Abstract
Purpose
Over the last years, the number of vertebral arthrodesis has been steadily increasing. The use of iliac crest bone autograft remains the “gold standard” for bone graft substitute in these procedures. However, this solution has some side effects, such as the problem of donor site morbidity indicating that there is a real need for adequate alternatives. This pilot study aimed to evaluate the usefulness of chitosan (Ch) porous 3D scaffolds incorporated with resolvin D1 (RvD1) as an alternative implant to iliac bone autograft.
Methods
We have performed bilateral posterolateral lumbar vertebral arthrodesis in a rat animal model. Three experimental groups were used: (i) non-operated animals; (ii) animals implanted with Ch scaffolds incorporated with RvD1 and (iii) animals implanted with iliac bone autograft.
Results
The collagenous fibrous capsule formed around the Ch scaffolds with RvD1 is less dense when compared with the iliac bone autograft, suggesting an important anti-inflammatory effect of RvD1. Additionally, new bone formation was observed in the Ch scaffolds with RvD1.
Conclusion
These results demonstrate the potential of these scaffolds for bone tissue repair applications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal arthrodesis is a surgical procedure that leads to the fusion of two or more vertebrae usually placing a bone graft as a bridge. When conservative treatments fail, this procedure is used in patients suffering from low back pain or sciatica. Spinal arthrodesis is useful in several spine disorders comprising genetic, degenerative, and traumatic conditions and numbers for this surgical intervention are increasing every year. Consequently, demand for technical improvements—such as developing new biomaterials to be used as grafts—is also growing [1].
Autologous bone grafting from the iliac crest is still considered the gold-standard procedure. However, major donor site complications ranging from 2.4 to 6.2%; postoperative pain at the harvested site reported in 6 to 39% of cases; and prolonged surgeries that cause increased risks of bleeding and infection justify the search for new solutions [2, 3]. Additionally, population aging reduces the possibility of using autologous bone grafts [4]. Another widely used option is the combination of bone morphogenetic protein 2 (BMP-2) with biomaterials, however the use of BMPs causes significant inflammatory responses and may lead to either excessive or ectopic bone formation [5]. Therefore, surgeons need more sophisticated and innovative solutions, including, for example, regenerative biomaterials [6].
A biomaterial for bone tissue regeneration should support tissue repair at the defect area and eventually degrade and be replaced by new bone. Several types of biomaterials have been studied for bone repair applications. These include demineralized bone matrix, ceramic materials, metallic materials, natural or synthetic polymeric materials and composites, among others. Polymeric scaffolds are widely used since they can act as carriers of cells and molecules of interest that can actively contribute to the process of bone tissue repair and regeneration [7].
We have developed a new immunomodulatory biomaterial, 3D porous chitosan (Ch) scaffolds with resolvin D1 (RvD1) [8] that may be adequate for bone regeneration. Chitosan is a polymer of natural origin that has a chemical composition constituted by b (1–4) linked D-glucosamine residues with N-acetyl-glucosamine side chains. Chitosan is under study for several different biomedical applications, such as for bone tissue engineering studies [9]. Resolvins belong to a class of endogenous anti-inflammatory molecules, the specialized pro-resolution mediators (SPMs). Resolvins actively induce the resolution of the inflammatory response by preventing neutrophil infiltration, promoting apoptotic neutrophils phagocytosis, inducing clearance of inflammatory microenvironments, and ultimately promoting tissue repair [10]. This immunomodulatory biomaterial was able to induce in vivo macrophage polarization towards an M2 phenotype in an inflammatory air-pouch model, decrease pro-inflammatory cytokines and decrease fibrous capsule thickness around the implanted scaffolds [8]. When tested in rat femoral critical size defect model, it resulted in bone healing improvement [11]. The normal course of healing requires an inflammatory phase followed by a natural resolution of inflammation. This is achieved with this immunomodulatory biomaterial since the 3D chitosan scaffold will induce an inflammatory response with the presence of M1 macrophages and afterwards RvD1 will cause a shift in the macrophage profile towards a M2 reparative phenotype.
In this pilot study, we have explored the behavior of the immunomodulatory Ch scaffolds with RvD1 and compared it to an iliac bone autologous graft in lumbar spine arthrodesis.
Materials and methods
Production of 3D chitosan (Ch) scaffolds with resolvin D1 (RvD1)
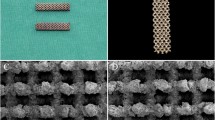
Chitosan from squid pen (Mahtani Chitosan Pvt. Ltd) was purified and produced with 15% of degree of acetylation (DA) as described elsewhere [12]. Concisely, 3D porous scaffolds were produced from degassed 2% w/v Ch solutions in 0.2 M acetic acid via thermally induced phase separation (− 20°) with ensuing sublimation of the ice crystals. After l freeze drying (− 80°C; 0.2 mbar; 24 h), the obtained 3D Ch scaffolds were cut with the shape of a cylinder having a diameter of 4 mm and a thickness of 2 mm. The 3D Ch scaffolds were sterilized immersed in ethanol under vacuum using an ethanol series: 70% (v/v) during 30 min, 50% (v/v) and 25% (v/v) ethanol during 10 min. Subsequently, the scaffolds were washed using ultrapure (Milli Q) water for 10 min. To incorporate the RvD1, we have followed a previously developed procedure [8]. In summarizing, a solution of RvD1 (Cayman Chemical, Ann Arbor, Michigan 48108 USA) was prepared in a concentration of 3.33 ng/μl, and a volume of 30 μl was incorporated in the scaffolds drop-wise with a micropipette. After, the scaffolds were submitted to an additional freeze drying step (− 80°C; 0.2 mbar; 24 h).
Animal model
We have submitted female Sprague Dawley rats (Charles River Laboratories Spain), of 8 weeks of age, to bilateral posterolateral lumbar vertebral arthrodesis at the level of L4 and L5. Anesthesia was performed by isoflurane inhalation. The dorsal area was shaved, washed, and disinfected. The target area was identified by reference to the iliac crest. A midline skin incision was performed, followed by two paramedian fascial incisions and structure-preserving anatomical dissection. The laminae and posterolateral face of the vertebral bodies were exposed and a motorized drill piece was utilized to decorticate the L4 and L5 laminae. Subsequently, either harvested autologous bone or synthetic implant (according to specific group protocol) were placed on the decorticated laminae, bridging the interlaminar space. Finally, closure in layers with skin suturing 4-0 nylon thread was done. Animal care and analgesia were provided post-surgery. In this pilot study, we included three animals in each group: (i) Non-operated animals; (ii) Animals implanted with 3D Ch scaffolds with RvD1 and (iii) Animals with an implanted iliac bone autograft harvested in the same procedure. For autologous bone graft harvest, two separate fascial incisions were performed and approximately 0.2 cm3 of corticocancellous bone was collected from each iliac crest, according to the procedure reported by Brecevich et al. [13]. Animals were sacrificed 6 weeks post-arthrodesis for histological evaluation of the intervened structures.
Histological evaluation
Sections of the lumbar spine were collected, cleaned, and submitted to fixation and decalcification using 0.25 M of EDTA (sigma, pH 7.3) for 7 weeks with agitation. Afterward, samples were submitted to an ethanol series for dehydration. Next, the samples were embedded in paraffin blocks, and serial sections were prepared for picrosirius red and Masson's trichrome staining procedures using standard protocols. The stained slides were analyzed using a stereomicroscope (SZX10, Olympus) and an inverted microscope (Axiovert 200 M, Zeiss). The picrosirius red stained sections were visualized through a polarized lens coupled to a binocular inverted microscope (Zeiss, Axiovert 200 M) to study collagen birefringent fibers. This technique can be used to distinguish the thickness and packing (maturation) of collagens. Type I collagen stains in red, whereas type III collagen in green [14, 15]. All images were acquired using the same parameters (light intensity and angle of the polarizing lens).
Fibrous capsule analysis
Evaluation of the fibrous capsule formed around the implanted scaffolds and the iliac bone autograft was performed by measuring its thickness using Masson's trichrome stained sections. Axion Vision software was used for the measurements. The fibrous capsule area was analyzed by drawing a line throughout the capsule, and afterwards the fibrous capsule thickness was measured as the average thickness of fifteen different random locations throughout the capsule. Since these results are from a pilot study and we have a limited number of animals (three per group) we consider that this does not allow a correct statistical analysis and could lead to an incorrect interpretation of the results. Therefore, we have not performed statistical analysis.
Results
We have used here a rat model of vertebral arthrodesis to test by histological screening the usefulness of implanting a porous 3D chitosan scaffold with resolvin D1 incorporated. The histological evaluation was performed on the lumbar spine area at the level of L4 and L5 for all experimental groups. Figure 1 presents Masson's trichrome stained sections with different magnifications allowing for a general view of the lumbar vertebrae (A) and a detailed view (B and C) of the interface between bone and muscle tissue (non-operated); bone and Ch scaffolds with RvD1 (Chitosan + RvD1); and bone and autologous bone (iliac bone autograft). In the images of the general view presented in (A), we can visualize the anatomical elements of the rat lumbar vertebra and identify the implantation area of the Ch scaffolds and the autologous bone graft. Both can be visualized in the posterolateral face of the vertebrae in the area where the lamina was decorticated, close to the lamina-spinous process transition. In the detailed views presented in (B) and (C), we observe the formation of a collagenous fibrous capsule (FC) around the implants, as Masson's trichrome highlights collagen fibers. This fibrous capsule was thinner in the group implanted with Ch scaffolds when compared with iliac bone autograft. Interestingly, we found new bone formation (NB) within the porous Ch scaffold, inside the open spaces of the scaffold that resulted from Ch microstructure degradation. To complement these observations, Fig. 2 shows similar images using picrosirius red staining and acquired using transmitted light. Using this staining, the NB within the Ch scaffolds can be more clearly visualized.
Histological sections of lumbar vertebrae stained with Masson's trichrome of the different experimental groups: non-operated animals, animals implanted with Ch scaffolds with RvD1 and animals with an implanted iliac bone autograft. A Global view of the area; B and C Detailed view of the intervened area. (VB) Vertebral body; (VF) Vertebral foramen; (L) Lamina; (SP) Spinous process; (Ch) Chitosan + RvD1 scaffold; (IA) Iliac bone autograft; (NB) Newly formed bone; (FC) Fibrous capsule. (Scale bar: 0.5 mm)
Panel of Global (A) and detailed view (B and C) of histological sections stained with picrosirius red of the intervened area in lumbar vertebrae of non-operated animals, animals implanted with Ch scaffolds with RvD1 and animals with an implanted iliac bone autograft. (VB) Vertebral body; (VF) Vertebral foramen; (L) Lamina; (SP) Spinous process; (Ch) Chitosan + RvD1 scaffold; (IA) Iliac bone autograft; (NB) Newly formed bone; (FC) Fibrous capsule. (Scale bar: 0.5 mm)
Figure 3 displays images of picrosirius red stained sections obtained under polarized light. The red color in the birefringence analysis indicates thick collagen fibers, whereas green birefringence color indicate thin fibers. Additionally, homogenous red staining is indicative of mature collagen that is highly packed and thicker. We observed a predominance of red birefringence fibers, which is expectable due to the 6 weeks implantation time used in this pilot study. The images show red birefringent collagenous fibers around the implanted Ch scaffolds and the implanted iliac bone autograft. We observed a more intense red birefringence around the iliac bone autograft indicative of a thicker and packed collagenous capsule—and, therefore, more mature—compared with the one observed in the implanted Ch scaffolds.
Histological sections of picrosirius red staining of the non-operated animals and animals implanted either with Ch scaffolds with RvD1 or with autologous iliac bone graft. A Transmitted light. B Polarized light. Red birefringence color indicates thick collagen fibers, whereas green birefringence color indicates thinner fibers. (Scale bar: 0.5 mm)
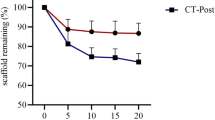
The thickness measurement of the fibrous capsule formed around the implants is presented in Fig. 4. The fibrous capsule thickness in iliac bone autograft group is higher in comparison with the implanted Ch scaffolds with resolvin D1 group, as shown in Figs. 1 and 2. In addition, the images obtained using polarized light presented in Fig. 3 provide additional information on the degree of maturation of the fibrous capsule's collagen fibers, which are thicker and more packed in the iliac bone autograft group.
Discussion
There are several possibilities available to be used as bone grafts. An interesting solution is the association of molecules able to stimulate osteoblast function or modulate inflammation with biomaterials [16]. Ideally, these newly developed biomaterials would allow appropriate bone healing without the need to use autograft or high-dose growth factors while causing minimal inflammatory response [17].
In this pilot study, we have explored the use of 3D porous Ch scaffolds embedded with RvD1 as a possible alternative for iliac bone grafts. For that, we performed a procedure to promote bilateral posterolateral lumbar vertebral arthrodesis at the level of L4 and L5. We developed and implemented this animal model for the first time. We have mimic the human scenario being evaluated, using a methodology similar to that seen clinically which is considered critical to have a valid in vivo model [18].
We have previously demonstrated that Ch scaffolds with RvD1 have immunomodulatory properties. Using a rodent air pouch inflammation model, we shifted the macrophage polarization profile towards an M2 anti-inflammatory phenotype. We have also observed a decrease in pro-inflammatory cytokines and in the thickness of the fibrous capsule formed around the implants [8]. Additionally, we have tested this immunomodulatory biomaterial in a rat femur critical size defect model and observed a positive effect on bone repair [11]. These interesting results included the decrease in fibrous capsule formation and new bone formation within the Ch scaffold.
Chitosan-based biomaterials have been extensively studied for biomedical applications, namely for bone repair. Chitosan is a biocompatible and versatile natural polymer that can be used alone or in combination with other polymers to form gels, micro/nanoparticles, and films to be applied as drug delivery systems for bone regeneration [19]. Chitosan-based biomaterials are also being explored for spinal applications. Rodríguez-Vázquez et al. [20] developed a chitosan-hydroxyapatite scaffold, and reported that a composite of chitosan-hydroxyapatite with a 20:80 ratio lead to bone formation in a model of lumbar laminectomy. Carvalho et al. [21] produced chitosan-silane membranes for lumbar surgery. These membranes were applied in an experimental model of lumbar laminectomy and the authors observed signs of bone tissue repair in continuity with native bone.
In the process of osteogenesis and bone tissue repair it is important to control inflammation and induce an anti-inflammatory response through an M2 anti-inflammatory macrophage response. The process of bone healing can be divided in three phases: inflammatory, repair and remodeling. The healing process is greatly influenced by the initial inflammatory response. The resolution of the inflammatory response begins a few hours after the acute inflammatory response is initiated. In the resolution process the initial inflammatory stimuli are eliminated; the pro-inflammatory mediators are suspended, and the anti-inflammatory and pro-resolving mediators are promoted [22]. RvD1 has important anti-inflammatory effects; it stimulates macrophage phagocytosis of microbes, efferocytosis of apoptotic polymorphonuclear leukocytes and controls macrophage polarization [23]. Thus, the use of RvD1 has a positive role in creating an anti-inflammatory microenvironment having a positive role in bone tissue repair. Additionally, the prevention of epidural adhesion is still a significant challenge in spinal surgery [24, 25]. Our results suggest a potential beneficial effect of RvD1 to overcome this problem, however this potential interesting effect needs to be further explored in future studies.
This pilot study underlines the importance of incorporating RvD1 within the implanted scaffolds. Future studies should focus on improving the ability to form new bone while maintaining the interesting anti-inflammatory effect of RvD1. We propose that a combination of chitosan with a calcium phosphate-based material to accelerate new bone repair while maintaining the use of RvD1 would be a promising approach.
Final considerations
We have developed an alternative procedure to iliac bone autografts used in spinal surgery. We have incorporated resolvin D1 (RvD1), a pro-resolution lipid mediator with anti-inflammatory properties, in chitosan (Ch) 3D scaffolds. Our results suggest an important anti-inflammatory effect of RvD1 that leads to the formation of a thinner fibrous capsule around the Ch + RvD1 scaffolds compared to iliac bone autograft. New bone formation was also seen within the implanted Ch + RvD1 scaffolds. Thus, this pilot study points to new formulations for biomaterials to be used in future studies on vertebral arthrodesis.
References
Noh T, Zakaria H, Massie L, Ogasawara CT, Lee GA, Chedid M (2021) Bone marrow aspirate in spine surgery: case series and review of the literature. Cureus 13(12):e20309. https://doi.org/10.7759/cureus.20309
Sheha ED, Meredith DS, Shifflett GD, Bjerke BT, Iyer S, Shue J, Nguyen J, Huang RC (2018) Postoperative pain following posterior iliac crest bone graft harvesting in spine surgery: a prospective, randomized trial. Spine J 18(6):986–992. https://doi.org/10.1016/j.spinee.2017.10.011
Kim H, Kar AK, Kaja A, Lim EJ, Choi W, Son WS, Oh JK, Sakong S, Cho JW (2021) More weighted cancellous bone can be harvested from the proximal tibia with less donor site pain than anterior iliac crest corticocancellous bone harvesting: retrospective review. J Orthop Surg Res 16(1):220. https://doi.org/10.1186/s13018-021-02364-y
Fiani B, Jarrah R, Shields J, Sekhon M (2021) Enhanced biomaterials: systematic review of alternatives to supplement spine fusion including silicon nitride, bioactive glass, amino peptide bone graft, and tantalum. Neurosurg Focus 50(6):E10. https://doi.org/10.3171/2021.3.FOCUS201044
Gillman CE, Jayasuriya AC (2021) FDA-approved bone grafts and bone graft substitute devices in bone regeneration. Mater Sci Eng C Mater Biol Appl 130:112466. https://doi.org/10.1016/j.msec.2021.112466
Golubovsky JL, Ejikeme T, Winkelman R, Steinmetz MP (2021) Osteobiologics. Oper Neurosurg (Hagerstown) 21(Suppl 1):S2–S9. https://doi.org/10.1093/ons/opaa383
Tang G, Liu Z, Liu Y, Yu J, Wang X, Tan Z, Ye X (2021) Recent trends in the development of bone regenerative biomaterials. Front Cell Dev Biol 9:665813. https://doi.org/10.3389/fcell.2021.665813
Vasconcelos DP, Costa M, Amaral IF, Barbosa MA, Aguas AP, Barbosa JN (2015) Development of an immunomodulatory biomaterial: using resolvin D1 to modulate inflammation. Biomaterials 53:566–573. https://doi.org/10.1016/j.biomaterials.2015.02.120
Tian Y, Wu D, Wu D, Cui Y, Ren G, Wang Y, Wang J, Peng C (2022) Chitosan-based biomaterial scaffolds for the repair of infected bone defects. Front Bioeng Biotechnol 10:899760. https://doi.org/10.3389/fbioe.2022.899760
Freire MO, Van Dyke TE (2013) Natural resolution of inflammation. Periodontol 2000 63(1):149–164. https://doi.org/10.1111/prd.12034
Vasconcelos DP, Costa M, Neves N, Teixeira JH, Vasconcelos DM, Santos SG, Aguas AP, Barbosa MA, Barbosa JN (2018) Chitosan porous 3D scaffolds embedded with resolvin D1 to improve in vivo bone healing. J Biomed Mater Res, Part A 106(6):1626–1633. https://doi.org/10.1002/jbm.a.36370
Vasconcelos DP, Fonseca AC, Costa M, Amaral IF, Barbosa MA, Aguas AP, Barbosa JN (2013) Macrophage polarization following chitosan implantation. Biomaterials 34(38):9952–9959. https://doi.org/10.1016/j.biomaterials.2013.09.012
Brecevich AT, Kiely PD, Yoon BV, Nguyen JT, Cammisa FP, Abjornson C (2017) Efficacy comparison of Accell Evo3 and Grafton demineralized bone matrix putties against autologous bone in a rat posterolateral spine fusion model. Spine J 17(6):855–862. https://doi.org/10.1016/j.spinee.2017.01.012
Montes GS, Junqueira LC (1991) The use of the Picrosirius-polarization method for the study of the biopathology of collagen. Mem Inst Oswaldo Cruz 86(Suppl 3):1–11. https://doi.org/10.1590/s0074-02761991000700002
Vieira AE, Repeke CE, Ferreira Junior Colavite SdeBPM, Biguetti CC, Oliveira RC, Assis GF, Taga R, Trombone AP, Garlet GP (2015) Intramembranous bone healing process subsequent to tooth extraction in mice: micro-computed tomography, histomorphometric and molecular characterization. PLoS ONE 10(5):e0128021. https://doi.org/10.1371/journal.pone.0128021
Masalskas BF, Martins W, Leoni GB, Faloni APD, Marcaccini AM, Sousa YTCS, de Castro-Raucci LMS (2018) Local delivery of strontium ranelate promotes regeneration of critical size bone defects filled with collagen sponge. J Biomed Mater Res Part A 106(2):333–341. https://doi.org/10.1002/jbm.a.36237
Plantz MA, Gerlach EB, Hsu WK (2021) Synthetic bone graft materials in spine fusion: current evidence and future trends. Int J Spine Surg 15(s1):104–112
Drespe IH, Polzhofer GK, Turner AS, Grauer JN (2005) Animal models for spinal fusion. Spine J 5(6 Suppl):209S-216S. https://doi.org/10.1097/BRS.0000000000004142
Rahimi M, Mir SM, Baghban R, Charmi G, Plummer CM, Shafiei-Irannejad V, Soleymani J, Pietrasik J (2022) Chitosan-based biomaterials for the treatment of bone disorders. Int J Biol Macromol 215:346–367. https://doi.org/10.1016/j.ijbiomac.2022.06.079
Rodriguez-Vazquez M, Ramos-Zuniga R (2020) Chitosan-hydroxyapatite scaffold for tissue engineering in experimental lumbar laminectomy and Posterolateral spinal fusion in Wistar rats. Asian Spine J 14(2):139–147. https://doi.org/10.31616/asj.2019.0091
Carvalho M, Costa LM, Pereira JE, Shirosaki Y, Hayakawa S, Santos JD, Geuna S, Fregnan F, Cabrita AM, Mauricio AC, Varejao AS (2015) The role of hybrid chitosan membranes on scarring process following lumbar surgery: post-laminectomy experimental model. Neurol Res 37(1):23–29. https://doi.org/10.1179/1743132814Y.0000000414
Maruyama M, Rhee C, Utsunomiya T, Zhang N, Ueno M, Yao Z, Goodman SB (2020) Modulation of the inflammatory response and bone healing. Front Endocrinol (Lausanne) 11:386. https://doi.org/10.3389/fendo.2020.00386
Serhan CN, Dalli J, Colas RA, Winkler JW, Chiang N (2015) Protectins and maresins: new pro-resolving families of mediators in acute inflammation and resolution bioactive metabolome. Biochem Biophys Acta 1851(4):397–413. https://doi.org/10.1016/j.bbalip.2014.08.006
Chen HY, Lin TC, Chiang CY, Wey SL, Lin FH, Yang KC, Chang CH, Hu MH (2021) Antifibrotic effect of Bletilla striata polysaccharide-resveratrol-impregnated dual-layer carboxymethyl cellulose-based sponge for the prevention of epidural fibrosis after laminectomy. Polymers (Basel) 13(13):2129. https://doi.org/10.3390/polym13132129
Wang Y, Li L, Ma Y, Tang Y, Zhao Y, Li Z, Pu W, Huang B, Wen X, Cao X, Chen J, Chen W, Zhou Y, Zhang J (2020) Multifunctional supramolecular hydrogel for prevention of epidural adhesion after laminectomy. ACS Nano 14(7):8202–8219. https://doi.org/10.1021/acsnano.0c01658
Funding
Open access funding provided by FCT|FCCN (b-on). Not applicable. No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. All authors participated in the preparation of the manuscript. All authors read and approved the final manuscript. The in vivo procedures were performed by DV, MC, VS, JR. Histological evaluation, image collection and analysis were performed by DV, MC, AS, JB.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to this article was reported.
Ethical approval
The experimental protocols were planned and performed in accordance with guidelines approved by the Ethics Committee and the Portuguese Official Authority on Animal Welfare and Experimentation (DGAV). The procedures were also reviewed and authorized by the in-house Animal Welfare Body, “Órgão Responsável pelo Bem-Estar Animal: ORBEA”, to positively affect the quality of the studies and animal welfare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Daniela P. Vasconcelos and Madalena Costa shared first authorship.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vasconcelos, D.P., Costa, M., Reis, J.L. et al. Chitosan 3D scaffolds with resolvin D1 for vertebral arthrodesis: a pilot study. Eur Spine J 32, 1985–1991 (2023). https://doi.org/10.1007/s00586-023-07725-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07725-1