Abstract
Purpose
Adult spinal deformity (ASD) surgery is prone to postoperative complications, leading to high reoperation rates. The global alignment and proportion (GAP) score is a novel method to predict mechanical complications (MC) based on the optimal parameters related to individual pelvic incidence. The aim of this study was to determine the cut-off point and the predictive value of the GAP score for those MCs that require reoperation. A secondary aim was to investigate the cumulative incidence of MCs requiring reoperation during a long follow-up period.
Methods
In total, 144 ASD patients were operated at our institution due to marked symptomatic spinal deformity between 2008 and 2020. The cut-off point and the predictive value of the GAP score for the MCs that required reoperation and the cumulative incidence of reoperated MCs after index surgery were determined.
Results
A total of 142 patients were included in the analysis. The risk for having an MC that required reoperation was significantly lower when the postoperative GAP score was < 5 (HR = 3.55, 95% CI: 1.40–9.02). The discriminative power of the GAP score to predict MCs that require reoperation was good with an AUC of 0.70 (95% CI: 0.58–0.81). The cumulative incidence of reoperated MCs was 18%.
Conclusion
The GAP score was associated with the risk for MCs that require reoperation. The best predictive value for surgically treated MC was with the GAP score \(\ge\) 5. The cumulative incidence of the reoperated MCs was 18%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult spinal deformity (ASD) surgery is prone to postoperative complications, leading to high reoperation rates [1,2,3,4,5,6]. Indeed, almost 20% of patients sustain a mechanical complication (MC) related to implants or bony structures, typically implant breakage or junctional failure, resulting in reoperation [1, 3,4,5,6]. Of all the primary complications leading to reoperation, MCs make up more than 60% [3,4,5, 7]. Although reoperations due to MCs have been shown to be cost-effective and sometimes less expensive than the index surgery itself, they still cause a significant economic burden on healthcare systems [8,9,10].
The primary aim of ASD correction surgery is to achieve a spinal alignment that does not require significant compensation mechanisms postoperatively and is economical to maintain when the patient is ambulatory [7, 11]. To achieve this goal, various classifications and scores have been developed [12, 13].
The Global Alignment and Proportion (GAP) score is a novel proportional model to predict all MCs [7]. The GAP score is based on a patient’s individual pelvic incidence. The premise is that not everyone benefits from the same radiological targets. According to the original validation study by Yilgor et al., the cut-off points of the GAP score were determined as follows: 0–2 to indicate a proportioned, 3–6 to indicate moderately disproportioned, and 6–13 to indicate severely disproportioned spinopelvic alignment [7]. The best predictive value for any MC was found with the GAP score ≥ 2 [7].
The aim of this study was to determine the cut-off point and the predictive value of the GAP score for those MCs requiring reoperation. A second aim was to investigate the cumulative incidence of the reoperated MCs during a long follow-up period.
Methods
The hypothesis of this study was that the GAP score is associated with the risk for MCs that require reoperation. The study was an analysis of prospectively collected data (diary number: 17U/2012). For the ASD patients who were operated at our institution Central Finland Central Hospital, Finland between 2008 and 2020, we used the following inclusion criteria: (1) patient age ≥ 18 years, (2) a minimum follow-up of two years, (3) a marked symptomatic sagittal spinal deformity (PI-LL > 10°, SVA > 5 cm and PT > 25°) and/or progressive symptomatic coronal thoracic or lumbar spinal deformity, and (4) the restoration of sagittal and coronal balance as to have the main indication for surgery. The exclusion criterion was the lack of standing full spine posterior-anterior and sagittal radiographs, which prevented the calculation of the GAP score.
Disability was assessed using the Oswestry Disability Index (ODI) and a separate Visual Analogue Scale (VAS) for leg pain (VAS-Leg) and back pain (VAS-Back) [14]. The severity of the deformity was assessed with the SRS-Schwab deformity classification [13].
The GAP score was measured and calculated from full spine standing posterior-anterior and sagittal radiographs taken preoperatively and at 0–3 months postoperatively. The GAP score was calculated using the following original formula: RPV + RLL + LDI + RSA + AF, where RPV is a relative pelvic version, RLL is a relative lumbar lordosis, LDI is a lordosis distribution index, and RSA is a relative spinopelvic alignment (Fig. 1) [7]. In the formula, AF indicates an age factor that is defined as an adult (< 60 years) or an older adult (≥ 60 years) [7].
MCs were evaluated from postoperative radiographs and patient records. As in the original validation study, proximal junctional failure (PJF) was defined as a fracture of the upper instrumented vertebra or one vertebra above, pullout of instrumentation at the upper instrumented vertebra, and/or sagittal subluxation [7]. Distal junctional failure (DJF) was defined as a fracture, implant pullout, or symptomatic ≥ 10° postoperative increase in kyphosis between the lowest instrumented vertebra and one vertebra below it. Proximal junctional kyphosis (PJK) was defined as over 10° increase of kyphotic angle between the lower endplate of the upper instrumented vertebra and the upper endplate of the second vertebra above during the follow-up without the need for surgery. PJK was not reported separately when a patient sustained a PJF leading to reoperation.
Statistical methods
The descriptive statistics are presented as means with standard deviation (SD), as medians with interquartile range, or counts with percentages. The relationship between the postoperative GAP score and the risk for MC requiring reoperation after ASD surgery was analyzed using generalized linear models. Receiver-operating characteristic (ROC) curves were used for the determination of thresholds for the MCs requiring reoperation. The diagnostic accuracy of the GAP score for MCs requiring reoperation was analyzed using the area under the curve (AUC), sensitivity, specificity, likelihood ratio, and positive predictive value. We defined the best cut-off point as the value with the highest accuracy that maximizes the Youden's index. Confidence intervals (95% CI) for the predictive values were obtained by bias-corrected and accelerated bootstrapping (10 000 replications). Cox proportional hazards regression was used to estimate the adjusted hazard ratios (HR) and their 95% confidence intervals. The relationship between the year of surgery and the operated MCs was analyzed using the Spearman's correlation test. Stata 17.0 (StataCorp LP, College Station, TX, USA) was used for the statistical analyses.
Results
Between 2008 and 2020, 144 ASD patients were operated to restore sagittal and coronal balance by three experienced spinal orthopedic surgeons at our hospital Central Finland Central Hospital, Finland. Two patients were excluded from the analysis because one was congenitally unable to stand and answer questionnaires and one patient died before postoperative radiographs were acquired.
Preoperative patient characteristics are described in Table 1. Of the 142 included patients, 96 (68%) were female. The mean (SD; range) age of the included patients was 65 (± 9; 22–81) years. The mean (SD; range) follow-up time for MCs was seven (± 3.3; 2–14) years. The mean (median; range) number of the fused levels was eight (nine; one to 16). In total, 57 (40%) patients had three column osteotomy (3CO), 62 (44%) had combined anterior interbody correction (ALIF) and posterior fusion, and 23 (16%) had posterior fusion and correction with multiple thoracolumbar Ponte osteotomies. Of the142 patients, 139 had posterior rods. In all posterior instrumentations, titanium alloy pedicle screws were used. The posterior rod material used was titanium alloy in 114 (82%) patients, cobalt-chrome in 24 (17%), and titanium-cobalt-chrome hybrid in one (1%). Two-rod construction was used in 90 (65%) patients, three longitudinal rods in 10 (7%), and four-rod constructs in 39 (28%). Three (2%) patients had anterior fixation or plating only associated with high angle (25–35°) anterior sagittal correction.
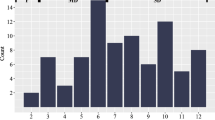
The mean (SD) GAP score was preoperatively 7.7 (± 3.7) and postoperatively 4.4 (± 3.3) (Fig. 2).
The optimal cut-off point to predict the risk for MCs that require reoperation was the GAP score ≥ 5. The discriminative power of the GAP score to predict MCs that require reoperation was good with an AUC of 0.70 (95% CI: 0.58 to 0.81) (Fig. 3).
The risk for MCs that require reoperation was significantly lower when the postoperative GAP score was < 5 (HR 3.55, 95% CI: 1.40–9.02, p = 0.008) adjusted with age, sex, body mass index, number of fused levels, and diagnosis of osteoporosis or neuromuscular disease (Fig. 4).
The total GAP score had a significant association with MCs that required reoperation (p = 0.003). The LDI (p = 0.002) and the RSA (p = 0.008) were the best parameters of the GAP score to predict MCs that require reoperation, while the RLL (p = 0.067), the RPV (p = 0.35), and the AF (p = 0.57) were the worst parameters to predict MCs that require reoperation (Fig. 5).
Postoperative GAP score and scoring subgroups adjusted with age, sex, body mass index (BMI), number of fused levels, and diagnosis of osteoporosis or neuromuscular disease. Statistically significant predictive value for rod breakage or proximal junctional failure was found in the GAP score, lordosis distribution index (LDI), and relative spinopelvic alignment (RSA). RPV relative pelvic version, RLL relative lumbar lordosis, AF age factor, < 60 or \(\ge\) 60 years, mechanical complications indicate those mechanical complications that required reoperation
Altogether, 23 (16%) patients sustained 26 MCs (cumulative incidence of 18%) that required reoperation because of a risk for instability or the patient's symptoms were associated with a MC seen on the radiograph (Table 2). Three patients (2%) were operated separately for two different complications, PJF and RB. Reoperated MCs included 11 (42%) PJFs, one (4%) DJF, and 14 (54%) RB. Mean (SD, range) time to reoperation was 14 (± 17, 0.5–48) months for junctional failure and 30 (30, six to 120) months for RB. Of the 26 reoperated MCs, 17 (65%) occurred more than six months after surgery. Of all patients, 24 (17%) had PJK ≥ 10° in their latest radiograph without major local symptoms, symptomatic loss of sagittal balance, or risk for instability and, therefore, were treated conservatively.
The number of the operated RBs (p < 0.001) and PJFs (p = 0.011) correlated with the year of surgery, with more incidents being in the earlier years of ASD surgery. The GAP score did not, however, correlate with the year of surgery (p = 0.239).
Discussion
The findings of this study confirm the association between the postoperative GAP score and MCs that require reoperation after ASD surgery. In the present patient cohort, the risk for sustaining an MC that requires reoperation was significantly higher when the postoperative GAP score was ≥ 5, indicating moderately disproportioned spinopelvic alignment. The cumulative incidence of MCs that required reoperation was 18%.
Several studies report conflicting results on the GAP score’s ability to predict MCs [15,16,17,18,19,20,21,22,23,24]. To our best knowledge, very few studies have specifically investigated the discriminatory power and threshold of the GAP score for those MCs that require reoperation. Yilgor et al. found that higher GAP scores were associated with higher rates of reoperated MCs [7]. Gupta et al. found the discriminative power of the GAP score increased as the years of follow-up increased [17]. Jacobs et al. reported a good ability of the GAP score to predict MCs [20]. Ham et al. investigated the accuracy of the GAP score to predict MCs specifically with patients with degenerative kyphoscoliosis [19]. In their study, the accuracy was lower when considering only those MCs that required reoperation, but moderate when considering all MCs [19].
Kwan et al., Bari et al., and Baum et al. reported the poor discriminatory power of the GAP score for both MCs and/ or reoperated MCs [15, 16, 24]. There were, however, differences in the studies, such as the length of the fusions, the rate of 3CO, and the age of the patients, which may explain the differences in the results compared to those in our study [15, 16, 24]. There was also variation in the studies as to whether neuromuscular diseases were included [7, 15,16,17, 19, 20, 24]. In our study, patients were not excluded based on the etiology of ASD. Therefore, the patient population was heterogeneous and included, for example, neuromuscular diseases and degenerative and post-traumatic spinal deformities, which may also explain the differences in the results.
In the present patient cohort, the LDI and the RSA were the best individual parameters of the GAP score to predict MCs that required reoperation, whereas the RLL, the RPV, and the AF were poorer in predicting operated MCs. To our knowledge, very few studies have assessed the predictive value of the GAP score parameters for MCs separately and the accuracy varied between studies [20, 21, 23, 25]. Indeed, the accuracy of the parameters for those MCs that require reoperation was not defined in the referenced studies.
Both Gupta et al. and Yilgor et al. defined the cut-off point of the GAP score for MCs to be ≥ 2 [7, 17]. The present study only included symptomatic and severe cases that required reoperation for MCs, whereas Yilgor et al. and Gupta et al. included all MCs [7, 17]. Therefore, the higher cut-off point in the present patient cohort is to be expected. Further, this suggests that patients in the present study tolerated greater disproportion before they sustained an MC and underwent reoperation. The patients in our study were also older compared to those in the studies of Yilgor et al. and Gupta et al. [7, 17]. Thus, it is possible that the patients in the present cohort had a lower level of physical demands and may, therefore, have had a lower risk for repetitive load leading to rod-related complications [7, 17].
Unfortunately, no surgical details were presented in the study by Yilgor et al., but the inclusion criterion was presented to be ≥ 4 levels of posterior instrumented fusion [7]. Therefore, it is not possible to compare whether the number of fused levels or other surgical methods could explain the differences in the cut-off levels. The study by Gupta et al. and the present study differed in, for example, the median length of fusion, the rate of 3COs, the rod constructs, and the rod materials used [17].
The other referenced studies focused mainly on assessing the accuracy of the GAP score for MCs and did not redefine the cut-off point [15, 16, 19, 20, 24]. However, as the reoperations after ASD surgery cause significant financial costs, it is important to recognize the threshold for severe MCs that require reoperation [8, 10]. Therefore, it would be useful for the surgeon in the planning of ASD surgery that the cut-off point of the GAP score for MCs had been evaluated between different groups. For example, according to the etiology of ASD or the surgical method used.
The cumulative incidence of the reoperated MCs in the present study is in line with previous studies [3,4,5, 7]. As the present study comprised only one DJF, the prediction analysis for DJF separately was not performed. Interestingly, the MCs correlated to the year of surgery, with surgery in the earlier years being more prone to MCs.
Our study confirms the validity of the GAP score in predicting MCs that require reoperation. The strength of this study is the relatively long follow-up time. To our best knowledge, there are very few long-term studies on the evaluation of the GAP score with more than five years of follow-up, as most studies meet a minimum follow-up period of two years [15, 16, 18,19,20,21,22,23]. In addition, we had an established clinical care team made up of highly experienced spine surgeons and nurses, and patient reachability for controls in the relatively stable catchment area was high. Furthermore, the large amount of prospectively collected data that extensively covered patient demographic data and exact time points as an example of MCs is a further strength of this study.
The limitations of this study are the relatively small number of patients and the heterogenous indications for ASD correction. In addition, the follow-up time of the patients who were operated in previous few years was uneven. Further, learning curve and the development of surgical techniques in ASD surgery may have biased the results, as those patients who underwent the most recent techniques tolerated a poor GAP score better. Also, the weakness of the study is that it does not take into account the effect of patient-reported outcome measurements (PROMs) on reoperations, although the decision to reoperation was made based on the patient's symptoms and radiographic MCs together. We are conducting another study where we evaluate PROMs and reoperations due to MCs among ASD patients. The predictability of clinical outcomes for reoperations due to MCs would also be worth of an investigation.
Conclusion
This study confirms the validity of the GAP score to predict MCs requiring reoperation after ASD surgery. The best predictive value for surgically treated MC was found with the GAP score \(\ge\) 5. The lordosis distribution index (LDI) and the relative spinopelvic alignment (RSA) were the best individual parameters of the GAP score to predict MCs. The cumulative percentage of surgically treated MCs was 18%. Bone-related MCs generally occurred earlier than implant-related MCs.
Data and materials availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request with a written request, from the institution’s patient records with signed GDPR and registry permissions.
References
Soroceanu A, Diebo BG, Burton D et al (2015) Radiographical and implant-related complications in adult spinal deformity surgery. Spine (Phila Pa 1976) 40:1414–1421. https://doi.org/10.1097/BRS.0000000000001020
Diebo BG, Shah NV, Boachie-Adjei OV et al (2019) Adult spinal deformity. The Lancet 394:160–172. https://doi.org/10.1016/S0140-6736(19)31125-0
Mok JM, Cloyd JM, Bradford DS et al (2009) Reoperation after primary fusion for adult spinal deformity. Spine (Phila Pa 1976) 34:832–839. https://doi.org/10.1097/BRS.0b013e31819f2080
Scheer JK, Tang JA, Smith JS et al (2013) Reoperation rates and impact on outcome in a large, prospective, multicenter, adult spinal deformity database. J Neurosurg Spine 19:464–470. https://doi.org/10.3171/2013.7.SPINE12901
Scheer JK, Mundis GM, Klineberg E et al (2016) Recovery following adult spinal deformity surgery: the effect of complications and reoperation in 149 patients with 2-year follow-up. Eur Spine J 25:2612–2621. https://doi.org/10.1007/s00586-015-3787-3
Passias PG, Soroceanu A, Yang S et al (2016) Predictors of revision surgical procedure excluding wound complications in adult spinal deformity and impact on patient-reported outcomes and satisfaction. J Bone Joint Surg 98:536–543. https://doi.org/10.2106/JBJS.14.01126
Yilgor C, Sogunmez N, Boissiere L et al (2017) Global alignment and proportion (GAP) score. J Bone Joint Surg 99:1661–1672. https://doi.org/10.2106/JBJS.16.01594
Qureshi R, Puvanesarajah V, Jain A et al (2017) Cost implications of primary versus revision surgery in adult spinal deformity. World Neurosurg 104:68–73. https://doi.org/10.1016/j.wneu.2017.05.002
Safaee MM, Dalle Ore CL, Zygourakis CC et al (2018) The unreimbursed costs of preventing revision surgery in adult spinal deformity: analysis of cost-effectiveness of proximal junctional failure prevention with ligament augmentation. Neurosurg Focus 44:E13. https://doi.org/10.3171/2018.1.FOCUS17806
Theologis AA, Miller L, Callahan M et al (2016) Economic impact of revision surgery for proximal junctional failure after adult spinal deformity surgery. Spine (Phila Pa 1976) 41:E964–E972. https://doi.org/10.1097/BRS.0000000000001523
le Huec JC, Charosky S, Barrey C et al (2011) Sagittal imbalance cascade for simple degenerative spine and consequences: algorithm of decision for appropriate treatment. Eur Spine J 20:699–703. https://doi.org/10.1007/s00586-011-1938-8
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30:346–353. https://doi.org/10.1097/01.brs.0000152379.54463.65
Schwab F, Ungar B, Blondel B et al (2012) Scoliosis research society—schwab adult spinal deformity classification. Spine (Phila Pa 1976) 37:1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2
Pekkanen L, Kautiainen H, Ylinen J et al (2011) Reliability and validity study of the finnish version 2.0 of the oswestry disability index. Spine (Phila Pa 1976) 36:332–338. https://doi.org/10.1097/BRS.0b013e3181cdd702
Bari TJ, Ohrt-Nissen S, Hansen LV et al (2019) Ability of the global alignment and proportion score to predict mechanical failure following adult spinal deformity surgery—validation in 149 patients with two-year follow-up. Spine Deform 7:331–337. https://doi.org/10.1016/j.jspd.2018.08.002
Baum GR, Ha AS, Cerpa M et al (2021) Does the global alignment and proportion score overestimate mechanical complications after adult spinal deformity correction? J Neurosurg Spine 34:96–102. https://doi.org/10.3171/2020.6.SPINE20538
Gupta MC, Yilgor C, Moon HJ et al (2021) Evaluation of global alignment and proportion score in an independent database. Spine J 21:1549–1558. https://doi.org/10.1016/j.spinee.2021.04.004
Ha AS, Hong DY, Coury JR et al (2021) Partial intraoperative global alignment and proportion scores do not reliably predict postoperative mechanical failure in adult spinal deformity surgery. Global Spine J 11:1046–1053. https://doi.org/10.1177/2192568220935438
Ham D-W, Kim H-J, Choi JH et al (2021) Validity of the global alignment proportion (GAP) score in predicting mechanical complications after adult spinal deformity surgery in elderly patients. Eur Spine J 30:1190–1198. https://doi.org/10.1007/s00586-021-06734-2
Jacobs E, van Royen BJ, van Kuijk SMJ et al (2019) Prediction of mechanical complications in adult spinal deformity surgery—the GAP score versus the Schwab classification. Spine J 19:781–788. https://doi.org/10.1016/j.spinee.2018.11.013
Ohba T, Ebata S, Oba H et al (2019) Predictors of poor global alignment and proportion score after surgery for adult spinal deformity. Spine (Phila Pa 1976) 44:E1136–E1143. https://doi.org/10.1097/BRS.0000000000003086
Wang M, Xu L, Chen X et al (2021) Optimal reconstruction of sagittal alignment according to global alignment and proportion score can reduce adjacent segment degeneration after lumbar fusion. Spine (Phila Pa 1976) 46:E257–E266. https://doi.org/10.1097/BRS.0000000000003761
Sun X, Sun W, Sun S et al (2021) Which sagittal evaluation system can effectively predict mechanical complications in the treatment of elderly patients with adult degenerative scoliosis? Roussouly classification or global alignment and proportion (GAP) score. J Orthop Surg Res 16:641. https://doi.org/10.1186/s13018-021-02786-8
Kwan KYH, Lenke LG, Shaffrey CI et al (2021) Are higher global alignment and proportion scores associated with increased risks of mechanical complications after adult spinal deformity surgery? An external validation. Clin Orthop Relat Res 479:312–320. https://doi.org/10.1097/CORR.0000000000001521
Kawabata A, Yoshii T, Sakai K et al (2020) Identification of predictive factors for mechanical complications after adult spinal deformity surgery. Spine (Phila Pa 1976) 45:1185–1192. https://doi.org/10.1097/BRS.0000000000003500
Funding
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital. The research has received funding from the Finnish Government Research Fund by the University of Eastern Finland. The funder had no role in the design of the study or collection, analysis, or interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
The corresponding main author was SH. She was a major contributor in writing the manuscript. She also participated in the data extraction. JPR was the supervisor and edited the manuscript. He also analyzed and interpreted the patient data. LP had a major role in the data extraction and analyzing. HK was responsible for statistical analyzes and wrote the statistical methods in a manuscript. The main supervisor was KK. She was a major contributor in editing the manuscript. She had the main responsibility in the data extraction and participated in statistical analyzes. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Consent for publication
Patient’s permission to participate and to publish the clinical study were acquired at admission to treatment to the institution and approved by the Chief Medical Physician. The consent we obtained from study participants was written.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the ethical committee of Central Finland Health Care District, 17U/2012. The consent we obtained from study participants was written.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hiltunen, S., Repo, J.P., Pekkanen, L. et al. Mechanical complications and reoperations after adult spinal deformity surgery: a clinical analysis with the GAP score. Eur Spine J 32, 1421–1428 (2023). https://doi.org/10.1007/s00586-023-07593-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07593-9