflection curves. For symmetrical load directions (LB, AR, and LS), the average values between negative and positive load (left, right) were used. Torsional preload in the sagittal plane was determined by analyzing the moment change in the neutral position between flexion and extension after each surgical step.
The statistical evaluation was performed with MATLAB (Matlab 2020b, MathWorks, Massachusetts, USA). The difference in range of motion (ROM) relative to the native condition is reported with median and interquartile range. The Wilcoxon signed rank test was used for the statistical comparison of matched relative ROM values. Specifically, for the obtained results in each of the five loading directions, the ROM after the vertebropexies was compared with the movement after the respective previous decompression steps and a third comparison consists of the assessment of possible differences between the two vertebropexy steps. The mean values were used for segment-wise analysis, as only three data points were available per spinal level. Due to multiple comparisons, the significance level α was adjusted with Bonferroni corrections and set to be 0.05/2 = 0.025.
Results
The absolute ROM of the native segment and the segment after microsurgical decompression, interspinous vertebropexy, midline decompression, and interlaminar vertebropexy is shown in Table 2 according to loading case.
Interspinous vertebropexy
Interspinous vertebropexy significantly reduced the ROM in all loading scenarios (Online Resource 1). The ligamentous stabilization technique was able to decrease the ROM after microsurgical decompression in FE by almost 70% (p < 0.001), in LS by 22% (p < 0.001), in LB by 8% (p < 0.001), in AS by 12% (p < 0.01), and in AR by 9% (p < 0.001). The effect of interspinous vertebropexy based on segments (Table 2) was relatively constant, and independent of the segment.
Interlaminar vertebropexy
Interlaminar vertebropexy significantly decreased the ROM of all segments compared to midline decompression in all loading scenarios. ROM was decreased by 70% (p < 0.001) in FE, 18% (p < 0.001) in LS, 11% (p < 0.01) in LB, 7% (p < 0.01) in AS, and 4% (p < 0.01) in AR. The ROM was comparable between the segments.
Comparison of the two vertebropexy techniques
Vertebral segment ROM was significantly smaller with the interspinous vertebropexy compared to the interlaminar vertebropexy for all loading scenarios except FE. In FE, the effect of the two techniques was comparable (36.7 vs. 43.1%, p = 0.08 (median; relative ROM after stabilization; native = 100%). Significantly smaller vertebral segment ROM was achieved using interspinous vertebropexy in LS (81.7 vs. 98.1%; p < 0.01), LB (95.9 vs. 100.3%; p < 0.001), AS (96.3 vs. 115.9%; p < 0.001), and AR (93.5 vs. 115.5%; p < 0.001).
Overall, both techniques decreased vertebral body segment ROM in FE, LS and LB beyond the native state.
The vertebropexy mainly reduced ROM in FE, in the other loading cases the effect was considerably smaller. The decompression steps led to increased ROM in each loading scenario compared to the native state.
Discussion
By applying the concept of ligamentous stabilization of joints to the spine, a novel technique of segmental stabilization, namely “vertebropexy” is described and its biomechanical performance in cadaveric specimens is reported. Vertebropexy not only restored the native segmental stability after decompression, but transferred the segment to a semi-rigid state, a finding which was most pronounced in flexion–extension.
Depending on the integrity of the dorsal structures after decompression two surgical techniques were developed: (1) interspinous vertebropexy following posterior microsurgical decompression with preservation of midline structures and (2) interlaminar vertebropexy following posterior decompression without preservation of midline structures. These structures mostly provide passive stability in flexion [16]. With both vertebropexy techniques segmental stability could be increased for all directions of movement compared to prior decompression. Considering flexion–extension, vertebropexy reduced the ROM by more than 50% compared to the native segment.
When comparing the two vertebropexy techniques, the stabilizing effect of the interspinous technique was more pronounced. This can be explained by the smaller lever arm of the interlaminar technique compared to the interspinous technique, as the distance to the center of rotation, i.e., to the center of the disc, is smaller. A force of 70N for tightening the knot was arbitrarily chosen to not exceed the load to failure [18], to minimize the risk of iatrogenic fracture, and to use a force that could be easily achieved in the operating room.
Spinal fusion is currently used to treat various spinal pathologies and has an overall high complication rate [1,2,3,4,5,6,7] with one-third of patients requiring reoperation within 15 years [19]. Most of the long-term complications are believed to be consequences of a relevant change of biomechanical loads due to the increased stiffness of the fused segments [1, 2, 6, 8]. However, due to unsatisfying alternatives, spinal fusion is still considered the gold standard for surgical treatment of several spinal conditions. To counter the disadvantages of spinal fusion, an alternative method was developed that would increase spinal stability without completely immobilizing the vertebral segment. Previous concepts pursuing the same goal failed: spinous process implants, were initially followed with growing interest. However, in recent years, some studies have shown higher rates of reoperation with low cost-effectiveness, so they are hardly in use anymore [9, 11]. The same applies to cervical wiring techniques: sublaminar wires for atlantoaxial fusion were first described by Galli in 1939 [20] and have been further developed over the years [21, 22]. However, despite improvements and innovations, no technique has gained acceptance due to insufficient stability. Therefore, we aimed for a novel method that avoids any foreign material, generates stability, and is reversible, with the option of conversion to the current gold standard, dorsal fusion. With these requirements in mind, we have transferred the orthopedic concept of ligamentous stabilization of joints to the spine. A comparable ligamentous stabilization has already been successfully performed in a case report on the cervical spine to treat dropped head syndrome [12]. In the present study, this idea was transferred to the lumbar spine. A first attempt at ligament stabilization, called "syndesmoplasty," for unilateral degenerative spondylolisthesis was performed as early as 1999 [23]. The latter follows a related non-rigid stabilization technique using an artificial ligament whose free ends are inserted into the vertebral body through a hole in the pedicle, crossed within the vertebral body, and exit the vertebral body via the contralateral pedicle. For lower grade spondylolisthesis (Meyerding grade 1 and 2) good clinical and radiological results were reported. The authors concluded the technique as a valuable alternative in treatment of degenerative spondylolisthesis compared to rigid fusion.
The biomechanical characteristics of both vertebropexy techniques seem promising. Furthermore, vertebropexy might have other advantages compared to spinal fusion: it is fully reversible, the use of biologic tissue eliminates the need for foreign bodies (e.g., metal implants), fusion can still be performed secondarily if ineffective, segment stability is increased while avoiding complete fusion, and preventing postural deformity.
Limitations
This study is a proof-of-concept study. Although allograft implantation itself is a long-established method, it has not yet been studied in the application of vertebropexy. The data demonstrate reduced ROM in the vertebropexy groups. However, to what extent this stability remains in a mobile person with more supple constructs and human movements cannot be answered. Thus, the next step will be to demonstrate clinical applicability.
Long-term maintenance of stability is also a factor that is not easily answered. Certainly, some tension is lost by slight creep of the allograft. However, it is known from anterior cruciate ligament reconstruction that this occurs in the first few minutes and under load [24], implying that our study has already quantified the relaxed state. In the long term, biological effects, such as tendon degradation, could also play a role in biomechanical stability.
In addition, there are other biomechanical factors whose effects on the patient are difficult to assess. For example, vertebropexy is certainly associated with a shift in the center of rotation since fixation is posterior. Also, a possible giggli saw effect of the tendon in osteoporotic bone, which did not occur in our study but could be conceivable, could be a potential issue. A disadvantage of the interlaminar technique is the inevitable weakening of the ligamentum flavum, by creating a small passage for the tendon allograft, of the overlying and underlying segment.
Conclusion
Vertebropexy is a new concept of semi-rigid spinal stabilization based on ligamentous reinforcement of the spinal segment. It is able to reduce motion, especially in flexion–extension. Studies are needed to evaluate its clinical application.
Availability of data and material
None.
References
Park P, Garton HJ, Gala VC et al (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine 29:1938–1944. https://doi.org/10.1097/01.brs.0000137069.88904.03
Chen Z, Zhao J, Xu H et al (2008) Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J 17:1476–1480. https://doi.org/10.1007/s00586-008-0776-9
Marie-Hardy L, Pascal-Moussellard H, Barnaba A et al (2020) Screw loosening in posterior spine fusion: prevalence and risk factors. Global Spine J 10:598–602. https://doi.org/10.1177/2192568219864341
Ondra SL, Marzouk S (2003) Revision strategies for lumbar pseudarthrosis. Neurosurg Focus 15:1–5. https://doi.org/10.3171/foc.2003.15.3.9
Chrastil J, Patel AA (2012) Complications associated with posterior and transforaminal lumbar interbody fusion. J Am Acad Orthop Sur 20:283–291. https://doi.org/10.5435/jaaos-20-05-283
Guan Y, Yoganandan N, Maiman DJ, Pintar FA (2008) Internal and external responses of anterior lumbar/lumbosacral fusion: nonlinear finite element analysis. J Spinal Disord Tech 21:299–304. https://doi.org/10.1097/bsd.0b013e31812e6276
Kim HJ, Iyer S (2016) Proximal junctional kyphosis. J Am Acad Orthop Sur 24:318–326. https://doi.org/10.5435/jaaos-d-14-00393
Borgeaud T, Huec J-CL, Faundez A (2022) Pelvic and spinal postural changes between standing-sitting positions following lumbosacral fusion: a pilot study. Int Orthop, pp 1–8. https://doi.org/10.1007/s00264-022-05365-6
Jung J-M, Hyun S-J, Kim K-J, Jahng T-A (2021) Dynamic stabilization surgery in patients with spinal stenosis: long-term outcomes and the future. Spine 46:E893–E900. https://doi.org/10.1097/brs.0000000000004049
Prud’homme M, Barrios C, Rouch P et al (2015) Clinical outcomes and complications after pedicle-anchored dynamic or hybrid lumbar spine stabilization. J Spinal Disord Techniques 28:E439–E448. https://doi.org/10.1097/bsd.0000000000000092
Cecchinato R, Bourghli A, Obeid I (2020) Revision surgery of spinal dynamic implants: a literature review and algorithm proposal. Eur Spine J 29:57–65. https://doi.org/10.1007/s00586-019-06282-w
Farshad M, Burkhard MD, Spirig JM (2021) Occipitopexy as a fusionless solution for dropped head syndrome: a case report. JBJS Case Connect 11. https://doi.org/10.2106/jbjs.cc.21.00049
Cornaz F, Fasser M-R, Spirig JM et al (2019) 3D printed clamps improve spine specimen fixation in biomechanical testing. J Biomech 98:109467. https://doi.org/10.1016/j.jbiomech.2019.109467
Krackow KA, Cohn BT (1987) A new technique for passing tendon through bone. Brief note. J Bone Joint Surg Am 69:922–924
Meyer DC, Bachmann E, Lädermann A et al (2018) The best knot and suture configurations for high-strength suture material. An in vitro biomechanical study. Orthop Traumatol Surg Res 104:1277–1282. https://doi.org/10.1016/j.otsr.2018.08.010
Widmer J, Cornaz F, Scheibler G et al (2020) Biomechanical contribution of spinal structures to stability of the lumbar spine—novel biomechanical insights. Spine J 20:1705–1716. https://doi.org/10.1016/j.spinee.2020.05.541
Wilke H-J, Wenger K, Claes L (1998) Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J 7:148–154. https://doi.org/10.1007/s005860050045
Kim KH, Long MK, McCormack R, Ruotolo C (2018) Use of a safety clamp when performing arthroscopic knot tying preserves the suture when it is placed under excessive tension. Orthopedics 42:1–4. https://doi.org/10.3928/01477447-20181023-06
Maruenda JI, Barrios C, Garibo F, Maruenda B (2016) Adjacent segment degeneration and revision surgery after circumferential lumbar fusion: outcomes throughout 15 years of follow-up. Eur Spine J 25:1550–1557. https://doi.org/10.1007/s00586-016-4469-5
Gallie WE (1939) Fractures and dislocations of the cervical spine. Am J Surg 46:495–499. https://doi.org/10.1016/s0002-9610(39)90309-0
Brooks AL, Jenkins EB (1978) Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg 60:279–284. https://doi.org/10.2106/00004623-197860030-00001
Dickman CA, Sonntag VK, Papadopoulos SM, Hadley MN (1991) The interspinous method of posterior atlantoaxial arthrodesis. J Neurosurg 74:190–198. https://doi.org/10.3171/jns.1991.74.2.0190
Mochida J, Suzuki K, Chiba M (1999) How to stabilize a single level lesion of degenerative lumbar spondylolisthesis. Clin Orthop Relat Res 368:126–134. https://doi.org/10.1097/00003086-199911000-00015
Cruz AI, Fabricant PD, Seeley MA et al (2016) Change in size of Hamstring grafts during preparation for ACL reconstruction. J Bone Joint Surg 98:484–489. https://doi.org/10.2106/jbjs.15.00802
Acknowledgements
The authors would like to thank Dr. Christoph Zindel for his support. Imaging was performed with support of the Swiss Center for Musculoskeletal Imaging, SCMI, Balgrist Campus AG, Zurich.
Funding
Open access funding provided by University of Zurich. The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Contributions
MF: conception, manuscript editing; CT: data collection; JW: results interpretation and manuscript editing; MRF: data analysis and manuscript editing; FC: data collection and manuscript editing; AKC: design of the study, results interpretation, manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
The first author (MF) reports being a Consultant for Incremed (Balgrist University Startup), Zimmer Biomet, Medacta, and 25 Segments (Balgrist Startup). All the other authors report no conflicts of interest.
Ethics approval
Kantonale Ethikkommission Zürich had given the approval for the study. (Basec No. KEK-ZH-Nr. 2022-00104).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farshad, M., Tsagkaris, C., Widmer, J. et al. Vertebropexy as a semi-rigid ligamentous alternative to lumbar spinal fusion. Eur Spine J 32, 1695–1703 (2023). https://doi.org/10.1007/s00586-023-07647-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07647-y