Abstract
Purpose
To investigate the association of age with delay in spine surgery and the effects on neurological outcome after traumatic spinal cord injury (SCI).
Methods
Ambispective cohort study (2011–2017) in n = 213 patients consecutively enrolled in a Level I trauma center with SCI care in a metropolitan region in Germany. Age-related differences in the injury to surgery interval and conditions associated with its delay (> 12 h after SCI) were explored using age categories or continuous variables and natural cubic splines. Effects of delayed surgery or age with outcome were analyzed using multiple logistic regression.
Results
The median age of the study population was 58.8 years (42.0–74.6 IQR). Older age (≥ 75y) was associated with a prolonged injury to surgery interval of 22.8 h (7.2–121.3) compared to 6.6 h (4.4–47.9) in younger patients (≤ 44y). Main reasons for delayed surgery in older individuals were secondary referrals and multimorbidity. Shorter time span to surgery (≤ 12 h) was associated with higher rates of ASIA impairment scale (AIS) conversion (OR 4.22, 95%CI 1.85–9.65), as mirrored by adjusted spline curves (< 20 h 20–25%, 20–60 h 10–20%, > 60 h < 10% probability of AIS conversion). In incomplete SCI, the probability of AIS conversion was lower in older patients [e.g., OR 0.09 (0.02–0.44) for’45-59y’ vs.’ ≤ 44y’], as confirmed by spline curves (< 40y 20–80%, ≥ 40y 5–20% probability).
Conclusion
Older patient age complexifies surgical SCI care and research. Tackling secondary referral to Level I trauma centers and delayed spine surgery imposes as tangible opportunity to improve the outcome of older SCI patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aging society in industrialized high-income countries is introducing profound changes in the epidemiology of central nervous system (CNS) injuries. In traumatic brain injury (TBI), the demographic change of the recent decades is characterized by shifting patterns of etiology and premorbidity [1, 2]. A similar global trend with increasing rates of elderly patients is observed in traumatic spinal cord injury (SCI) [3] and has implications for emergency medicine, acute surgical care, and translational research [4].
Spine surgery performed as early as possible after the injury is recognized as outcome relevant after SCI [5]. However, multimorbidity and other age-related conditions may restrict the feasibility to perform spine surgery early after the injury. On the other hand, a link between age and poor neurofunctional outcome after SCI has been described [6,7,8,9], albeit neuroanatomical correlates of an age-related decline in axonal regeneration, evident in experimental models [10], could not be revealed in human pilot data [11]. This implies the question to what extent age is independently associated with neurological recovery after SCI and if age-related restrictions in acute surgical management may additionally confound neurological outcome.
This study explores the association of age with the injury to surgery interval and the conditions associated with the violation of the study center’s guideline to start the first spine surgery within 12 h (≤ 12 h) after SCI. In addition, the study investigates effects of the injury to surgery interval and age on neurological outcome.
Methods
Study oversight
The study was conducted within the Comparative Outcome and Treatment Evaluation in Spinal Cord Injury (COaT-SCI) project, which consecutively enrolls SCI patients aged 14 years or older admitted to the BG Hospital Unfallkrankenhaus Berlin, a Level 1 trauma center with 24 h/7d spine surgery service and a specialized treatment center for SCI (60 beds) located in the metropolitan region of Berlin, Germany.
The ambispective study included acute traumatic SCI patients enrolled from 2011 to 2017. Data were collected prospectively from May 2015 to December 2017 using case report forms. Retrospective data for the period from January 2011 to April 2015 were collected by chart review and were stored in a versioned database. For explorative comparison of patient characteristics and outcomes between both enrollment periods, see Supplementary Table 1.
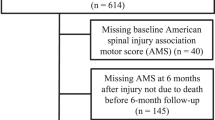
Patients who did not undergo spine surgery or whose initial surgery was performed at another center were excluded. Decisions to postpone surgery because of initially minor neurological deficits or spontaneous neurological improvement in association with spinal stenosis and/or central cord syndrome were additional exclusion criteria as they represented exemptions from the study center’s guideline to start the spine surgery ≤ 12 h after SCI. Patients who died during primary hospitalization were excluded only from the analysis of neurological outcome (Fig. 1).
Data analysis chart. Horizontal arrows indicate excluded patients. Cases without spine surgery or admitted after the first spine surgery were excluded. In addition, cases with minor neurological deficits or spontaneous neurological improvement in the context of spinal stenosis and/or central cord syndrome were excluded because they were exemptions to the study center’s internal guideline to start the surgery ≤ 12 h after SCI. The reasons for delayed spine surgery were recorded only if the ≤ 12 h timeframe was exceeded. Patients who died during primary hospitalization, or with missing neurological examination at discharge were excluded from the outcome analyses. Abbreviations: AIS = ASIA Impairment Scale, SCI = spinal cord injury
Variable definitions
For the explorative analysis of age effects, the International Spinal Cord Injury Core Data Set age categories for large sample sizes [12] were modified in a way that the younger age categories were combined to’ ≤ 44 years’ (≤ 44y) and compared to the’45–59 years’ (45-59y),’60–74 years’ (60–74y), and’ ≥ 75 years’ (≥ 75y) categories in order to achieve age groups of a similar size. Other demographic baseline characteristics included gender, body mass index (BMI), and the Charlson comorbidity index (CCI) based on pre-existing health conditions obtained from the medical records and by questioning the patients or their relatives. The CCI was calculated as described elsewhere [13]. TBI was graded according to the Glasgow Coma Scale as mild (I°), moderate (II°), or severe (III°). Other accompanying injuries include sternal-rib fractures, injury to the chest or abdominal cavities, fractures of the pelvis or the upper or lower extremities, or large vessel injuries. The etiology of SCI was categorized into falls, traffic accidents, and other types of injury comprising sports accidents, acts of violence, suicide attempts, and falling objects. The time of SCI was extracted from emergency medical records. Admission to the study center and the start of surgery (incision time) were documented in the electronic hospital information system. The exact time intervals from SCI to first spine surgery, from SCI to admission, and from admission to first spine surgery were calculated. The daytime of surgery was recorded and categorized into 7am–5 pm and 5 pm–7am. Spine surgery was categorized as delayed when the ≤ 12 h threshold representing the study center’s internal guideline for the start of the first spine surgery (cut time) was exceeded. As no common recommendations about the exact timing of early spine surgery are available [14] and the variability in clinical practice is huge [15], the trial center has determined the 12-h time window for spine surgery routines after acute traumatic SCI based on available literature and on feasibility considerations regarding transport routes and required diagnostics. In cases with the start of surgery > 12 h, the circumstances or health conditions contributing to the decision made by the team of emergency physicians, anesthesiologists, and spine surgeons to postpone the surgery were recorded.
For neurological classification at admission and discharge, the ASIA impairment scale (AIS) and the neurological level of injury (NLI) were assessed according to ISNCSCI [16] by physicians experienced in the treatment of SCI. For neurological outcome analysis, AIS changes over time were dichotomized into ‘non-conversion’ vs. ‘conversion’ and improvements in the NLI by at least two segments were considered as relevant. The follow-up ends at discharge from primary surgical or rehabilitation care. The median (IQR) time of follow-up in the study sample is 90 days (55–124).
Statistical analysis
For continuous variables, median and quartiles are reported as descriptive measures. Differences between groups were tested using the Kruskal–Wallis test followed by Dunn’s post-test for multiple comparison. Categorical variables were reported as absolute and relative frequencies and compared using the Chi-square test. To examine the association of age with primary or secondary referral, natural cubic splines were used in a sensitivity analysis. The neurological recovery was analyzed in the total sample and stratified for baseline AIS into complete SCI (AIS A) and incomplete SCI (AIS B–D) as the AIS represents a major prognostic factor [17] and in order to address interactions between age and AIS. The binary multiple regression models with AIS conversion as outcome variable included the independent variables: age group, gender, CCI, surgery ≤ 12 h after SCI, accompanying TBI, cervical NLI at admission, and, if applicable, AIS at admission. The enrollment period (retrospective vs. prospective) was also included to adjust for differences in data quality and possible variations of the ISNCSCI [18]. Considerations for model development were visualized by means of directed acyclic graphs (Supplementary Fig. 1) using the browser-based application DAGitty (version 3.0). Sensitivity analysis included binary multiple logistic regression models using continuous age and a logarithmic transformation of the time from injury to surgery instead of the respective categorized variables. Natural cubic splines were used for age and injury to surgery time where appropriate (decision based on AIC comparison between models). A two-sided significance level of α = 0.05 was used. If not otherwise stated, no adjustment for multiple testing was applied in this exploratory study. All p-values have to be interpreted cautiously. All analyses were performed in the COaT-SCI database version as of 03/18/2019 using the software SPSS (version 26.0) and R (packages ‘base,’ ‘splines,’ ‘ggeffects’ and ‘tidyverse’). The study was reported according to the STROBE statement [19] (Supplementary Table 2).
Results
Baseline characteristics
The median age of the study population (n = 213) was 58.8 years with an interquartile range (IQR) of 42.0–74.6 and a range of 14.1–90.7 years. When comparing the age groups, ‘60-74y’ and ‘ ≥ 75y’ included more female patients and had clearly higher BMI and CCI scores compared to ‘ ≤ 44y’ and ‘45-59y’ (Table 1). Falls were the prevailing etiology of SCI in the groups of older patients, whereas traffic accidents and other types of injury were much more frequent in the ‘45-59y’ and especially in the ‘ ≤ 44y’ group. A slight disparity in SCI severity across the age groups was attributable to a higher rate of 27.7% motor incomplete AIS C patients in the ‘ ≥ 75y’ group compared to the younger groups with rates between 6.3% and 9.3% (Table 1). The distribution of the NLI in the age groups shifted with older age toward much higher frequencies of cervical NLI and less frequent thoracic or lumbar NLI. Approximately one third of the ‘ ≤ 44y’ group had a cervical NLI (32.8%), whereas rates between 61.5% and 74.5% were observed in the older groups (Table 1).
The older patients suffered less frequently TBI or other accompanying injuries. The rate of severe TBI was 12.1% in the ‘ ≤ 44y’ and 8.9% in the ‘45-59y’ group, but 0.0% in the ‘60-74y’ and 2.0% in the ‘ ≥ 75y’ group. The rate of other concomitant injuries was also lower in older patients with 71.2% in the ‘ ≤ 44y’ compared to 38.8% in the ‘ ≥ 75y’ group (Table1).
Timing of surgical management
The injury to surgery time for decompression and/or stabilization [median (IQR), hours] was clearly shorter in the group ‘ ≤ 44y’ [6.6 (4.4–47.9)] compared to ‘60-74y’ [15.1 (6.0–63.8)] and particularly to ‘ ≥ 75y’ [22.8 (7.2–121.3)]. The ‘45-59y’ group had an injury to surgery time of [11.8 (6.3–58.8)] (Fig. 2a). Consequently, the study center’s internal guideline to start the first spine surgery ≤ 12 h after SCI could be met in more than half of the cases only in the ‘ ≤ 44y’ and ‘45-59y’ groups. Shorter injury to surgery time (≤ 12 h) in younger age groups was associated incomplete SCI AIS B-D (Fig. 2B). Frequency of surgeries within or outside regular working hours was similar between the age groups (Fig. 2C).
Timing of surgical management by age-subgroups. a Time from SCI to first spine surgery. The line indicates the 12 h threshold for the start of spine surgery (cut) based on the trial center’s internal guideline. b Frequency of spine surgery performed within the 12 h threshold stratified for the baseline AIS. Chi-square test comparing the onset of surgery categories (surgery ≤ 12 h vs. surgery > 12 h) between the age groups (AIS A p = 0.802; AIS B-D p = 0.003). c Frequency of spine surgery within or without regular working hours (7am–5 pm vs. 5 pm–7am) stratified for the baseline AIS. Chi-square test comparing the daytime of surgery categories between the age groups (AIS A p = 0.376; AIS B-D p = 0.096). d Time difference between SCI and admission to the trial center. e Time from trial center admission to first spine surgery. Bonferroni adjusted p-values of Dunn’s post-test after Kruskal–Wallis test are shown in the panels a, d, and e. Abbreviations: AIS = ASIA Impairment Scale, SCI = spinal cord injury
The time from SCI to study center admission [median (IQR), hours] differed considerably between the age groups ‘ ≤ 44y’ [1.5 (1.2–3.0)] or ‘45–60 years’ [1.6 (1.1–5.1)] compared to ‘60-74y’ [3.1 (1.5–22.7)] or ‘ ≥ 75y’ [4.1 (1.2–24.8)] (Fig. 2d). The time from admission to the first spine surgery was substantially longer only in the ‘ ≥ 75y’ [7.9 (4.3–48.0)] group compared with the ‘ ≤ 44y’ [3.8 (3.0–31.2)] group (Fig. 2e).
Reasons for delayed spine surgery
The main conditions associated with delayed spine surgery (> 12 h) after SCI were multiple trauma in the ‘ ≤ 44y’ and ‘45-59y’ groups and secondary referral from other hospitals as well as multimorbidity in the ‘60-74y’ and ‘ ≥ 75y' groups (Fig. 3a). Other conditions not observed in the ‘ ≤ 44y’ group, but relevant for postponed surgery in the ‘45-59y’ and the older groups, were intake of coagulation inhibitors (direct oral anticoagulants n = 4; coumarin derivates n = 4; antiplatelet drugs n = 1) or extended diagnostics in cases with underlying ankylosing spondylitis (Fig. 3a).
Reasons for delay in spine surgery and association of age with primary referral. a Reasons for surgery performed > 12 h after SCI. Sample size (reasons/patients): total n = 111/102, ‘ ≤ 44 y’ n = 24/23, ‘45–59 y’ n = 23/22, ‘60–74 y’ n = 31/29, ‘ ≥ 75y’ n = 33/28. b Estimated probability of primary referral as function in association to patient age based on binary logistic regression using natural cubic splines with 3 degrees of freedom (n = 213 patients). Abbreviations: SCI = spinal cord injury
In a subgroup analysis, the rate of secondary referrals was higher in the older age groups (Table 2). The median time from injury to admission was considerably longer in patients with secondary referral compared to those in the primary referral groups. Similarly, the injury to surgery time interval was prolonged in the secondary referral compared to the primary referral groups. However, the median time from trial center admission to surgery was not longer in each age group after secondary referral (Table 2).
Sensitivity analysis using natural cubic splines revealed that patients ≥ 60 years of age were less likely to have a primary referral (45–55% probability) compared with younger age groups (65–75% probability) (Fig. 3b).
Neurological outcome
Comparing the spine surgery categories (surgery ≤ 12 h, surgery > 12 h) in the total sample, AIS conversions were occurring more frequently, when the surgery began ≤ 12 h compared to > 12 h within all four age groups but without clear differences between the age groups (Fig. 4a). After stratification for the AIS at admission, a rather similar pattern of AIS conversions was observed in AIS A (Fig. 4b). In the AIS B–D stratum, a majority of patients with surgery ≤ 12 h after SCI experienced an AIS conversion across all age groups, but particularly the ‘ ≤ 44y’ group converted more frequently than the older groups (Fig. 4c).
Neurological recovery in the total sample and stratified for severity of SCI. a Pattern of AIS conversion in the total sample. Chi-square test comparing AIS conversion between spine surgery categories (surgery < = 12 h, surgery > 12 h) p < 0.001. Chi-square test comparing age groups p = 0.272. b AIS conversion in patients AIS A at baseline. Chi-square test comparing AIS conversion between spine surgery categories p = 0.021. Chi-square test comparing AIS conversion between age groups p = 0.358 c AIS changes in patients AIS B-D at baseline. Chi-square test comparing AIS conversion between spine surgery categories p < 0.001. Chi-square test comparing AIS conversion between age groups p = 0.004. d Pattern of NLI changes by more than two segments in the total sample. Chi-square test comparing NLI changes between spine surgery categories p = 0.011. Chi-square test comparing NLI changes between age groups p = 0.023. e NLI changes in patients AIS A at baseline. Chi-square test comparing NLI changes between spine surgery categories p = 0.143. Chi-square test comparing NLI changes between age groups p = 1. f Frequency of NLI changes for patients AIS B-D at baseline. Chi-square test comparing NLI changes between spine surgery categories p = 0.004. Chi-square test comparing NLI changes between age groups p = 0.002. Abbreviations: AIS = ASIA Impairment Scale, SCI = spinal cord injury
The analysis of NLI changes in the total sample revealed higher rates of improvement both when the surgery has started ≤ 12 h compared to > 12 h and in the younger compared to the older groups (Fig. 4d). This pattern of NLI changes did not apply to the AIS A stratum (Fig. 4e), but to AIS B–D revealing patterns of NLI improvement (Fig. 4f) very similar to AIS conversions (Fig. 4c).
The adjusted logistic regression model calculated in the total sample demonstrated a higher probability of AIS conversion when the surgery began ≤ 12 h after SCI [OR (95% CI) of 4.22 (1.85–9.65)]. In addition, the baseline AIS was associated with AIS conversion, but only a weak association of age with probability of AIS conversion was observed (Table 3). Sensitivity analysis using natural cubic splines of continuous age and injury to surgery time confirmed these results (Table 4). The adjusted spline curve for probability of AIS conversion declined from 45 to 15% in patients ≤ 40 years and it plateaued at a probability of 10% in patients > 40 years (Fig. 5a). Regarding the injury to surgery time, the adjusted curve indicated the highest probability for AIS conversion at > 20% when the surgery was performed < 20 h after SCI and the probability declined to below 10% when the surgery began > 60 h after SCI (Fig. 5b).
Estimated probability of AIS conversion using natural cubic splines. The probability of AIS conversion in association with patient age a the injury to surgery interval b in the total sample (n = 192) and with patient age in the AIS B-D stratum c (n = 110) was calculated based on multiple binary logistic regression using natural cubic splines with 2 degrees of freedom, adjusted for sex, CCI, AIS at admission, NLI at admission, TBI, time from SCI to surgery (log-transformed) and enrollment period
In the AIS A stratum, a clear effect of surgery ≤ 12 h, but not of age on AIS conversions was observed (Table 3). Here, cervical NLI indicated a higher probability for AIS conversion [OR (95% CI), 12.74 (2.12–76.72)]. Sensitivity analysis using age and the injury to surgery interval as continuous variables confirmed these effects (Table 4). In the AIS B–D stratum, the surgery ≤ 12 h status was also associated with a higher probability for AIS conversion [3.00 (1.02–8.88)] and older age indicated a lower prospect to improve [‘45-59y,’ 0.09 (0.02–0.44); ‘60-74y,’ 0.12 (0.02–0.67); and ‘ ≥ 75y,’ 0.10 (0.02–0.61)] compared to the ‘ ≤ 44y’ reference group. Significant additional effects in the AIS A–B stratum were also observed for the AIS at admission and the enrollment period (Table 3). Sensitivity analysis using natural cubic spline of age and the log-transformed injury to surgery interval as covariates confirmed the effect of age. The effect of the injury to surgery interval however was weaker when the continuous injury to surgery interval was used instead of the categorical variable (Table 4). The adjusted spline curve for probability of AIS conversion in association with age declined steeply from 80 to 20% in patients < 40 years and it plateaued at a probability between 5 and 20% in patients ≥ 40 years (Fig. 5c).
Discussion
The fact that half of the study population is at least 59 years old and experienced significant delay in spine surgery underlines the importance of rethinking SCI emergency care algorithms for elderly patients [4, 20]. The result that spine surgery ≤ 12 h after SCI is associated with better neurological outcome across all age groups adds confirmative evidence to previous studies on the timing of decompression and/or stabilization [5]. Older SCI patients suffer fewer multiple injuries, which are the main reason for postponed spine surgery in younger patients. However, missing the study center’s aim to start the surgery ≤ 12 h after SCI can be linked with secondary referral to the Level-1 trauma center particularly in elderly patients with incomplete SCI. This generates the hypothesis that the urgency of spine surgery in this group of patients could be underestimated in the pre-hospital setting. This assumption is supported by our observation that, in contrast to younger SCI patients, the majority of elderly patients has secondary referrals and that the delay in admission to the study center is constantly contributing to the prolonged injury to surgery intervals, whereas the delay after admission exposed a more random pattern attributable to pre-existing individual injury or health conditions including multiple pre-morbidities, oral anticoagulation, or ankylosing spondylitis, the latter of which bares diagnostic challenges in the imaging of occult fractures [21] and requires more complex surgical procedures [22].
In incomplete SCI (AIS B–D), the adjusted regression models reveal age effects additional to the effects of the injury to surgery interval. Thus, not only delayed spine surgery, but also biological effects of aging on neuronal plasticity and/or regeneration may contribute to a poorer neurological outcome [23]. That age effects are observed only after incomplete SCI is consistent with a multicenter study, which has demonstrated stronger age effects on functional recovery in AIS B or C rather than in AIS A cohorts [9] and can be explained by the higher potential for intrinsic recovery in incomplete SCI [17, 24] providing a greater margin for functional loss due to outcome modifying factors [25].
Limitations of the study are its monocenter design and that is not population based. In addition, the follow-up ended at discharge from primary SCI care at a median time of 90 days and thus is not standardized. However, the study was conducted in a Level I trauma center with a supra-regional catchment area and a large specialized SCI treatment center allowing for a disease specific assessment of acute healthcare data, which are not available in European multicenter datasets in this detail [26]. Notably, the distribution of neurological baseline and neurological recovery profiles (ISNCSCI) observed in this study is consistent with multicenter studies in Europe and North America [17]. In addition, the demographic structure of the sample regarding age and gender matches recent data from a nationwide German neurotrauma study [2]. Therefore, the sample seems to have sufficient external validity to allow for explorative studies reflecting urban settings in industrialized countries.
Secondary referral to the study center was one of the most frequent reasons for the delay of the first spine surgery in older patients with incomplete SCI in this study, and this delay was associated with worse neurological outcome. Although observational studies are limited in their ability to reveal causal relationships, the study results are relevant for future health services research on how a straight access of elderly SCI patients to a center with specialized 24 h/7d spine surgery service can be achieved and to evaluate effects of initial referral to specialized centers as a target to improve SCI care [27]. Furthermore, since both delayed spine surgery and age can be considered as independent confounders of neurological recovery, the study findings are relevant to the design of clinical trials [28] on neurorestorative therapies.
Availability of data and material
The dataset analyzed in the current study is not publicly available due to legal restrictions under the General Data Protection Regulation of the European Union and other applicable national or local privacy regulations but are available from the corresponding author on reasonable request.
Code availability
The syntax code used with the statistical software SPSS (version 26.0) and the R script can be provided by the corresponding author upon reasonable request. The code used with the DAGitty online application (version 3.0) is attached to the legend of Supplementary Fig. 1.
References
Roozenbeek B, Maas AI, Menon DK (2013) Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol 9:231–236. https://doi.org/10.1038/nrneurol.2013.22
Maegele M, Lefering R, Sakowitz O, Kopp MA, Schwab JM, Steudel W, Unterberg A, Hoffmann R, Uhl E, Marzi I (2019) The Incidence and Management of Moderate to Severe Head Injury. A retrospective analysis of data from the Trauma Register of the German Trauma Society. Dtsch Arztebl Int 116:167–173
WHO (2013) International Perspectives on Spinal Cord Injury
Badhiwala JH, Ahuja CS, Fehlings MG (2018) Time is spine: a review of translational advances in spinal cord injury. J Neurosurg Spine 30:1–18. https://doi.org/10.3171/2018.9.SPINE18682
Badhiwala JH, Wilson JR, Witiw CD, Harrop JS, Vaccaro AR, Aarabi B, Grossman RG, Geisler FH, Fehlings MG (2021) The influence of timing of surgical decompression for acute spinal cord injury: a pooled analysis of individual patient data. Lancet Neurol 20:117–126. https://doi.org/10.1016/S1474-4422(20)30406-3
Cifu DX, Huang ME, Kolakowsky-Hayner SA, Seel RT (1999) Age, outcome, and rehabilitation costs after paraplegia caused by traumatic injury of the thoracic spinal cord, conus medullaris, and cauda equina. J Neurotrauma 16:805–815. https://doi.org/10.1089/neu.1999.16.805
Cifu DX, Seel RT, Kreutzer JS, McKinley WO (1999) A multicenter investigation of age-related differences in lengths of stay, hospitalization charges, and outcomes for a matched tetraplegia sample. Arch Phys Med Rehabil 80:733–740
Furlan JC, Fehlings MG (2009) The impact of age on mortality, impairment, and disability among adults with acute traumatic spinal cord injury. J Neurotrauma 26:1707–1717. https://doi.org/10.1089/neu.2009-0888
Wilson JR, Davis AM, Kulkarni AV, Kiss A, Frankowski RF, Grossman RG, Fehlings MG (2014) Defining age-related differences in outcome after traumatic spinal cord injury: analysis of a combined, multicenter dataset. Spine J 14:1192–1198. https://doi.org/10.1016/j.spinee.2013.08.005
Geoffroy CG, Hilton BJ, Tetzlaff W, Zheng B (2016) Evidence for an Age-Dependent Decline in Axon Regeneration in the Adult Mammalian Central Nervous System. Cell Rep 15:238–246. https://doi.org/10.1016/j.celrep.2016.03.028
Furlan JC, Bracken MB, Fehlings MG (2010) Is age a key determinant of mortality and neurological outcome after acute traumatic spinal cord injury? Neurobiol Aging 31:434–446. https://doi.org/10.1016/j.neurobiolaging.2008.05.003
Biering-Sorensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, Post MWM, Vogel L (2017) International Spinal Cord Injury Core Data Set (version 2.0)-including standardization of reporting. Spinal Cord 55:759–764. https://doi.org/10.1038/sc.2017.59
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Wilson JR, Tetreault LA, Kwon BK, Arnold PM, Mroz TE, Shaffrey C, Harrop JS, Chapman JR, Casha S, Skelly AC, Holmer HK, Brodt ED, Fehlings MG (2017) Timing of Decompression in Patients With Acute Spinal Cord Injury: A Systematic Review. Global Spine J 7:95S-115S. https://doi.org/10.1177/2192568217701716
Fehlings MG, Rabin D, Sears W, Cadotte DW, Aarabi B (2010) Current practice in the timing of surgical intervention in spinal cord injury. Spine 35:S166-173. https://doi.org/10.1097/BRS.0b013e3181f386f6
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, Donovan W, Graves D, Jha A, Jones L, Mulcahey MJ, Krassioukov A (2011) Reference for the 2011 revision of the international standards for neurological classification of spinal cord injury. J Spinal Cord Med 34:547–554. https://doi.org/10.1179/107902611X13186000420242
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, Bartlett PF, Blight AR, Dietz V, Ditunno J, Dobkin BH, Havton LA, Ellaway PH, Fehlings MG, Privat A, Grossman R, Guest JD, Kleitman N, Nakamura M, Gaviria M, Short D (2007) Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 45:190–205. https://doi.org/10.1038/sj.sc.3102007
Solinsky R, Kirshblum SC (2018) Challenging questions regarding the international standards. J Spinal Cord Med 41:684–690. https://doi.org/10.1080/10790268.2017.1362929
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology 18:800–804. https://doi.org/10.1097/EDE.0b013e3181577654
Oner C, Rajasekaran S, Chapman JR, Fehlings MG, Vaccaro AR, Schroeder GD, Sadiqi S, Harrop J (2017) Spine Trauma-What Are the Current Controversies? J Orthop Trauma 31(Suppl 4):S1–S6. https://doi.org/10.1097/BOT.0000000000000950
Tavolaro C, Ghaffar S, Zhou H, Nguyen Q, Bellabarba C, Bransford R (2019) Is routine MRI of the spine necessary in trauma patients with ankylosing spinal disorders or is a CT scan sufficient? Spine J. https://doi.org/10.1016/j.spinee.2019.03.004
Reinhold M, Knop C, Kneitz C, Disch A (2018) Spine fractures in ankylosing diseases: recommendations of the spine section of the German society for orthopaedics and trauma (DGOU). Global Spine J 8:56S-68S. https://doi.org/10.1177/2192568217736268
Geoffroy CG, Meves JM, Zheng B (2017) The age factor in axonal repair after spinal cord injury: A focus on neuron-intrinsic mechanisms. Neurosci Lett 652:41–49. https://doi.org/10.1016/j.neulet.2016.11.003
Curt A, Van Hedel HJ, Klaus D, Dietz V (2008) Group E-SS recovery from a spinal cord injury: significance of compensation, neural plasticity, and repair. J Neurotrauma 25:677–685. https://doi.org/10.1089/neu.2007.0468
Kopp MA, Watzlawick R, Martus P, Failli V, Finkenstaedt FW, Chen Y, DeVivo MJ, Dirnagl U, Schwab JM (2017) Long-term functional outcome in patients with acquired infections after acute spinal cord injury. Neurology 88:892–900. https://doi.org/10.1212/WNL.0000000000003652
EMSCI European Multicenter Study about Spinal Cord Injury. http://emsci.org. Accessed 01–21–2021
Richard-Denis A, Ehrmann Feldman D, Thompson C, Bourassa-Moreau E, Mac-Thiong JM (2017) Costs and length of stay for the acute care of patients with motor-complete spinal cord injury following cervical trauma: the impact of early transfer to specialized acute SCI center. Am J Phys Med Rehabil 96:449–456. https://doi.org/10.1097/PHM.0000000000000659
Jackson JW (2016) Diagnostics for confounding of time-varying and other joint exposures. Epidemiology 27:859–869. https://doi.org/10.1097/EDE.0000000000000547
Acknowledgements
We would like to thank Julian Rind and Elias Baumgartner for their support in data acquisition. The BG Hospital Unfallkrankenhaus Berlin is member of the European Multicenter Trial about Spinal Cord Injury (EMSCI) and acknowledges the support of EMSCI in ISNCSCI training. The work of MAK receives funding support from the Wings for Life Spinal Cord Research Foundation (Grants WfL-DE-16/16 and WfL-DE-11/20). The work of JMS is supported by the National Institute of Disability, Independent Living and Rehabilitation Research (NIDILRR Grant 90SI5020), the National Institutes of Neurological Disorders-NIH (Grant R01 NS118200-01), the European Union (EU EraNet – Neuron Program, SILENCE Grant 01EW170A), the Craig H Neilsen Foundation (Grant 596764), the Wings for Life Spinal Cord Research Foundation and the William E. Hunt and Charlotte M. Curtis endowment. JMS is a Discovery Theme Initiative Scholar (Chronic Brain Injury) of the Ohio State University.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors have not received any specific funding for their work related to this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data were collected by MAK, TLü, AN, EP, JL, MK, and TLi. Source verification of key data was performed by MH. The statistical analysis was performed by TLü, MAK, and UG. The first draft of the manuscript was written by MAK and TLü. All authors contributed on the intellectual content of the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they have no conflicts of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional Ethics Committee of Charité—Universitätsmedizin Berlin (Approval Number EA2/015/15) and with the 1964 Helsinki Declaration and its later amendments and other applicable ethical standards.
Consent to participate
If applicable, informed consent for the study participation was obtained from the individual participants prior to the inclusion in the Comparative Outcome and Treatment Evaluation in Spinal Cord Injury (COaT-SCI) study. In case that it was not reasonable to obtain informed consent, only routinely collected clinical care data were used for non-commercial research in accordance with the regulations of the Berlin State Hospital Act in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kopp, M.A., Lübstorf, T., Blex, C. et al. Association of age with the timing of acute spine surgery–effects on neurological outcome after traumatic spinal cord injury. Eur Spine J 31, 56–69 (2022). https://doi.org/10.1007/s00586-021-06982-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06982-2