Abstract
Background
Restoration of three-dimensional (3D) alignment is critical in correcting patients with adolescent idiopathic scoliosis using posterior spinal fusion (PSF). However, current studies mostly rely on 2D radiographs, resulting in inaccurate assessment of surgical correction and underlying predictive factors. While 3D reconstruction of biplanar radiographs is a reliable and accurate tool for quantifying spinal deformity, no study has reviewed the current literature on its use in evaluating surgical prognosis.
Purpose
To summarize the current evidence on patient and surgical factors affecting sagittal alignment and curve correction after PSF based on 3D parameters derived from reconstruction of biplanar radiographs.
Methods
A comprehensive search was conducted by three independent investigators on Medline, PubMed, Web of Science, and Cochrane Library to obtain all published information on predictors of postoperative alignment and correction after PSF. Search items included "adolescent idiopathic scoliosis," "stereoradiography," "three-dimensional," "surgical,” and "correction." The inclusion and exclusion criteria were carefully defined to include clinical studies. Risk of bias was assessed with the Quality in Prognostic Studies tool, and level of evidence for each predictor was rated with the Grading of Recommendations, Assessment, Development, and Evaluations approach. 989 publications were identified, with 444 unique articles subjected to full-text screening. Ultimately, 41 articles were included.
Results
Strong predictors of better curve correction included preoperative normokyphosis (TK > 15°), a corresponding rod contour, intraoperative vertebral rotation and translation, and upper and lower instrumented vertebrae selected based on sagittal and axial inflection points. For example, for Lenke 1 patients with junctional vertebrae above L1, fusion to NV-1 (1 level above the neutral vertebra) achieved optimal curve correction while preserving motion segments. Pre-op coronal Cobb angle and axial rotation, distal junctional kyphosis, pelvic incidence, sacral slope, and type of instrument were identified as predictors with moderate evidence. For Lenke 1C patients, > 50% LIV rotation was found to increase spontaneous lumbar curve correction. Pre-op thoracolumbar apical translation and lumbar lordosis, Ponte osteotomies, and rod material were found to be predictors with low evidence.
Conclusions
Rod contouring and UIV/LIV selection should be based on preoperative 3D TK in order to achieve normal postoperative alignment. Specifically, Lenke 1 patients with high-lying rotations should be fused distally at NV-1, while hypokyphotic patients with large lumbar curves and truncal shift should be fused at NV to improve lumbar alignment. Lenke 1C curves should be corrected using > 50% LIV rotation counterclockwise to the lumbar rotation. Further investigation should compare surgical correction between pedicle-screw and hybrid constructs using matched cohorts. DJK and overbending rods are potential predictors of postoperative alignment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a complex three-dimensional deformity that can progress if untreated, causing chronic back pain and significant pulmonary impairment [1,2,3,4,5,6,7]. Generations of surgical procedures have aimed at correcting the frontal curve and truncal deformity while maintaining spinopelvic alignment [8,9,10,11,12,13,14,15,16]. As 40–46% of all AIS patients are hypokyphotic, special attention should be paid to restoring sagittal balance in these patients, with studies supporting that failure to restore thoracic kyphosis (TK) may predispose to proximal or distal junctional kyphosis, as well as late complications predisposing to future decompensation [17,18,19,20,21]. While pedicle-screw systems have been shown to demonstrate efficacious correction in the frontal and axial planes by the placement of powerful anchors, they have been shown to cause flattening of the sagittal spine [22,23,24].
To evaluate and improve postoperative correction, numerous factors have been extensively investigated using conventional 2D radiographs, with mixed consensus within the current literature regarding the difference in surgical correction from different factors [25,26,27,28,29]. Prior studies have shown such relationship with patient-related factors including preoperative curve magnitude and flexibility, and with surgical factors including implant density, fusion length, and the type of instrument and technique used, such as differential rod contouring, direct vertebral rotation, and Ponte osteotomies [30,31,32,33,34,35,36,37,38,39].
As many of the studies compared surgical correction rates using plain radiographs, the true deformity of the spine has been inaccurately evaluated. Notably, 2D thoracic kyphosis (TK) has been shown to be variably overestimated on 2D radiographs by an average of 10° due to technical difficulty in visualizing thoracic endplates and the varying magnitude of axial rotation among patients [40,41,42,43,44,45,46]. Due to vertebral rotation in the transverse plane, lateral radiographs do not allow for a true lateral assessment of the sagittal plane [41, 47]. In addition, while axial rotation causes rib hump deformity, it is often inaccurately assessed by the Nash–Moe method on 2D which results in a mean 8–10° error [48, 49]. Moreover, prior studies have shown statistically significant differences in 2D and 3D Cobb angles due to pelvic rotation. With increasing focus placed on tridimensional alignment, there comes a need for more accurate methods in quantifying spinal deformity, so as to improve rod contouring and selection of end-instrumented vertebrae to be better aligned to the true morphology of the spine [50, 51].
In recent years, three-dimensional reconstruction of biplanar radiographs has emerged as a method that allows accurate measurement of axial rotation and adjustment for axial rotation for a more accurate evaluation of the spine in its true planes [52,53,54,55,56,57,58]. After manual localization of the T1-L5 vertebral bodies, 3D spinal parameters will be automatically calculated with normalization of patient rotation. Notably, changes in 3D TK, wedging, intervertebral rotation, and orientation of the plane of maximum curvature are parameters unique to 3D reconstruction and may act as outcome variables to reflect the 3D morphology of the spine more accurately [59,60,61,62,63,64]. Therefore, this study aims to summarize the patient and surgical factors affecting three-dimensional correction after posterior spinal fusion (PSF) based on reconstruction of biplanar radiographs.
Methods
Literature search strategy and selection criteria
The protocol for this systematic review has been registered in PROSPERO (CRD42022373484) on 23/11/2022 [65]. The literature search and reporting of results in this review were conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [66]. An extensive search was performed on the following databases: PubMed, Web of Science, MEDLINE, and Cochrane Library. All fields were searched in the databases using the following keywords: "adolescent idiopathic scoliosis," "stereoradiography," "reconstruction," "three-dimensional," "surgical," "correction," "postoperative," and "junctional kyphosis." Detailed search items are included in Supplementary Material.
The search was limited to publications from 2010 to 2022 to exclude surgical techniques that are rarely used currently. The inclusion criteria included randomized controlled trials, cohort studies, case–control studies, and case series reporting predictors of postoperative alignment and surgical correction based on 3D reconstruction of biplanar radiographs. To maximize overall sample size, studies using validated algorithms to estimate 3D T4-T12 kyphosis based on biplanar radiographs were also included [41, 67]. The exclusion criteria included studies involving anterior spinal fusion, non-English publications, case reports, biomechanical studies, non-human or cadaveric studies, and studies with a sample size < 20. Studies evaluating thoracic volume and lung function were excluded since this was beyond the scope of this systematic review.
The search and screening process were conducted by three independent investigators (SW, ST, DW). Potentially relevant abstracts were screened based on the inclusion criteria, and full-text articles were obtained for eligible results. Three investigators discussed any disagreements regarding accepting full-text articles until consensus was achieved. References of each article were screened to look for potentially relevant studies.
Data extraction and critical appraisal
The primary outcome of this systematic review was the effects of patient-related predictors and surgery-specific predictors on 3D curve correction after PSF.
Patient-related predictors included preoperative 3D radiographic measurements, which included Cobb angle, thoracic kyphosis and lumbar lordosis, axial vertebral rotation, pelvic parameters, vertebral tilt and translation, and junctional kyphosis. Surgery-specific predictors included the type of instrument used, selection of upper instrumented vertebra (UIV) and lower instrumented vertebra (LIV), rod contouring, rod material, and number of Ponte osteotomies.
The amount of 3D curve correction was defined by intraoperative correction (preoperative to first standing postoperative X-ray) and spontaneous changes between follow-up visits. The parameters included changes in Cobb angle, thoracic kyphosis, axial rotation, pelvic parameters, and proximal junctional kyphosis in the fused and unfused spine. In addition, shoulder-height difference was included, as well as global sagittal alignment, as measured using sagittal vertical axis (SVA), the distance between the center of T1 and the central hip vertical axis (T1–CHVA), and odontoid-hip angle (OD-HA).
Details regarding each study’s sample size, design, inclusion criteria, predictors identified, radiological definition of novel 3D parameters, risk of bias, phase of inquiry, and level of evidence are recorded in Table 1.
Risk of bias
The risk of bias of these publications was assessed using the six domains of the Quality in Prognostic Studies (QUIPS) tool by the three independent reviewers, and consensus was reached after discussion [68]. For retrospective studies, bias due to attrition is not applicable and therefore not assessed. The QUIPS risk of bias for these studies is detailed in Table 2.
Grading of evidence
The quality of evidence for each factor included was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach by the three independent reviewers [69]. Factors with evidence mainly coming from confirmatory studies were initially assigned with a high level of evidence, while factors with evidence mainly coming from exploratory studies were assigned a moderate level of evidence. The quality of evidence was downgraded by one level according to the following criteria: inconsistency, imprecision, indirectness, and publication bias. The quality of evidence was upgraded by one level for the following cases: strong evidence of association between independent variables and outcomes, evidence of dose–response gradient, and when all residual confounding was shown to reduce the demonstrated effect. The detailed evidence available for each factor and the GRADE quality of evidence rating is presented in Table 3.
Search results
The search results are illustrated in the PRISMA flowchart (Fig. 1). A total of 985 articles were yielded from the initial search, of which 253 articles were from Medline, 376 articles from Web of Science, 46 articles from Cochrane library, and 310 articles were from PubMed. Of the 985 articles, there were 545 duplicated articles, and 440 unique articles were screened for the inclusion and exclusion criteria. As a result, a total of 36 articles from 34 datasets were included in the final study for further analysis.
PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) Flowchart detailing the data screening process. A total of 985 articles were yielded from the initial search, of which 440 unique articles were screened for the inclusion and exclusion criteria. As a result, a total of 36 articles were included in the final study for further analysis
Among the 36 publications included, 18 were classified as confirmatory studies, and 18 were classified as exploratory studies. In terms of study design, 31 were retrospective cohort studies, 5 were retrospective case–control studies, and there were no cross-sectional studies or randomized controlled trials. The mean age of subjects across studies ranged from 10 to 21 years, and the length of follow-up ranged from 12 months to 2.4 years. Sample sizes of studies ranged from 20 to 1063 subjects.
Results
Patient-related predictors
For studies reporting patient-related predictors of 3D correction, the earliest study was published in 2016 [60], and the instrumentation was all pedicle-screw constructs.
Sagittal alignment
There is strong evidence that preoperative thoracic kyphosis affects 3D curve correction. In a multivariate analysis of 371 subjects, Pasha et al. [70, 71] found that preoperative clusters, which shared significant differences in TK, predicted three clusters of 3D surgical outcomes with an accuracy of 64%. Regarding global alignment, Yeung et al. [72] reported that hypokyphotic patients had adopted a more forward-leaning posture to compensate for global sagittal imbalance (indicated by SVA-SFD and sagittal OD-HA) compared to normokyphotic adolescent idiopathic scoliosis (AIS) subjects. However, this improved from immediate post-op to the 2-year postoperative follow-up. However, there is limited strength of evidence as there were only 7 hypokyphotic subjects in the whole cohort. There is moderate evidence that distal junctional kyphosis (DJK), pelvic incidence (PI), and sacral slope (SS) affect postoperative curve magnitude and alignment from a study by Pasha et al. [71]. For lumbar lordosis and thoracolumbar apical translation, which were also identified in the same study, there is low evidence that these two parameters affect postoperative alignment due to lack of effect size measurement and relatively low variable importance in the predictive model.
Axial rotation
There is moderate evidence that preoperative axial rotation affects surgical correction. The preoperative 3D clusters with high prognostic value reported by Pasha et al. [70] had significant differences in the magnitude of apical vertebral rotation (AVR) and comprised two types of axial projections as viewed from above — lemniscate-shaped and loop-shaped projections, with the former having two significant rotations and the latter only having one significantly rotated curve. Shen et al. [73] reported that patients with higher preoperative torsion showed comparable postoperative coronal Cobb angle, but there were differences in the orientation of the plane of maximum deformity in the thoracolumbar segment between the high and low torsion groups (47.95° vs. 30.03°).
Coronal Cobb angle
There is moderate evidence that preoperative Cobb angle affects surgical correction, as most studies focused on planes with greater difference between 2D and 3D imaging. The preoperative clusters demonstrated by Pasha et al. [70] had statistically significant differences in proximal thoracic (PT), main thoracic (MT), and thoracolumbar/lumbar (TL/L) Cobb angle. Machida et al. [74] reported that postoperative Cobb angle and AVR in the PT curve had small to moderate association with radiographic shoulder height differences up to the 2-year follow-up.
Surgical factors
Type of instrumentation
There is moderate evidence that the instrumentation affects surgical outcomes. Sikora-Klak et al. [75] reported that the use of all-screw instrumentation was associated with significantly better coronal correction and slightly better restoration of TK when compared to hybrid constructs, while Kato et al. [76] reported greater axial correction using all-screw systems. However, both studies did not adjust for preoperative curve parameters, which were unequal between the case–control groups, and other surgical factors were not accounted for.
UIV and LIV selection
There is strong evidence that the amount of surgical correction is associated with UIV and LIV selection. Pasha et al. [77] found that following preoperative 3D classification of 76 patients, UIV and LIV selection had different impacts on the surgical outcomes in each of the five subtypes. For example, LIV at T12 in Type 1 and UIV at T2 in Type 2 were associated with improved frontal balance and lower proximal junction kyphosis (PJK), respectively. This association was also found in a larger study of 371 subjects by Pasha et al. [70].
Vertebral tilt and translation
There is strong evidence that the amount of surgical correction is associated with the relative positioning of the apical and end-instrument vertebrae, a function of the degree of translation and derotation during correction. Homans et al. [78] reported that a higher PJK angle was correlated with a larger anterior shift of UIV during surgical correction and a more posterior position of UIV at the most recent follow-up. Regarding selective thoracic fusion in patients with main thoracic curves and lumbar modifiers, Pasha et al. [79] found that in addition to thoracic curve correction, leveling of the LIV (i.e., reducing frontal tilt) was the factor most likely to result in greater 3D correction of the uninstrumented lumbar curve.
Rod material
There is weak evidence that rod material influences 3D surgical correction. Among 10 studies, 5 studies each reported the use of titanium (Ti), stainless steel (SS), and cobalt–chromium (CoCr) rods, respectively. Comparing all three rod materials, Le Navéaux et al. [80] reported that there was no significant 3D shape change of the instrumented spine or of the rods from 1-week post-op to the 2-year follow-up. However, there were only 14 subjects in each group. Ilharreborde et al. [81] also reported no significant differences between Ti and CoCr rods in 3D outcomes in 35 hypokyphotic subjects. In another study of 153 AIS patients by Kato et al. [76], no difference in AVR correction was observed between Ti and SS rods. In a study of 134 AIS patients with severe thoracic lordosis, Newton et al. [82] found that better TK restoration was moderately associated with the use of SS rods rather than CoCr rods (p < 0.01, η2 = 0.08).
Rod contouring
There is strong evidence that rod shape in relation to spine contour influences surgical correction. To quantify rod contour in relation to the scoliotic curve, Kluck et al. reported a novel 3D parameter, the rod-to-spine distance (RSD), while Le Navéaux et al. [83] measured the difference between rod curvature and kyphosis (°). Both parameters moderately correlated with change in 3D thoracic kyphosis. Le Navéaux et al. [50] reported that pre-insertion concave rod curvature itself was not predictive of postoperative thoracic kyphosis due to rod flattening during instrumentation. In addition, the plane of maximum curvature of the rods deviated from the sagittal plane after surgical instrumentation. This was supported by Kluck et al. [84], who found that preoperative rod angle difference was decreased by 9° on average, with the convex rod generally being more curved than the concave rod post-instrumentation. For axial correction, Le Navéaux et al. [80] reported a modest positive association between the amount of differential contouring performed between the concave and convex rods and the degree of AVR correction (R2 = 0.28).
Ponte osteotomies in patients with severe thoracic lordosis
There is weak evidence that Ponte osteotomies influence surgical outcomes. In a matched comparison of severe AIS patients by Floccari et al. [67], Ponte osteotomies were reported to provide small radiographic gains in the coronal plane (66.6% vs 58.7%) with no improvement in the sagittal plane and no change in truncal rotation. This was reciprocated in a study by Newton et al. [82], which found that use of Ponte osteotomies was only weakly associated with improved thoracic kyphosis (η2 = 0.04).
Discussion
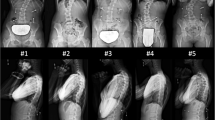
In recent decades, sagittal alignment has been highlighted as an important surgical aim in the correcting scoliotic deformities, yet this is often sacrificed using pedicle-screw systems in favor for correction in the coronal and axial planes. Despite thorough investigations into the effect of various factors on postoperative correction, results remain inconsistent. This may be explained by the reliance on 2D imaging for the measurement of spinal parameters, which results in inaccurate estimation of surgical correction, especially for patients with severe curves. While reconstruction of low-dose biplanar images serves as a safe and reliable method for evaluating three-dimensional curve deformities, a full modeling process for each patient is time-consuming and labor intensive, potentially limiting large-scale studies. In this review, we have collected and summarized the key predictors of 3D postoperative alignment and correction for PSF. Preoperative 3D thoracic kyphosis, UIV and LIV selection, rod contour, and intraoperative vertebral rotation were found to be predictive of postoperative outcomes with strong evidence (Fig. 2). Pre-op coronal Cobb angle and axial rotation, DJK, pelvic parameters (PI and SS), and type of instrument were found to be predictive of postoperative outcomes with moderate evidence, while pre-op TL apical translation, Ponte osteotomies, rod material, and lumbar lordosis were found to be predictors with low evidence.
A summary of the findings of this systematic review. UIV and LIV selection, preoperative 3D TK, rod contour, and EIV rotation were identified as predictors of surgical outcome with strong evidence. Predictors with moderate evidence included preoperative coronal Cobb angle, AVR, PI, SS, and type of instrument. Predictors with weak evidence included rod material and Ponte osteotomies. *UIV = upper instrumented vertebra, LIV = lower instrumented vertebra, 3D TK = three-dimensional thoracic kyphosis, EIV = end-instrumented vertebra, AVR = apical vertebral rotation, PI = pelvic incidence, SS = sacral slope
Patient-related factors and EIV selection
Preoperative coronal Cobb angle, thoracic kyphosis and axial rotation were identified as important predictors of postoperative sagittal and axial alignment, which reflects residual deformities in patients with severe curves, hypokyphosis or high torsion with less flexibility initially. While there may be associations between initial curve characteristics and postoperative outcomes across different planes, these are mostly due to aggressive intraoperative correction maneuvers causing disturbances in other planes [83]. The key value of assessing preoperative 3D spinal morphology arises from the comparison of surgical correction within subgroups of 3D curves, so as to achieve patient-specific surgical treatment. In a series of studies by Pasha et al. [70, 77, 85], UIV and LIV selection had different impacts on the surgical outcomes among preoperative clusters based on 3D spinal morphology. Where to fuse Lenke 1A curves distally has been a long-debated topic, with distal adding-on, PJK, and residual motion as the main concerns. For patients with NV close to EV, Suk et al. [86] recommended fusion to the neutral vertebra (NV) or NV-1. However, manual identification of NV and EV has been criticized to be unreliable among observers [87, 88]. Based on 3D analysis of axial rotation, Pasha et al. [70] suggested that the shape of axial projection may reflect the relationship between NV and EV and could be a potential determinant of fusion level for optimal postoperative alignment. For example, Lenke 1 patients with lemniscate-shaped axial projections have higher junctional vertebrae and should be fused to NV-1. For preoperative sagittal parameters, Vidal et al. [89] suggested that for hypokyphotic subjects with a low PI, overcorrection of LL in distal fusions led to poor sagittal balance postoperatively. Based on analysis of 3D spinal parameters, Pasha et al. [70] suggested that for hypokyphotic patients who have a high sagittal inflection point, fusion should be extended to the lumbar spine to improve postoperative sagittal balance. With this information, surgeons may optimize postoperative alignment while sparing motion segments and avoiding PJK and adding-on in selected patients.
Moderate predictive ability was attributed for the following parameters. Though distal junctional kyphosis, PI, and SS were identified as three of the top 5 predictors of postoperative 3D outcome clusters based on a random forest model by Pasha et al. [51, 90], the utility of these parameters as independent predictors remains uncertain, as the top predictors were selected based on mean decrease accuracy, which mostly reflects overall model performance rather than individual effect. In the same study, thoracolumbar apical translation on the sagittal plane and lumbar lordosis was identified as predictors with low evidence due to low mean decrease accuracy. Though the authors did not elaborate on the possible mechanism of these parameters, these sagittal parameters might reflect lumbar and pelvic compensation for sagittal imbalance in hypokyphotic patients [89, 91].
Surgical factors
Studies comparing outcomes of current systems [75, 76] had a generally moderate risk of bias due to important unadjusted factors such as the operating surgeon, fusion length, and baseline patient characteristics. Ilharreborde et al. [35, 81] have extensively reported on the postoperative correction rates of posteromedial translation with sublaminar bands, which shows satisfactory correction in hypokyphotic patients. Whether this method is superior to all-screw systems relies on further investigation with 3D analyses, as the current literature likely has overestimated preoperative thoracic kyphosis using 2D parameters [17, 92], which may account for the reported lordotic effect of pedicle-screw constructs.
End-instrumented vertebrae (EIV) rotation and translation during surgery were significantly predictive of postoperative correction and alignment in several confirmatory studies. The concept of selective thoracic fusion was introduced by King et al. [93] in the 80 s, with the goal of preserving motion segments while allowing spontaneous correction of the compensatory lumbar curve. However, unsatisfactory outcomes including adding-on and overcorrection have been reported, which may be remedied using direct vertebral rotation or translation. Using 3D analysis, Pasha et al. [70, 71] found that leveling EIV tilt and reducing rotation were associated with reduced coronal Cobb angle and rotation in the unfused lumbar spine postoperatively and at latest follow-up. This was also found by Kim et al. [94] and Chang et al. [95] using the Nash–Moe method to measure change in AVR. Using 3D analyses, Zuckerman et al. [96] also found that direct vertebral rotation produced significant improvements in thoracic AVR and AVR in the unfused lumbar curve. In another study by Pasha et al. [79], % EIV derotation was found to have different impacts on surgical outcome across subgroups of lumbar modifiers and sagittal alignment, and patients with C lumbar modifiers were found to benefit from more LIV rotation. Kim et al. [94] supported the findings, noting that for B and C modifiers, LIV rotation counter-clockwise to lumbar rotation produced better curve correction, while for A modifiers, LIV rotation clockwise to lumbar rotation prevented overcorrection and distal adding-on.
As for the effect of EIV shift on sagittal alignment, Homans et al. [78] reported that a larger anterior shift of UIV during surgery was moderately associated with a higher PJK angle. This was attributed to the subsequent rebound of the UIV to a posterior position, which aligned with the hypothesis shared by Alzakri et al. [97, 98] that PJK develops as a compensatory mechanism to restore global sagittal balance in patients with reduced thoracic kyphosis. This further highlights the significance of sagittal alignment, even in patients with normal preoperative kyphosis.
Regarding rod curvature, preoperative rod-to-spine contour was reported to be predictive of change in thoracic kyphosis from two studies with low risk of bias. Kluck et al. [84] quantified rod contour prior to insertion using the rod-to-spine distance, while Le Navéaux et al. [83] measured the difference between rod curvature and kyphosis. Both parameters were found to moderately correlate with change in thoracic kyphosis, and their predictive ability was limited due to flattening of the rods during derotation maneuvers. This has been also identified in a study by Newton et al. [99] based on 2D measurements, and it was suggested that rod overcontouring by 20° could prevent in vivo deformation. For axial correction, differential rod contouring is often performed between the concave and convex rods, in which the concave rod is bent sagittal to a larger degree to rotate the concavity of the curve backward and bring the convexity of the curve anteriorly. Using 3D analysis, Le Navéaux et al. [83] found positive associations between the amount of differential contouring performed and the degree of AVR correction (R2 = 0.28) and orientation of the main thoracic PMC (R2 = 0.41). In a CT study by Seki et al. [100], differential rod contouring > 10° resulted in significant improvement of AVR and rib hump indices.
Rod material was identified as a predictor with low evidence. While SS rods are less popular due to higher infection rates and smaller corrective ability [82, 101, 102], recent studies have converged to compare the surgical outcomes between Ti and CoCr rods, which have different mechanical properties. Ti rods are more elastic, which may undermine in situ bending. Two prior comparative studies [38, 103] have shown that CoCr rods resulted in a mean 3–4° improvement in correction of 2D TK with no difference in other planes. While we identified two studies comparing Ti and CoCr rods [80, 81], both did not find significant changes in any 3D parameters.
Ponte osteotomies were identified as a predictor of postoperative alignment with low evidence. Floccari et al. [67] reported that Ponte osteotomies provided an 8% gain in coronal correction with no differences in other planes. Newton et al. [82] reported that it was weakly associated with improved TK, though preoperative flexibility was not accounted for in this study. While cadaver and biomechanical studies generally demonstrate that Ponte osteotomies increase curve flexibility, human studies have yielded insufficient evidence supporting the efficacy in radiographic correction [104]. However, prior studies did not include matched control groups [104,105,106] and one included normokyphotic subjects [107]. While a large study by Abousamra et al. [108] has shown that intraoperative blood loss was not associated with the number of Ponte osteotomies, its use should still be carefully considered given increased surgical time and potential neurological complications [109].
This is the first review to evaluate the predictors of 3D postoperative alignment and correction after PSF, which includes 3D preoperative spinal parameters and surgical factors. Several limitations were present in this review. First, a meta-analysis could not be conducted due to the lack of comprehensive information on patient characteristics and detailed surgical technique in most of the included studies. However, unless explicitly mentioned otherwise, all included studies used pedicle-screw constructs. Further prognostic studies should include a multivariable analysis adjusted for a set of predictors confirmed in the literature, such as baseline spinal parameters and fusion length. This would be beneficial for identifying new predictors with independent prognostic value. Secondly, publication bias could not be assessed since most studies did not report effect sizes and confidence intervals. However, the strength of evidence was mostly assessable via other domains. Thirdly, no randomized controlled trials or prospective studies were identified during our search. Nevertheless, the predictors extracted from included studies were rigorously examined for quality of evidence.
While it is encouraging to see the emergence of studies on 3D spinal correction, the review identified a paucity in high-quality studies contrasting surgical correction between pedicle-screw and hybrid constructs. Additionally, axial rotation and DJK were recognized as promising factors with potential value in prediction of surgical outcome. We recommend 3D preoperative assessment for patients with severe coronal Cobb angles to identify hypokyphotic candidates and to facilitate surgical planning in these patients. Overbending rods are a potential method to prevent rod flattening during intraoperative correction that requires further investigation. Future work may be expanded using validated algorithms to predict 3D parameters based on 2D ones, which may save time from manual input. Lastly, further research should include comprehensive information on patient and surgical details, taking into consideration the wide array of factors affecting early postoperative as well as long-term outcomes.
Conclusions
In summary, rod contouring and selection of UIV and LIV should be based on sagittal alignment measured using 3D TK. Rods should be contoured to mimic normal thoracic kyphosis while avoiding excessive anterior shift of the UIV in order to prevent PJK. LIV rotation produced favorable outcomes in patients with unfused lumbar curves, while there was low evidence supporting the use of Ponte osteotomies in lordotic patients. Further investigations should compare surgical correction between pedicle-screw and hybrid constructs using matched cohorts.
References
Johnston CE, Richards BS, Sucato DJ, Bridwell KH, Lenke LG, Erickson M (2011) Correlation of preoperative deformity magnitude and pulmonary function tests in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 36(14):1096–1102
Ledonio CG, Rosenstein BE, Johnston CE, Regelmann WE, Nuckley DJ, Polly DW Jr (2017) Pulmonary function tests correlated with thoracic volumes in adolescent idiopathic scoliosis. J Orthop Res 35(1):175–182
Newton PO, Faro FD, Gollogly S, Betz RR, Lenke LG, Lowe TG (2005) Results of preoperative pulmonary function testing of adolescents with idiopathic scoliosis. A study of six hundred and thirty-one patients. J Bone Joint Surg Am 87(9):1937–1946
Teles AR, St-Georges M, Abduljabbar F, Simões L, Jiang F, Saran N et al (2020) Back pain in adolescents with idiopathic scoliosis: the contribution of morphological and psychological factors. Eur Spine J 29(8):1959–1971
Théroux J, Stomski N, Hodgetts CJ, Ballard A, Khadra C, Le May S et al (2017) Prevalence of low back pain in adolescents with idiopathic scoliosis: a systematic review. Chiropr Man Therap 25:10
Yaszay B, Bastrom TP, Bartley CE, Parent S, Newton PO (2017) The effects of the three-dimensional deformity of adolescent idiopathic scoliosis on pulmonary function. Eur Spine J 26(6):1658–1664
Wong AYL, Samartzis D, Cheung PWH, Cheung JPY (2019) How Common is back pain and what biopsychosocial factors are associated with back pain in patients with adolescent idiopathic scoliosis? Clin Orthop Relat Res 477(4):676–686
Acaroglu E, Doany M, Cetin E, Castelein R (2019) Correction of rotational deformity and restoration of thoracic kyphosis are inversely related in posterior surgery for adolescent idiopathic scoliosis. Med Hypotheses 133:109396
Addai D, Zarkos J, Bowey AJ (2020) Current concepts in the diagnosis and management of adolescent idiopathic scoliosis. Childs Nerv Syst 36(6):1111–1119
Bodendorfer BM, Shah SA, Bastrom TP, Lonner BS, Yaszay B, Samdani AF et al (2020) Restoration of thoracic kyphosis in adolescent idiopathic scoliosis over a twenty-year period: Are we getting better? Spine (Phila Pa 1976) 45(23):1625–1633
Dobbs MB, Lenke LG, Kim YJ, Luhmann SJ, Bridwell KH (2006) Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90 degrees. Spine (Phila Pa 1976) 31(20):2386–2391
Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M (2005) Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary? Spine (Phila Pa 1976) 30(18):2061–2067
McMaster MJ (1991) Luque rod instrumentation in the treatment of adolescent idiopathic scoliosis. A comparative study with Harrington instrumentation. J Bone Joint Surg Br 73(6):982–989
Dumpa SR, Shetty AP, Aiyer SN, Kanna RM, Rajasekaran S (2018) Reciprocal changes in sagittal alignment in adolescent idiopathic scoliosis patients following strategic pedicle screw fixation. Asian Spine J 12(2):300–308
Lonner BS, Lazar-Antman MA, Sponseller PD, Shah SA, Newton PO, Betz R et al (2012) Multivariate analysis of factors associated with kyphosis maintenance in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 37(15):1297–1302
Thomas ES, Boyer N, Meyers A, Aziz H, Aminian A (2022) Restoration of thoracic kyphosis in adolescent idiopathic scoliosis with patient-specific rods: Did the preoperative plan match postoperative sagittal alignment? Eur Spine J
Hwang SW, Samdani AF, Tantorski M, Cahill P, Nydick J, Fine A et al (2011) Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: an effect imparted by postoperative thoracic hypokyphosis. J Neurosurg Spine 15(5):491–496
Young E, Regan C, Currier BL, Yaszemski MJ, Larson AN (2022) At mean 30-year follow-up, cervical spine disease is common and associated with thoracic hypokyphosis after pediatric treatment of adolescent idiopathic scoliosis. J Clin Med 11(20)
Abelin-Genevois K, Sassi D, Verdun S, Roussouly P (2018) Sagittal classification in adolescent idiopathic scoliosis: original description and therapeutic implications. Eur Spine J 27(9):2192–2202
Abelin-Genevois K, Estivalezes E, Briot J, Sevely A, de Gauzy JS, Swider P (2015) Spino-pelvic alignment influences disc hydration properties after AIS surgery: a prospective MRI-based study. Eur Spine J 24(6):1183–1190
Post M, Verdun S, Roussouly P, Abelin-Genevois K (2019) New sagittal classification of AIS: validation by 3D characterization. Eur Spine J 28(3):551–558
Lowenstein JE, Matsumoto H, Vitale MG, Weidenbaum M, Gomez JA, Lee FY et al (2007) Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine (Phila Pa 1976) 32(4):448–452
Newton PO, Yaszay B, Upasani VV, Pawelek JB, Bastrom TP, Lenke LG et al (2010) Preservation of thoracic kyphosis is critical to maintain lumbar lordosis in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 35(14):1365–1370
Watanabe K, Nakamura T, Iwanami A, Hosogane N, Tsuji T, Ishii K et al (2012) Vertebral derotation in adolescent idiopathic scoliosis causes hypokyphosis of the thoracic spine. BMC Musculoskelet Disord 13:99
Ries Z, Harpole B, Graves C, Gnanapragasam G, Larson N, Weintstein S et al (2015) Selective thoracic fusion of lenke I and II curves affects sagittal profiles but not sagittal or spinopelvic alignment: a case-control study. Spine (Phila Pa 1976) 40(12):926–934
Fletcher ND, Hopkins J, McClung A, Browne R, Sucato DJ (2012) Residual thoracic hypokyphosis after posterior spinal fusion and instrumentation in adolescent idiopathic scoliosis: risk factors and clinical ramifications. Spine (Phila Pa 1976) 37(3):200–206
Monazzam S, Newton PO, Bastrom TP, Yaszay B (2013) Multicenter Comparison Of The Factors Important In Restoring Thoracic Kyphosis During Posterior Instrumentation For Adolescent Idiopathic Scoliosis. Spine Deform 1(5):359–364
Luo M, Jiang H, Wang W, Li N, Shen M, Li P et al (2017) Influence of screw density on thoracic kyphosis restoration in hypokyphotic adolescent idiopathic scoliosis. BMC Musculoskelet Disord 18(1):526
Ohrt-Nissen S, Luk KDK, Samartzis D, Cheung JPY (2020) Selection of the lowest instrumented vertebra in main thoracic adolescent idiopathic scoliosis: Is it safe to fuse shorter than the last touched vertebra? Eur Spine J 29(8):2018–2024
Pankowski R, Roclawski M, Ceynowa M, Mikulicz M, Mazurek T, Kloc W (2016) Direct vertebral rotation versus single concave rod rotation: low-dose intraoperative computed tomography evaluation of spine derotation in adolescent idiopathic scoliosis surgery. Spine (Phila Pa 1976) 41(10):864–871
Larson AN, Aubin CE, Polly DW Jr, Ledonio CG, Lonner BS, Shah SA et al (2013) Are more screws better? A systematic review of anchor density and curve correction in adolescent idiopathic scoliosis. Spine Deform 1(4):237–247
Yang S, Jones-Quaidoo SM, Eager M, Griffin JW, Reddi V, Novicoff W et al (2011) Right adolescent idiopathic thoracic curve (Lenke 1 A and B): does cost of instrumentation and implant density improve radiographic and cosmetic parameters? Eur Spine J 20(7):1039–1047
Sudo H, Abe Y, Kokabu T, Ito M, Abumi K, Ito YM et al (2016) Correlation analysis between change in thoracic kyphosis and multilevel facetectomy and screw density in main thoracic adolescent idiopathic scoliosis surgery. Spine J 16(9):1049–1054
Ilharreborde B (2018) Sagittal balance and idiopathic scoliosis: does final sagittal alignment influence outcomes, degeneration rate or failure rate? Eur Spine J 27(Suppl 1):48–58
Ilharreborde B, Pesenti S, Ferrero E, Accadbled F, Jouve JL, De Gauzy JS et al (2018) Correction of hypokyphosis in thoracic adolescent idiopathic scoliosis using sublaminar bands: a 3D multicenter study. Eur Spine J 27(2):350–357
Allia J, Clement JL, Rampal V, Leloutre B, Rosello O, Solla F (2018) Influence of derotation connectors on 3d surgical correction of adolescent idiopathic scoliosis. Clin Spine Surg 31(3):E209–E215
Aubin CE, Labelle H, Ciolofan OC (2007) Variability of spinal instrumentation configurations in adolescent idiopathic scoliosis. Eur Spine J 16(1):57–64
Angelliaume A, Ferrero E, Mazda K, Le Hanneur M, Accabled F, de Gauzy JS et al (2017) Titanium vs cobalt chromium: what is the best rod material to enhance adolescent idiopathic scoliosis correction with sublaminar bands? Eur Spine J 26(6):1732–1738
Giudici F, Galbusera F, Zagra A, Wilke HJ, Archetti M, Scaramuzzo L (2017) Determinants of the biomechanical and radiological outcome of surgical correction of adolescent idiopathic scoliosis surgery: the role of rod properties and patient characteristics. Eur Spine J 26(Suppl 4):524–532
Sullivan TB, Bastrom TP, Bartley CE, Dolan LA, Weinstein SL, Newton PO (2020) More severe thoracic idiopathic scoliosis is associated with a greater three-dimensional loss of thoracic kyphosis. Spine Deform 8(6):1205–1211
Parvaresh KC, Osborn EJ, Reighard FG, Doan J, Bastrom TP, Newton PO (2017) Predicting 3D thoracic kyphosis using traditional 2D radiographic measurements in adolescent idiopathic scoliosis. Spine Deform 5(3):159–165
Shen J, Parent S, Wu J, Aubin CE, Mac-Thiong JM, Kadoury S et al (2020) Towards a new 3D classification for adolescent idiopathic scoliosis. Spine Deform 8(3):387–396
Newton PO, Osborn EJ, Bastrom TP, Doan JD, Reighard FG (2019) The 3D sagittal profile of thoracic versus lumbar major curves in adolescent idiopathic scoliosis. Spine Deform 7(1):60–65
Pasha S, Cahill PJ, Dormans JP, Flynn JM (2016) Characterizing the differences between the 2D and 3D measurements of spine in adolescent idiopathic scoliosis. Eur Spine J 25(10):3137–3145
Machida M, Rocos B, Zabjek K, Lebel DE (2022) A comparison of the reliability and vulnerability of 3D sterEOS and 2D EOS when measuring the sagittal spinal alignment of patients with adolescent idiopathic scoliosis. Spine Deform 10(5):1029–1034
Illes T, Somoskeoy S (2013) Comparison of scoliosis measurements based on three-dimensional vertebra vectors and conventional two-dimensional measurements: advantages in evaluation of prognosis and surgical results. Eur Spine J 22(6):1255–1263
Hayashi K, Upasani VV, Pawelek JB, Aubin CE, Labelle H, Lenke LG et al (2009) Three-dimensional analysis of thoracic apical sagittal alignment in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 34(8):792–797
Boyer L, Shen J, Parent S, Kadoury S, Aubin CE (2018) Accuracy and precision of seven radiography-based measurement methods of vertebral axial rotation in adolescent idiopathic scoliosis. Spine Deform 6(4):351–357
Drerup B (1984) Principles of measurement of vertebral rotation from frontal projections of the pedicles. J Biomech 17(12):923–935
Le Naveaux F, Aubin CE, Parent S, ON P, Labelle H (2017) 3D rod shape changes in adolescent idiopathic scoliosis instrumentation: how much does it impact correction. Eur Spine J 26(6):1676–1683
Pasha S, Flynn J (2018) Data-driven classification of the 3D spinal curve in adolescent idiopathic scoliosis with an applications in surgical outcome prediction. Sci Rep 8(1):16296
Bao HD, Shu SB, Shi J, Liu SN, Sun MH, Hu AN et al (2018) Similar coronal curvature may not represent the same 3-dimensional deformity in adolescent idiopathic scoliosis: a matched-pair study using EOS imaging system. Zhonghua Yi Xue Za Zhi 98(21):1691–1696
Dubousset J, Ilharreborde B, Le Huec JC (2014) Use of EOS imaging for the assessment of scoliosis deformities: application to postoperative 3D quantitative analysis of the trunk. Eur Spine J 23:397–405
Ferrero E, Mazda K, Simon AL, Ilharreborde B (2018) Preliminary experience with SpineEOS, a new software for 3D planning in AIS surgery. Eur Spine J 27(9):2165–2174
Ilharreborde B, Dubousset J, Le Huec JC (2014) Use of EOS imaging for the assessment of scoliosis deformities: application to postoperative 3D quantitative analysis of the trunk. Eur Spine J 23(Suppl 4):S397–S405
Lebel DE, Al-Aubaidi Z, Shin EJ, Howard A, Zeller R (2013) Three dimensional analysis of brace biomechanical efficacy for patients with AIS. Eur Spine J 22(11):2445–2448
Peeters CMM, Bos G, Kempen DHR, Jutte PC, Faber C, Wapstra FH (2022) Assessment of spine length in scoliosis patients using EOS imaging: a validity and reliability study. Eur Spine J
Zhang X, Yang D, Zhang S, Wang J, Chen Y, Dou X et al (2022) Do the three-dimensional parameters of brace-wearing patients with AIS change when transitioning from standing to sitting position? A preliminary study on Lenke I. BMC Musculoskelet Disord 23(1):419
Kuklo TR, Potter BK, Lenke LG (2005) Vertebral rotation and thoracic torsion in adolescent idiopathic scoliosis: what is the best radiographic correlate? J Spinal Disord Tech 18(2):139–147
Shen J, Kadoury S, Labelle H, Parent S (2016) Geometric torsion in adolescent idiopathic scoliosis: a surgical outcomes study of lenke type 1 patients. Spine (Phila Pa 1976) 41(24):1903–1907
Pasha S, Shen J, Kadoury S (2021) True 3D parameters of the spinal deformity in adolescent idiopathic scoliosis. Spine Deform 9(3):703–710
Atmaca H, Inanmaz ME, Bal E, Caliskan I, Kose KC (2014) Axial plane analysis of Lenke 1A adolescent idiopathic scoliosis as an aid to identify curve characteristics. Spine J 14(10):2425–2433
Atmaca H, Inanmaz ME, Bal E, Caliskan I, Kose KC (2014) Axial plane analysis of Lenke 1A adolescent idiopathic scoliosis as an aid to identify curve characteristics. Spine J Official J North Am Spine Soc 14(10):2425–2433
Wu HD, Wong MS (2020) Assessment of maximum spinal deformity in scoliosis: a literature review. J Med Biol Eng 40(5):621–629
Wan ST, S.; Wong, D.; Zhang, T.; Cheung, JPY (2022) Patient and surgical predictors of 3D correction in posterior spinal fusion: a systematic review
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Floccari LV, Poppino K, Greenhill DA, Sucato DJ (2021) Ponte osteotomies in a matched series of large AIS curves increase surgical risk without improving outcomes. Spine Deform 9(5):1411–1418
Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C (2013) Assessing bias in studies of prognostic factors. Ann Intern Med 158(4):280–286
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650):924
Pasha S, Shah S, Yaszay B, Newton P (2021) Discovering the association between the pre- and post-operative 3D spinal curve patterns in adolescent idiopathic scoliosis. Spine Deform 9(4):1053–1062
Pasha S, Shah S, Newton P, Harms study G (2021) Machine learning predicts the 3D outcomes of adolescent idiopathic scoliosis surgery using patient-surgeon specific parameters. Spine 46(9):579–587
Yeung KH, Man GCW, Skalli W, Hu Z, Hung VWY, Hung ALH et al (2021) Global sagittal alignment after surgery of right thoracic idiopathic scoliosis in adolescents and adults with and without thoracic hypokyphosis. Sci Rep 11(1):6294
Shen J, Kadoury S, Labelle H, Parent S (2016) Geometric Torsion in Adolescent Idiopathic Scoliosis: A Surgical Outcomes Study of Lenke Type 1 Patients. Spine 41(24):1903–1907
Machida M, Rocos B, Lebel DE, Zeller R (2022) Increased proximal vertebral rotation is associated with shoulder imbalance after posterior spinal fusion for severe adolescent idiopathic scoliosis. Spine Deform 10(5):1149–1156
Sikora-Klak J, Upasani VV, Ilharreborde B, Cross M, Bastrom TP, Mazda K et al (2021) Three-dimensional analysis of spinal deformity correction in adolescent idiopathic scoliosis: comparison of two distinct techniques. Childs Nerv Syst 37(2):555–560
Kato S, Debaud C, Zeller RD (2017) Three-dimensional EOS analysis of apical vertebral rotation in adolescent idiopathic scoliosis. J Pediatr Orthop 37(8):e543–e547
Pasha S, Baldwin K (2019) Surgical outcome differences between the 3D subtypes of right thoracic adolescent idiopathic scoliosis. Eur Spine J 28(12):3076–3084
Homans JF, Kruyt MC, Schlösser TPC, Colo D, Rogers K, Shah SA et al (2020) Changes in the position of the junctional vertebrae after posterior spinal fusion in adolescent idiopathic scoliosis: implication in risk assessment of proximal junctional kyphosis development. J Pediatr Orthop 40(2):e84–e90
Pasha S, Flynn JM, Sankar WN (2018) Outcomes of selective thoracic fusion for Lenke 1 adolescent idiopathic scoliosis: predictors of success from the sagittal plane. Eur Spine J 27(9):2223–2232
Le Navéaux F, Aubin CE, Parent S, ON P, Labelle H (2017) 3D rod shape changes in adolescent idiopathic scoliosis instrumentation: how much does it impact correction. Eur Spine J 26(6):1676–1683
Ilharreborde B, Simon AL, Ferrero E, Mazda K (2019) How to Optimize axial correction without altering thoracic sagittal alignment in hybrid constructs with sublaminar bands: description of the “frame” technique. Spine Deform 7(2):245–253
Newton PO, Wu KW, Bastrom TP, Bartley CE, Upasani VV, Yaszay B (2019) What factors are associated with kyphosis restoration in lordotic adolescent idiopathic scoliosis patients? Spine Deform 7(4):596–601
Le Naveaux F, Aubin CE, Parent S, Newton PO, Labelle H (2017) 3D rod shape changes in adolescent idiopathic scoliosis instrumentation: how much does it impact correction? Eur Spine J 26(6):1676–1683
Kluck D, Newton PO, Sullivan TB, Yaszay B, Jeffords M, Bastrom TP et al (2020) A 3D parameter can guide concave rod contour for the correction of hypokyphosis in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 45(19):E1264–E1271
Pasha S, Shah S, Yaszay B, Newton P, Harms Study G (2021) Discovering the association between the pre- and post-operative 3D spinal curve patterns in adolescent idiopathic scoliosis. Spine Deform 9(4):1053–1062
Suk SI, Lee SM, Chung ER, Kim JH, Kim WJ, Sohn HM (2003) Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 28(5):484–491
Erdemir C, Musaoğlu R, Selek Ö, Gök Ü, Şarlak AY (2015) Distal fusion level selection in Lenke 1A curves according to axial plane analyses. Spine J 15(11):2378–2384
Potter BK, Rosner MK, Lehman RA Jr, Polly DW Jr, Schroeder TM, Kuklo TR (2005) Reliability of end, neutral, and stable vertebrae identification in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 30(14):1658–1663
Vidal C, Mazda K, Ilharreborde B (2016) Sagittal spino-pelvic adjustment in severe Lenke 1 hypokyphotic adolescent idiopathic scoliosis patients. Eur Spine J 25(10):3162–3169
Pasha S, Shah S, Newton P (2021) Machine Learning Predicts the 3D Outcomes of Adolescent Idiopathic Scoliosis Surgery Using Patient-Surgeon Specific Parameters. Spine 46(9):579–587
Clément JL, Geoffray A, Yagoubi F, Chau E, Solla F, Oborocianu I et al (2013) Relationship between thoracic hypokyphosis, lumbar lordosis and sagittal pelvic parameters in adolescent idiopathic scoliosis. Eur Spine J 22(11):2414–2420
Legarreta CA, Barrios C, Rositto GE, Reviriego JM, Maruenda JI, Escalada MN et al (2014) Cervical and thoracic sagittal misalignment after surgery for adolescent idiopathic scoliosis: a comparative study of all pedicle screws versus hybrid instrumentation. Spine (Phila Pa 1976) 39(16):1330–1337
King HA, Moe JH, Bradford DS, Winter RB (1983) The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am 65(9):1302–1313
Kim SS, Kim JH, Suk SI (2017) Effect of Direct Vertebral Rotation on the Uninstrumented Lumbar Curve in Thoracic Adolescent Idiopathic Scoliosis. Asian Spine J 11(1):127–137
Chang DG, Suk SI, Kim JH, Song KS, Suh SW, Kim SY et al (2020) Long-term outcome of selective thoracic fusion using rod derotation and direct vertebral rotation in the treatment of thoracic adolescent idiopathic scoliosis: more than 10-year follow-up data. Clin Spine Surg 33(2):E50–E57
Zuckerman SL, Segar AH, Cerpa M, Chanbour H, Sardar ZM, Lenke LG (2022) Three-dimensional assessment of vertebral derotation in adolescent idiopathic scoliosis: review of a surgical technique and its success in achieving derotation in the instrumented and uninstrumented spine. Oper Neurosurg (Hagerstown) 22(6):380–386
Alzakri A, Vergari C, Van den Abbeele M, Gille O, Skalli W, Obeid I (2019) Global sagittal alignment and proximal junctional kyphosis in adolescent idiopathic scoliosis. Spine Deform 7(2):236–244
Kim YJ, Lenke LG, Bridwell KH, Kim J, Cho SK, Cheh G et al (2007) Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 32(24):2731–2738
Cidambi KR, Glaser DA, Bastrom TP, Nunn TN, Ono T, Newton PO (2012) Postoperative changes in spinal rod contour in adolescent idiopathic scoliosis: an in vivo deformation study. Spine (Phila Pa 1976) 37(18):1566–1572
Seki S, Kawaguchi Y, Nakano M, Makino H, Mine H, Kimura T (2016) Rod rotation and differential rod contouring followed by direct vertebral rotation for treatment of adolescent idiopathic scoliosis: effect on thoracic and thoracolumbar or lumbar curves assessed with intraoperative computed tomography. Spine J 16(3):365–371
Lamerain M, Bachy M, Delpont M, Kabbaj R, Mary P, Vialle R (2014) CoCr rods provide better frontal correction of adolescent idiopathic scoliosis treated by all-pedicle screw fixation. Eur Spine J 23(6):1190–1196
Okada E, Watanabe K, Hosogane N, Shiono Y, Takahashi Y, Nishiwaki Y et al (2013) Comparison of stainless steel and titanium alloy instruments in posterior correction and fusion surgery for adolescent idiopathic scoliosis-prospective cohort study with minimum 2-year follow-up. J Med Biol Eng 33(3):325–329
Bowden D, Michielli A, Merrill M, Will S (2022) Systematic review and meta-analysis for the impact of rod materials and sizes in the surgical treatment of adolescent idiopathic scoliosis. Spine Deform 10(6):1245–1263
Samdani AF, Bennett JT, Singla AR, Marks MC, Pahys JM, Lonner BS et al (2015) Do ponte osteotomies enhance correction in adolescent idiopathic scoliosis? An analysis of 191 Lenke 1A and 1B curves. Spine Deform 3(5):483–488
Pizones J, Izquierdo E, Sánchez-Mariscal F, Alvarez P, Zúñiga L, Gómez A (2010) Does wide posterior multiple level release improve the correction of adolescent idiopathic scoliosis curves? J Spinal Disord Tech 23(7):e24–e30
Shah SA, Dhawale AA, Oda JE, Yorgova P, Neiss GI, Holmes L Jr et al (2013) Ponte osteotomies with pedicle screw instrumentation in the treatment of adolescent idiopathic scoliosis. Spine Deform 1(3):196–204
Halanski MA, Cassidy JA (2013) Do multilevel Ponte osteotomies in thoracic idiopathic scoliosis surgery improve curve correction and restore thoracic kyphosis? J Spinal Disord Tech 26(5):252–255
Abousamra O, Sponseller PD, Lonner BS, Shah SA, Marks MC, Cahill PJ et al (2019) Thoracic Lordosis, especially in males, increases blood loss in adolescent idiopathic scoliosis. J Pediatr Orthop 39(3):e201–e204
Buckland AJ, Moon JY, Betz RR, Lonner BS, Newton PO, Shufflebarger HL et al (2019) Ponte osteotomies increase the risk of neuromonitoring alerts in adolescent idiopathic scoliosis correction surgery. Spine (Phila Pa 1976) 44(3):E175–E180
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wan, S.HT., Wong, D.LL., To, S.CH. et al. Patient and surgical predictors of 3D correction in posterior spinal fusion: a systematic review. Eur Spine J 32, 1927–1946 (2023). https://doi.org/10.1007/s00586-023-07708-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07708-2