Abstract
Purpose
In 2017, the GAP score was proposed as a tool to reduce mechanical complications (MC) in adult spinal deformity (ASD) surgery: the reported MC rate for the GAP proportioned category was only 6%, which is clearly lower to the MC rate reported in the literature. The aim of this study is to analyse if the most recent literature confirms the promising results of the original article.
Materials and methods
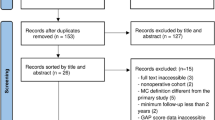
Using the PRISMA flow chart, we reviewed the literature to analyse GAP score capacity in predicting MC occurrence. We included articles clearly reporting ASD surgery MC stratified by GAP categories and the score’s overall capacity to predict MC using the area under the curve (AUC). The quality of the included studies was evaluated using GRADE and MINORS systems.
Results
Eleven retrospective articles (1,517 patients in total) were included. The MC distribution per GAP category was as follows: GAP-P, 32.8%; GAP-MD, 42.3%; GAP-SD, 55.4%. No statistically significant difference was observed between the different categories using the Kruskal–Wallis test (p = 0.08) and the two-by-two Pearson-Chi square test (P Vs MD, p = 0.300; P Vs SD, p = 0.275; MD Vs SD, p = 0.137). The global AUC was 0.68 ± 0.2 (moderate accuracy). The included studies were of poor quality according to the GRADE system and had a high risk of bias based on the MINORS criteria.
Conclusion
The actual literature does not corroborate the excellent results reported by the original GAP score article. Further prospective studies, possibly stratified by type of MC and type of surgery, are necessary to validate this score.


Similar content being viewed by others
References
Lord EL, Ayres E, Woo D, Vasquez-Montes D, Parekh Y, Jain D, Buckland A, Protopsaltis T (2021) The impact of global alignment and proportion score and bracing of proximal junctional kyphosis in adult spinal deformity. Global Spine J 12:219. https://doi.org/10.1177/21925682211001812
Smith JS, Shaffrey CI, Ames CP, Lenke LG (2019) Treatment of adult thoracolumbar spinal deformity: past, present and future. J Neurosurg Spine 30(5):551–567. https://doi.org/10.3171/2019.1.SPINE181494
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine 30(18):2024–2029. https://doi.org/10.1097/01.brs.0000179086.30449.96
Fehlings MG, Tetreault L, Nater A et al (2015) The Aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery 77(Suppl4):S1–S5. https://doi.org/10.1227/NEU.0000000000000953
Ames CP, Scheer JK, Lafage V, Smith JS, Bess S, Berven SH, Mundis GM, Sethi RK, Deinlein DA, Coe JD, Hey LA, Daubs MD (2016) Adult spinal deformity: epidemiology, health impact, evaluation and management. Spine Deform 4:310–322. https://doi.org/10.1016/j.jspd.2015.12.009
Zanirato A, Damilano M, Formica M, Piazzolla A, Lovi A, Villafane JH, Berjano P (2018) Complications in adult spine deformity surgery: a systematic review of the recent literature reporting aggregated incidences. Eur Spine J 27(9):2272–2284. https://doi.org/10.1007/s00586-018-5535-y
Formica M, Cavagnaro L, Zanirato A, Felli L, Formica C (2016) Proximal junctional spondylodiscitis after pedicle subtraction osteotomy. Spine J 16(2):e49-51. https://doi.org/10.1016/j.spinee.2015.09.050
Bridwell KH, Glassman S, Horton W et al (2009) Does treatment (non-operative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine 34(20):2171–2178. https://doi.org/10.1097/BRS.0b013e3181a8fdc8
Smith JS, Lafage V, Shaffrey CI et al (2016) Outcomes of operative and nonoperative treatment for adult spinal deformity: a prospective, multicenter, propensity-matched cohort assessment with minimum 2-year follow-up. Neurosurgery 78(6):851–861. https://doi.org/10.1227/NEU.0000000000001116
Formica M, Quarto E, Zanirato A, Mosconi L, Lontaro-Baracchini M, Alessio-Mazzola M, Felli L (2021) ALIF in the correction of spinal sagittal misalignment: a systematic review of literature. Eur Spine J 30(1):50–62. https://doi.org/10.1007/s00586-020-06598-y
Quarto E, Zanirato A, Ursino C, Traverso G, Russo A, Formica M (2021) Adult spinal deformity surgery: posterior three-column osteotomies vs anterior lordotic cages with posterior fusion. Complications, clinical and radiological results. A systematic review of the literature. Eur Spine J 30(11):3150–3161. https://doi.org/10.1007/s00586-021-06925-x
Roussouly P, Pinheiro-Franco JL (2011) Sagittal parameters of the spine: biomechanical approach. Eur Spine J 20(Suppl 5):S578–S585. https://doi.org/10.1007/s00586-011-1924-1
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis research society – Schwab adult spinal deformity classification: a validation study. Spine 37(12):1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine. Eur Spine J 28(9):1889–1905. https://doi.org/10.1007/s00586-019-06083-1
Le Huec JC, Hasegawa K (2016) Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and Japanese subjects. Eur Spine J 25(11):3630–3637. https://doi.org/10.1007/s00586-016-4485-5
Sebaaly A, Gehrchen M, Silvestre C, Kharrat K, Bari TJ, Kreichati G, Rizkallah M, Roussouly P (2020) Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classifcation: a multicentric study. Eur spine J: Publ Eur Spine Soc, Eur Spin Deform Soc Eur Sec Cerv Spine Res Soc 29:904–913. https://doi.org/10.1007/s00586-019-06253-1
Baum GR, Ha AS, Cerpa M, Zuckerman SL, Lin JD, Menger RP, Osorio JA, Morr S, Leung E, Lehman RA, Sardar Z, Lenke LG (2020) Does the global alignment and proportion score overestimate mechanical complications after adult spinal deformity correction? J Neurosurg Spine 34(1):1–7. https://doi.org/10.3171/2020.6.Spine20538
Kawabata A, Yoshii T, Sakai K, Hirai T, Yuasa M, Inose H, Utagawa K, Hashimoto J, Matsukura Y, Tomori M, Torigoe I, Kusano K, Otani K, Mizuno K, Satoshi S, Kazuyuki F, Tomizawa S, Arai Y, Shindo S, Okawa A (2020) Identifcation of predictive factors for mechanical complications after adult spinal deformity surgery: a multi-institutional retrospective study. Spine 45:1185–1192. https://doi.org/10.1097/brs.0000000000003500
Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstück F, Pérez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99:1661–1672. https://doi.org/10.2106/jbjs.16.01594
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J (2019) Updated guidance for trusted systematic reviews a new edition of the cochrane handbook for systematic reviews of interventions.Cochrane Database. Syst Rev 10:142. Doi: https://doi.org/10.1002/14651858.ED000142;
Moher D, Liberati A, Tetzlaf J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
OCEBM Levels of Evidence Working Group*. “The Oxford Levels of Evidence 2”. Oxford Centre for Evidence-Based Medicine. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ ocebm-levels-of-evidence
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, AlonsoCoello P, Schünemann HJ (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Bari TJ, Ohrt-Nissen S, Hansen LV, Dahl B, Gehrchen M (2019) Ability of the global alignment and proportion score to predict mechanical failure following adult spinal deformity surgery – validation in 149 patients with two-year follow-up. Spine Deform 7(2):331–337. https://doi.org/10.1016/j.jspd.2018.08.002
Jacobs E, Van Royen BJ, Van Kujik SMJ, Merk JMR, Stadhouder A, Van Rhijn LW, Willems PC (2019) Prediction of mechanical complications in adult spinal deformity surgery-the GAP score versus the Schwab classification. Spine J 19(5):781–788. https://doi.org/10.1016/j.spinee.2018.11.013
Gupta MC, Yilgor C, Moon HJ, Lertudomphonwanit T, Alanay A, Lenke L, Bridwell KH (2021) Evaluation of global alignment and proportion score in an independent database. Spine J 21(9):1549–1558. https://doi.org/10.1016/j.spinee.2021.04.004
Kwan KYH, Lenke LG, Shaffrey CI, Carreon LY, Dahl BT, Fehlings MG et al (2021) Are higher global alignment and proportion scores associated with increased risks of mechanical complications after adult spinal deformity surgery ? An external validation. Clin Orthop Relat Res 479(2):312–320. https://doi.org/10.1097/CORR.0000000000001521
Ham DW, Kim HJ, Choi JH, Park J, Lee J, Yeom JS (2021) Validity of the global alignment proportion (GAP) score in predicting mechanical complications after adult spinal deformity surgery in elderly patiens. Eur Spine J 30(5):1190–1198. https://doi.org/10.1007/s00586-021-06734-2
Sun X, Sun W, Sun S, Hu H, Zhang S, Kong C, Lu S (2021) Which sagittal evaluation system can effectively predict mechanical complications in the treatment of elderly patients with adult degenerative scoliosis ? Roussouly classification or Global Alignment and Proportion (GAP) Score. J Orthop Surg Res 16(1):641. https://doi.org/10.1186/s13018-021-02786-8
Yagi M, Daimon K, Hosogane N, Okada E, Suzuki S, Tsuji O et al (2021) Predictive probability of the global alignment and proportion score for the development of mechanical failure following adult spinal deformity surgery in Asian patients. Spine Spine (Phila Pa 1976) 46(2):80–86. https://doi.org/10.1097/BRS.0000000000003738
Teles AR, Aldebeyan S, Aoude A, Swamy G, Nicholls FH, Thomas KC, Jacobs WB (2022) Mechanical complications in adult spinal deformity surgery : can spinal alignment explain everything ? Spine Spine (Phila Pa 1976) 47(1):1–9. https://doi.org/10.1097/BRS.0000000000004217
Akobeng AK (2007) Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr 96(5):644–647. https://doi.org/10.1111/j.1651-2227.2006.00178.x
Dubousset J (1994) Three-dimensional analysis of the scoliotic deformity. In: Weinstein S (ed) The pediatric spine: principles and practice. Raven Press, pp 479–496
Amabile C, Le Huec JC, Skalli W (2016) Invariance of head-pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years. Eur Spine J 27(2):458–466. https://doi.org/10.1007/s00586-016-4830-8
Le Huec JC, Richards J, Tsoupras A, Price R, Leglise A, Faundez AA (2018) The mechanism in junctional failure of thoraco-lumbar fusion. Part I: Biomechanical analysis of mechanism responsible of vertebral overstress and description of the cervical inclination angle (CIA). Eur Spine J 27(Suppl 1):129–138. https://doi.org/10.1007/s00586-017-5425-8
Faundez AA, Richards J, Maxy Price R, Leglise A, Le Huec JC (2018) The mechanism in junctional failure of thoraco-lumbar fusions. Part II: Analysis of a series of PJK after thoraco-lumbar fusion to determine parameters allowing to predict the risk of junctional breakdown. Eur Spine J 27(Suppl 1):139–148. https://doi.org/10.1007/s00586-017-5426-7
Lafage R, Schwab F, Challier V, Henry KJ, Gum J, Smith J et al (2016) Defining spino-pelvic alignment thresholds. should operative goals in adult spinal deformity surgery account fo age? Spine 41(1):62–68. https://doi.org/10.1097/BRS.0000000000001171
Lafage R, Smith JS, Elysee J, Passias P, Bess S, Klineberg E et al (2022) Sagittal age-adjusted score (SAAS) for adult spinal deformity (ASD) more effectively predicts surgical outcomes and proximal junctional kyphosis than previous classifications. Spine Deformity 10(1):121–131. https://doi.org/10.1007/s43390-021-00397-1
Jalai CM, Cruz DL, Diebo BG, Poorman G, Lafage R, Bess S et al (2017) Full-body analysis of age-adjusted alignment in adult spinal deformity patients and lower-limb compensation. Spine (Phila Pa 1976) 42(9):653–661. https://doi.org/10.1097/BRS.0000000000001863
Iyer S, Lenke LG, Nemani VM, Fu M, Shifflett GD, Albert TJ, Sides BA, Metz LN, Cunningham ME, Kim HJ (2016) Variations in occipitocervical and cervicothoracic alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976) 41(23):1837–1844. https://doi.org/10.1097/BRS.0000000000001644
Iyer S, Lenke LG, Nemani VM, Albert TJ, Sides BA, Metz LN, Cunningham ME, Kim HJ (2016) Variations in sagittal alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976) 41(23):1826–1836. https://doi.org/10.1097/BRS.0000000000001642
Kim HJ, Bridwell KH, Lenke LG, Park MS, Song KS, Piyaskulkaew C, Chuntarapas T (2014) Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976) 39(9):576–580. https://doi.org/10.1097/BRS.0000000000000246
Le Huec JC, Charosky S, Barrey C, Rigal J, Anouble S (2011) Sagittal imbalance cascade for simple degenerative spine and consequences: algorithm of decision for appropriate treatment. Eur Spine J 20(Suppl 5):S699–S703. https://doi.org/10.1007/s00586-011-1938-8
Dial BL, Hills JM, Smith JS, Sardi JP, Lazaro B, Shaffery CI et al (2022) The impact of lumbar alignment targerts on mechanical complications after adult lumbar scoliosis surgery. Eur Spine J. https://doi.org/10.1007/s00586-022-07200-3
Duan PG, Mummaneni PV, Rivera J, Guin JM, Wang M, Xi Z et al (2020) The association between lower Hounsfield units in the upper instrumented vertebra and proximal junctional kyphosis in adult spinal deformity surgery with a minimum 2-year follow-up. Neurosurg Focus 49(2):E7. https://doi.org/10.3171/2020.5.FOCUS20192
Kim HJ, Dash A, Cunningham M, Schwab F, Dowdell J, Harrison J et al (2021) Patients with abnormal microarchitecture have an increased risk of early complications after spinal fusion surgery. Bone 143:115731. https://doi.org/10.1016/j.bone.2020.115731
Jiang J, Teng Y, Fan Z, Khan S, Xia Y (2014) Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis Clin Orthop Relat Res 472(3):968–975. https://doi.org/10.1007/s11999-013-3346-3
Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR, Harrop J, Sharan A, Ratliff JK (2007) Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine 6(4):291–297. https://doi.org/10.3171/spi.2007.6.4.1
Yadla S, Malone J, Campbell PG, Maltenfort MG, Harrop JS, Sharan AD, Vaccaro AR, Ratliff JK (2010) Obesity and spine surgery: reassessment based on a prospective evaluation of perioperative complications in elective degenerative thoracolumbar procedures. Spine J 10(7):581–587. https://doi.org/10.1016/j.spinee.2010.03.001
Noh SH, Ha Y, Obeid I, Park JY, Kuh SU, Chin DK et al (2020) Modified global alignment and proportion scoring with body mass index and bone mineral density (GAPB) for improving predictions of mechanical complications after adult spinal deformity surgery. Spine J 20:776–784. https://doi.org/10.1016/j.spinee.2019.11.006
He K, Head J, Mouchtouris N, Hines K, Shea P, Shmidt R et al (2020) The implications of paraspinal muscle atrophy in low back pain, thoracolumbar pathology, and clinical outcomes after spine surgery: a review of the literature. Global Spine J 10(5):657–666. https://doi.org/10.1177/2192568219879087
Yagi M, Hosogane N, Watanabe K, Asazuma T, Matsumoto M (2016) The paravertebral muscle and psoas for the maintenance of global spinal alignment in patient with degenerative lumbar scoliosis. Spine J 16:451–458. https://doi.org/10.1016/j.spinee.2015.07.001
Choi MK, Kim SB, Park CK, Malla HP, Kim SM (2017) Cross-sectional area of the lumbar spine trunk muscle and posterior lumbar interbody fusion rate: a retrospective study. Clin Spine Surg 30:E798–E803. https://doi.org/10.1097/BSD.0000000000000424
Kim JY, Ryu DS, Paik HK et al (2016) Paraspinal muscle, facet joint, and disc problems: risk factors for adjacent segment degeneration after lumbar fusion. Spine J 16:867–875. https://doi.org/10.1016/j.spinee.2016.03.010
Yagi M, Michikawa T, Hosogane N, Fujita N, Okada E, Suzuki S et al (2019) The 5-Item modified frailty index is predictive of severe adverse events in patients undergoing surgery for adult spinal deformity. Spine 44:E1083-1091. https://doi.org/10.1097/BRS.0000000000003063
Yagi M, Michikawa T, Hosogane N, Fujita N, Okada E, Suzuki S et al (2018) Treatment of frailty does not improve complication rates in corrective surgery for adult spinal deformity. Spine 44(10):723–731. https://doi.org/10.1097/BRS.0000000000002929
Funding
No funding to declare.
Author information
Authors and Affiliations
Contributions
EQ and AZ, review, first draft, statistical analysis; MP, SV, FV and SB, data analysis and results writing; J-CLH and MF, final manuscript review and language editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
No ethical approval was needed for this review.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Quarto, E., Zanirato, A., Pellegrini, M. et al. GAP score potential in predicting post-operative spinal mechanical complications: a systematic review of the literature. Eur Spine J 31, 3286–3295 (2022). https://doi.org/10.1007/s00586-022-07386-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07386-6