Abstract
Purpose
To determine whether abnormalities of the sagittal modifiers (SMs) of the Scoliosis Research Society (SRS)-Schwab classification truly reflect back pain (BP)-specific quality of life (QOL), it is necessary to examine their dose–response relationships and to determine clinically impactful thresholds for declines in BP-specific QOL. This study aimed to analyse the continuous dose–response relationship between each SM and BP-specific QOL.
Methods
This cross-sectional study, using data from a Japanese population-based cohort study, included 519 community-dwelling residents aged ≥ 50 years who participated in the annual health examination. The participants completed the Roland–Morris Disability Questionnaire (RDQ) on BP-specific QOL. Spino-pelvic alignment based on SMs was assessed by whole-spine X-ray examinations. We fitted general linear models with or without nonlinear terms to estimate the dose–response relationship between each SM and BP-specific QOL.
Results
Pelvic tilt, pelvic incidence minus lumbar lordosis (PI-LL), and sagittal vertical axis showed dose–response relationships with BP-specific QOL measured as the RDQ score. PI-LL was most likely to predict a minimally clinically important RDQ score when its value exceeded the 90th percentile. A nonlinear relationship between PI-LL and the BP-specific QOL score was found. RDQ increased when PI-LL exceeded 10°.
Conclusion
PI-LL might be the most sensitive of the three modifiers of the SRS-Schwab classification for determining BP-specific QOL. Moreover, BP-specific QOL worsens rapidly when the compensatory mechanism against malalignment exceeds a critical value. Therefore, we suggest that traditional classifications and surgical strategies should be re-examined regarding the dose-dependent abnormalities of the SMs to develop a more reliable classification strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
To evaluate the indications for the treatment of degenerative changes and post-traumatic deformities of the spine, an accurate radiographic assessment of the whole-spine is required. The importance of this assessment lies in the concept of ‘cone of economy’ that states that energy consumption is minimised when the centre of the gravity of the body is maintained in a cone centred on the trunk [1]. Spinal deformities due to degenerative changes and post-traumatic deformities increase the energy consumption required to maintain the centre of gravity within this cone [2]. However, once these deformities disrupt the compensatory mechanism for maintaining the centre of gravity, symptoms such as pain, disability, and psychological distress appear [3, 4].
The Scoliosis Research Society (SRS)-Schwab classification is one of the most widely used to classify adult spinal deformities [5]. This classification comprises four coronal curve types and three sagittal modifiers (SMs) (pelvic tilt [PT], pelvic incidence [PI] minus lumbar lordosis [LL] [PI-LL], and sagittal vertical axis [SVA] as global alignment [GA]); these SMs are widely used as treatment benchmarks [6], and they have been reported to be more correlated with back pain (BP)-specific quality of life (QOL) scores than coronal alignment [3, 4, 7]. However, previous studies which demonstrated this correlation could only show the degrees of linearity of the relationships between the SMs and BP-specific QOL. Therefore, quantifying the shapes and magnitudes of the continuous relationships between the SMs and BP-specific QOL is clinically important to determine impactful thresholds for declines in BP-specific QOL among community-dwelling individuals, including those with and without deformities.
This study aimed to analyse such relationships using a sub-cohort of the Locomotive Syndrome and Health Outcome in Aizu Cohort Study (LOHAS). We hypothesised that each SM would have a similar degree of dose–response relationship to BP-specific QOL.
Materials and methods
Study setting
This cross-sectional study was a secondary analysis of the LOHAS, involving residents from Tadami and Minami-aizu in Fukushima Prefecture, Japan, and was conducted according to the STROBE guidelines. Details regarding the setting and baseline characteristics of the study have been reported previously [8]. This study included residents aged ≥ 50 years who participated in the annual health examination conducted during 2010. We did not set any exclusion criteria. The Research Ethics Committee of our institute approved the study protocol (no. 673), and written informed consent was obtained from all participants.
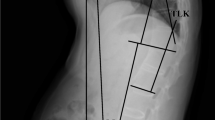
Definition of spino-pelvic alignment and radiographic evaluation
Spino-pelvic alignment (SPA) based on sagittal parameters was assessed by a whole-spine X-ray examination performed with participants in the standing position and their hands on the supraclavicular fosse [9]. We measured the following SPA characteristics using Surgimap Spine software (Nemaris Inc., USA): LL, PT, PI, PI-LL, and SVA. Each SPA characteristic was defined as follows [10]: LL, the angle between the L1 superior endplate and upper sacral plate; PT, the angle between the vertical reference line and the line connecting the midpoint of the sacral plate to the centre of the femoral heads; PI, the angle between the line perpendicular to the sacral plate and the line connecting the midpoint of the sacral plate to the centre of the femoral heads; PI-LL, PI minus LL; and SVA, the horizontal distance between the posterosuperior point of the S1 vertebral body and a vertical plumb line drawn from the centre of the C7 vertebral body. Measurements were performed by two independent examiners (R.T. and Y.K). Intra- and inter-rater measurement reliabilities were excellent (Supplementary file 1).
Outcome measurements: RDQ
The Roland–Morris Disability Questionnaire (RDQ) is a BP-specific QOL scale [11]. It is a self-administered questionnaire to measure disability caused by a low BP. It comprises 24 items; the total score is calculated based on the number of positive (yes) responses given. A high RDQ score indicates low QOL [12]. The RDQ is extremely useful in any situation when the expected level of dysfunction in participants is low; therefore, it may be more useful in primary care settings than the Oswestry disability index [13]. The questionnaire was completed by each patient at the time of their annual health examination.
Measurements of potential confounders
We selected potential confounders according to the epidemiological definition of variables determining both (1) the exposure (SMs) and (2) outcome (RDQ). After considering the clinical perspective and existing evidence [14], confounders of the association between SMs and RDQ included demographic characteristics such as age, sex, and underlying degenerative diseases (degenerative spondylolisthesis or isthmic spondylolisthesis), as well as surgical history. An experienced spine surgeon (K.O.) reviewed all radiographs and classified them according to these pathologies. We also obtained the spinal surgery history according to the whole-spine radiograph.
Calculations
Statistical analyses
Statistical analyses were conducted using Stata/SE software version 15 (Stata Corp., College Station, TX, USA). Participant characteristics were described using summary statistics. The distributions of PT, PI-LL, SVA as GA, and RDQ score are shown using histograms. To estimate the continuous dose–response relationships between the RDQ score and indices of SMs (PT, PI-LL, and SVA), linear regression models were fitted with robust standard errors. Age, sex, underlying spinal disease (none, degenerative spondylolisthesis, or isthmic spondylolisthesis), and surgical history (none, spinal fixation, or hip arthroplasty) were included as covariates in the models (Model 1). Additionally, according to the multivariable linear regression models, the mean RDQ scores predicted by the nonlinear or linear exposure variables were visually presented. We also examined the associations between the indices of SMs categorised by the SRS-Schwab classification and the RDQ score (Model 2). Details are presented in the Supplementary file 2. P < 0.05 was considered statistically significant.
Results
Descriptive statistics
Among 840 individuals who were included in the study, 615 (73.2%) participated in the RDQ survey. After excluding 96 participants with incomplete responses or missing confounding variables, 519 (61.8%) participants were included in the primary analysis (Fig. 1).
Table 1 summarises the characteristics of the study participants. Histograms of PT, PI-LL, and SVA are presented in Fig. 2. The median and interquartile range of the RDQ score were 0 and 0–3, respectively. The score of 305 (58.8%) patients was zero, and the maximum score was 22. The RDQ scores had a right-skewed distribution (Fig. 3).
Outcome data
The association between PT and the RDQ score is presented in Table 2. A nonlinear relationship was not supported (Model 1, P for nonlinearity = 0.076). A 1-standard deviation (SD) increase in PT was associated with a 0.45-point (95% confidence interval [CI], 0.04–0.86) higher RDQ score. The predicted RDQ score by PT value is shown in Fig. 4. In Model 2, PT > 30° was not associated with higher RDQ scores (mean difference, 1.28 points; 95% CI, − 0.17–2.74) compared with PT < 20°.
The Roland-Morris Disability Questionnaire (RDQ) score predicted using the continuous pelvic tilt (PT) value: Using the multivariable linear model including age, sex, underlying degenerative disease, and surgical history, the adjusted mean RDQ score for PT was predicted. The left vertical axis shows the adjusted RDQ score. The black solid line indicates point estimates of the RDQ score. The dotted lines indicate 95% confidence intervals. Grey bars indicate the frequency at which the PT values were observed. The right vertical axis shows the frequency of each grey bar. The red vertical lines indicate the boundary for the Scoliosis Research Society -Schwab classification
The association between PI-LL and the RDQ score is presented in Table 3. A nonlinear relationship was evident (Model 1, P for nonlinearity = 0.041). The predicted RDQ score by PI-LL value is shown in Fig. 5. When PI-LL exceeded 10°, the RDQ score sharply elevated. For example, at a PI-LL of 40°, the RDQ score was 4.6 points (95% CI, 2.8–6.4). In Model 2, PI-LL > 20° was associated with 1.38-point higher RDQ scores (95% CI, 0.05–2.72) compared with PI-LL ≤ 10°.
The Roland-Morris Disability Questionnaire (RDQ) score predicted using the continuous pelvic incidence minus lumbar lordosis (PI-LL) value: Using the multivariable linear model with restricted cubic spline including age, sex, underlying degenerative disease, and surgical history, the adjusted mean RDQ score for PI-LL was predicted. The left vertical axis shows the adjusted RDQ score. The black solid line indicates point estimates of the RDQ score. The dotted lines indicate 95% confidence intervals. Grey bars indicate the frequency at which the PI-LL values were observed. The right vertical axis shows the frequency of each grey bar. The red vertical lines indicate the boundary for the Scoliosis Research Society-Schwab classification
The association between SVA as GA and the RDQ score is presented in Table 4. A nonlinear relationship was not supported (Model 1, P for nonlinearity = 0.340). A 1-SD increase in SVA was associated with 0.61-point (95% CI, 0.18–1.05) higher RDQ scores. The predicted RDQ score by SVA value is shown in Fig. 6. In Model 2, SVA > 95 mm was not associated with higher RDQ scores (mean difference, 2.20 points; 95% CI, − 0.28–4.68) compared with SVA < 40 mm.
The Roland-Morris Disability Questionnaire (RDQ) score predicted using the continuous sagittal vertical axis (SVA) value: Using the multivariable linear model including age, sex, underlying degenerative disease, and surgical history, the adjusted mean RDQ score for SVA as global alignment (GA) was predicted. The left vertical axis shows the adjusted RDQ score. The black solid line indicates point estimates of the RDQ score. The dotted lines indicate 95% confidence intervals. Grey bars indicate the frequency at which the GA values were observed. The right vertical axis shows the frequency of each grey bar. The red vertical lines indicate the boundary for the Scoliosis Research Society -Schwab classification
The RDQ scores predicted by the percentiles of three modifiers are presented in Table 5. Among the scores predicted by the 90th percentiles of the three modifiers, only those predicted by PI-LL exceeded 3 points (3.06 points; 95% CI, 2.25–3.87). Additionally, the point estimate of the RDQ score predicted by the 95th percentile of PI-LL demonstrated the highest score among those predicted by the 95th percentiles of the three modifiers (3.78 points; 95% CI, 2.51–5.06).
Discussion
Among the dose–response relationships of the three SMs (PT, PI-LL, and SVA) with BP-specific QOL, PI-LL showed a distinctive nonlinear relationship. Additionally, only PI-LL-based SRS-Schwab classification category was associated with a worse BP-specific QOL. These findings suggest that PI-LL might be the most sensitive modifier determining BP-specific QOL among the three SMs.
Our findings partially agree with those of previous studies showing the correlations between the SMs of the SRS-Schwab classification with both BP-specific and general health-related QOL measurements [3, 4, 7]. However, although the relationships between the SMs and BP-specific QOL are not new concepts, we believe that our findings fill a gap in the literature. First, we were able to validate independent associations between the three SMs as continuous predictors and BP-specific QOL after adjustments for likely confounders. Second, this study revealed the clinical impact of the high values of three SMs on RDQ scores: participants with more than 95th percentile values of PT, PI-LL, or SVA have RDQ scores of ≥ 3 points on average, which corresponds to the minimally clinically important difference in the RDQ score [15]. In other words, the three SMs can be used to screen 5% of community-dwelling elderly individuals to identify people with disabilities affected by BP. Third, potential superiority of the PI-LL for evaluating BP-specific QOL impairment reinforces the recent evidence that PI is the only constant parameter providing key information about adult spino-pelvic degeneration [6, 16]. For example, the global alignment and proportion score based on PI is a tool for predicting the likelihood of mechanical complications after corrective surgery for patients with spinal deformity [6].
Interestingly, the finding that RDQ scores increased when PI-LL exceeded 10° may suggest that BP-specific QOL worsens rapidly when the compensatory mechanism against malalignment exceeds a critical value. This finding is the first empiric demonstration of the concept of the ‘cone of economy’ [1]: it is maintained within a particular range in sagittal alignment (e.g. within 10° in PI-LL); however, when it fails (e.g. > 10° in PI-LL), patient symptoms and health-related outcomes worsen rapidly. Collectively, our findings may suggest the need to revisit the traditional classifications and strategies for spinal surgeries such as instrumented fusion surgery based on a more reliable classification.
This study has several strengths. First, this is the first survey to focus on the shapes of the continuous dose–response relationships (i.e. not only correlation) between the three SMs and BP-specific QOL independent of the important confounders. Second, our data were thoroughly retrieved from a large population in the community. Recent studies have shown that sagittal alignment is widely involved not only in spinal deformity but also in many spinal disorders such as degenerative disc disease, osteoporosis, and facet joint arthritis [17,18,19]. An evaluation of sagittal alignment is not limited to corrective surgery for patients with spinal deformity; it should also be considered when treating localised spinal disorders [20]. During our study, alignment and QOL data were evaluated at the individual level via whole-spine radiographs and a questionnaire. Therefore, our findings reflect the actual general community setting and are applicable to other populations with any type of lumbar disease.
Despite these strengths, our study has some limitations. First, unmeasured factors leading to sagittal malalignment might have affected the results. Inter-vertebral disc degeneration, osteoporotic vertebral fractures, and trunk muscle mass are clinically important and might affect the relationship between sagittal alignment and BP-specific QOL [21]. Second, causality could not be assessed because of the cross-sectional nature of our study. However, the impact of altered SPA on BP-specific QOL is biologically plausible, and we believe that reverse causation is unlikely to occur given the traditional mechanisms of health-related QOL, in which biological changes in alignment and symptoms such as BP lead to a decline in function and perceived well-being [22]. Decreased LL triggers spinal deformity and causes sagittal imbalance, as reflected by an increased PI-LL value and SVA. Sagittal plane imbalance shifts the body towards the periphery of the ‘cone of economy’. Consequently, several compensatory mechanisms are deployed to help re-centre the body over the pelvis and to maintain an upright posture. When these compensatory mechanisms fail, efficiency performing daily living activities and QOL decline, and disruption of sagittal alignment leads to further decrease in QOL. Third, because the setting of this study was rural, the results may not be applicable to people living in urban areas. However, sagittal alignment parameters in this study were comparable to those of other Japanese cohort studies (Supplementary file 3) [23,24,25]. Therefore, our participants may represent the general Japanese population, and the findings may be reasonably applicable to all. Fourth, cervical spine alignment and lower limb joint alignment were not evaluated. Patients with deformity experienced changes in their alignment from the cervical spine to the ankle and used compensatory mechanisms to correct the imbalance.
Conclusion
PT, PI-LL, and SVA showed dose–response relationships with BP-specific QOL measured as the RDQ score among community-dwelling adults. Among the three modifiers of the SRS-Schwab classification, PI-LL might be the most sensitive for determining BP-specific QOL. Moreover, the new finding of a nonlinear relationship between PI-LL and the RDQ score found during our survey might potentially bring new insight to the classification and corrective surgery strategies for spinal disorders.
References
Dubousset J (1994) Three-dimensional analysis of the scoliotic deformity. The pediatric spine: principles and practice, Raven Press Ltd, New York
Klineberg E, Schwab F, Smith JS, Gupta MC, Lafage V, Bess S (2013) Sagittal spinal pelvic alignment. Neurosurg Clin North Am 24:157–162. https://doi.org/10.1016/j.nec.2012.12.003
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30:682–688 https://doi.org/10.1097/01.brs.0000155425.04536.f7
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30:2024–2029 https://doi.org/10.1097/01.brs.0000179086.30449.96
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis research society-schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37:1077–1082 https://doi.org/10.1097/BRS.0b013e31823e15e2
Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstück F, Pérez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A; European Spine Study Group (ESSG) (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99: 1661–1672 https://doi.org/10.2106/JBJS.16.01594
Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP (2009) Pelvic tilt and truncal inclination: Two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 34:E599–606 https://doi.org/10.1097/BRS.0b013e3181aad219
Otani K, Takegami M, Fukumori N, Sekiguchi M, Onishi Y, Yamazaki S, Ono R, Otoshi K, Hayashino Y, Fukuhara S, Kikuchi S, Konno S, LOHAS Research Group (2012) Locomotor dysfunction and risk of cardiovascular disease, quality of life, and medical costs: Design of the Locomotive Syndrome and Health Outcome in Aizu Cohort Study (LOHAS) and baseline characteristics of the study population. J Orthop Sci 17: 261–271 https://doi.org/10.1007/s00776-012-0200-5
Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW (2005) Is there an optimal patient stance for obtaining a lateral 36" radiograph? A critical comparison of three techniques. Spine (Phila Pa 1976) 30:427–433 https://doi.org/10.1097/01.brs.0000153698.94091.f8
Iyer S, Sheha E, Fu MC, Varghese J, Cunningham ME, Albert TJ, Schwab FJ, Lafage VC, Kim HJ (2018) Sagittal spinal alignment in adult spinal deformity: an overview of current concepts and a critical analysis review. JBJS Rev 6:e2. https://doi.org/10.2106/JBJS.RVW.17.00117
Roland M, Morris R (1983) A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 8:141–144 https://doi.org/10.1097/00007632-198303000-00004
Suzukamo Y, Fukuhara S, Kikuchi S, Konno S, Roland M, Iwamoto Y, Nakamura T, Committee on Science Project, Japanese Orthopaedic Association (2003) Validation of the Japanese version of the Roland-Morris disability questionnaire. J Orthop Sci 8: 543–548 https://doi.org/10.1007/s00776-003-0679-x
Deyo RA, Battie M, Beurskens AJ, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G (1998) Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976) 23:2003–2013 https://doi.org/10.1097/00007632-199809150-00018
Hallager DW, Hansen LV, Dragsted CR, Peytz N, Gehrchen M, Dahl B (2016) A comprehensive analysis of the SRS-Schwab adult spinal deformity classification and confounding variables: A prospective, con-US Cross-sectional study in 292 patients. Spine (Phila Pa 1976) 41:E589–597 https://doi.org/10.1097/BRS.0000000000001355
Bombardier C, Hayden J, Beaton DE (2001) Minimal clinically important difference. Low back pain: outcome measures. J Rheumatol 28:431–438
Zhou S, Xu F, Wang W, Zou D, Sun Z, Li W (2020) Age-based normal sagittal alignment in Chinese asymptomatic adults: establishment of the relationships between pelvic incidence and other parameters. Eur Spine J 29:396–404. https://doi.org/10.1007/s00586-019-06178-9
Kumar MN, Baklanov A, Chopin D (2001) Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 10:314–319. https://doi.org/10.1007/s005860000239
Miyakoshi N, Hongo M, Kobayashi T, Abe T, Abe E, Shimada Y (2015) Improvement of spinal alignment and quality of life after corrective surgery for spinal kyphosis in patients with osteoporosis: a comparative study with non-operated patients. Osteoporos Int 26:2657–2664. https://doi.org/10.1007/s00198-015-3163-5
Jentzsch T, Geiger J, Konig MA, Werner CM (2017) Hyperlordosis is associated with facet joint pathology at the lower lumbar spine. Clin Spine Surg 30:129–135. https://doi.org/10.1097/BSD.0b013e3182aab266
Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V (2015) Sagittal alignment of the spine: what do you need to know? Clin Neurol Neurosurg 139:295–301. https://doi.org/10.1016/j.clineuro.2015.10.024
Diebo BG, Shah NV, Boachie-Adjei O, Zhu F, Rothenfluh DA, Paulino CB, Schwab FJ, Lafage V (2019) Adult spinal deformity. Lancet 394:160–172. https://doi.org/10.1016/S0140-6736(19)31125-0
Wilson IB, Cleary PD (1995) Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 273:59–65. https://doi.org/10.1001/jama.1995.03520250075037
Banno T, Togawa D, Arima H, Hasegawa T, Yamato Y, Kobayashi S, Yasuda T, Oe S, Hoshino H, Matsuyama Y (2016) The cohort study for the determination of reference values for spinopelvic parameters (T1 pelvic angle and global tilt) in elderly volunteers. Eur Spine J 25:3687–3693. https://doi.org/10.1007/s00586-016-4411-x
Asai Y, Tsutsui S, Oka H, Yoshimura N, Hashizume H, Yamada H, Akune T, Muraki S, Matsudaira K, Kawaguchi H, Nakamura K, Tanaka S, Yoshida M (2017) Sagittal spino-pelvic alignment in adults: the Wakayama spine study. PLoS ONE 12:e0178697. https://doi.org/10.1371/journal.pone.0178697
Uehara M, Takahashi J, Ikegami S, Tokida R, Nishimura H, Sakai N, Kato H (2019) Sagittal spinal alignment deviation in the general elderly population: a Japanese cohort survey randomly sampled from a basic resident registry. Spine J 19:349–356. https://doi.org/10.1016/j.spinee.2018.06.346
Acknowledgements
The authors appreciate the LOHAS participants, staff of the public offices in Tadami and Minami-Aizu, and LOHAS research members for supporting this study. This work was also supported by JSPS KAKENHI Grant Number 19K18504.
Funding
The authors did not receive support from any organisation for the submitted work.
Author information
Authors and Affiliations
Contributions
RT, NK, MS, KO took part in conceptualisation. RT and NK involved in methodology. RT, NK, YK took part in formal analysis and investigation. RT and NK involved in writing—original draft preparation. YK, TN, MS, KO, MI, OS, SF, SK participated in writing—review and editing. MS, KO, SF, SK participated in funding acquisition. MS, KO, SF, SK took part in resources. MI, OS, SF, SK involved in supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Availability of data and material
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tominaga, R., Kurita, N., Kokubun, Y. et al. Dose-response relationship between spino-pelvic alignment determined by sagittal modifiers and back pain-specific quality of life. Eur Spine J 30, 3019–3027 (2021). https://doi.org/10.1007/s00586-021-06965-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06965-3