Abstract
Purpose
Spinal sagittal balance is associated with back pain and quality of life. Enhancing understanding of the clinical factors associated with sagittal balance is essential for guiding the development of effective non-operative treatment. We aimed to evaluate the associations between spinal sagittal balance and potentially modifiable clinical factors and interactions between current back pain and the evaluated clinical factors.
Methods
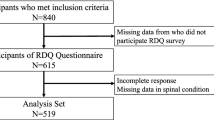
We conducted a cross-sectional study where sagittal alignment, measured radiographically by EOS, was defined by sagittal vertical axis (SVA). The clinical factors included non-radiographic (NR) lumbar lordosis angle, balance (Berg balance scale), hip and back extension range of motion (ROM) and extensor strength, and back pain. Pearson’s correlation coefficients and multivariable regression analyses were conducted in 63 adult participants (70% female, mean age 73 (SD 8.6) years) from the general population.
Results
We identified correlations between SVA and age (r = 0.4, p < 0.001), body mass index (BMI) (r = 0.3, p = 0.008), balance (r = − 0.5, p < 0.001) and NR lumbar lordosis angle (r = − 0.5, p < 0.001). The final model (R2 = 58%) identified that, after controlling for age and BMI, larger SVA was associated with lower NR lumbar lordosis (R2 = 15%, p < 0.001), poorer balance (R2 = 7%, p = 0.02), greater hip extensor strength (R2 = 4%, p = 0.053), and among people with back pain, NR lumbar extension ROM (R2 = 3%, p = 0.034). Hip ROM and lumbar strength were not significant.
Conclusion
Reduced NR lumbar lordosis magnitude and ROM, balance and hip strength are associated with SVA; however, it is unclear if these factors are compensatory, contributing, or modifiable. Hence, future longitudinal studies are needed.



Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Glassman SD, Bridwell K, Dimar JR et al (2005) The impact of positive sagittal balance in adult spinal deformity. Spine 30(18):2024–2029
Yamada T, Yamato Y, Hasegawa T et al (2020) Influence of the sagittal vertical axis on the risk of falls in community-dwelling elderly people: a retrospective longitudinal study. Spine Surg Relat Res 4(3):237–241. https://doi.org/10.22603/ssrr.2019-0082
Cheung JPY (2020) The importance of sagittal balance in adult scoliosis surgery. Ann Transl Med 8(2):35–35. https://doi.org/10.21037/atm.2019.10.19
James SL, Lucchesi LR, Bisignano C et al (2020) The global burden of falls: global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev 26(Supp 1):i3–i11. https://doi.org/10.1136/injuryprev-2019-043286
Acaroglu E, Yavuz AC, Guler UO et al (2016) A decision analysis to identify the ideal treatment for adult spinal deformity: is surgery better than non-surgical treatment in improving health-related quality of life and decreasing the disease burden? Eur Spine J 25(8):2390–2400. https://doi.org/10.1007/s00586-016-4413-8
Glassman SD, Carreon LY, Shaffrey CI et al (2020) Cost-effectiveness of adult lumbar scoliosis surgery: an as-treated analysis from the adult symptomatic scoliosis surgery trial with 5-year follow-up. Spine Deform. https://doi.org/10.1007/s43390-020-00154-w
Jacobs E, van Royen BJ, van Kuijk SMJ et al (2019) Prediction of mechanical complications in adult spinal deformity surgery-the GAP score versus the Schwab classification. The spine journal 19(5):781–788. https://doi.org/10.1016/j.spinee.2018.11.013
Kelly MP, Lurie JD, Yanik EL et al (2019) Operative versus nonoperative treatment for adult symptomatic lumbar scoliosis. J Bone Joint Surg Am 101(4):338–352. https://doi.org/10.2106/JBJS.18.00483
Le Huec JC, Thompson W, Mohsinaly Y et al (2019) Sagittal balance of the spine. Eur Spine J 28(9):1889–1905. https://doi.org/10.1007/s00586-019-06083-1
Saha D, Gard S, Fatone S et al (2007) The effect of trunk-flexed postures on balance and metabolic energy expenditure during standing. Spine 32(15):1605–1611. https://doi.org/10.1097/BRS.0b013e318074d515
Haddas R, Lieberman IH (2018) A method to quantify the “cone of economy.” Eur Spine J 27(5):1178–1187. https://doi.org/10.1007/s00586-017-5321-2
Hori Y, Hoshino M, Inage K et al (2019) ISSLS PRIZE IN CLINICAL SCIENCE 2019: clinical importance of trunk muscle mass for low back pain, spinal balance, and quality of life—a multicenter cross-sectional study. Eur Spine J 28(5):914–921. https://doi.org/10.1007/s00586-019-05904-7
Menezes-Reis R, Bonugli GP, Salmon CEG et al (2018) Relationship of spinal alignment with muscular volume and fat infiltration of lumbar trunk muscles. PLoS ONE 13(7):e0200198. https://doi.org/10.1371/journal.pone.0200198
Berry DB, Shahidi B, Rodríguez-Soto AE et al (2018) Lumbar muscle structure predicts operational postures in active-duty marines. J Orthop Sports Phys Ther 48(8):613–621. https://doi.org/10.2519/jospt.2018.7865
Akbar M, Terran J, Ames CP et al (2013) Use of Surgimap Spine in sagittal plane analysis, osteotomy planning, and correction calculation. Neurosurg Clin N Am 24(2):163–172. https://doi.org/10.1016/j.nec.2012.12.007
Hayden AM, Hayes AM, Brechbuhler JL et al (2018) The effect of pelvic motion on spinopelvic parameters. The spine journal 18(1):173–178. https://doi.org/10.1016/j.spinee.2017.08.234
Le Huec JC, Charosky S, Barrey C et al (2011) Sagittal imbalance cascade for simple degenerative spine and consequences: algorithm of decision for appropriate treatment. Eur Spine J 20(Suppl 5):699–703. https://doi.org/10.1007/s00586-011-1938-8
Morvan G, Mathieu P, Vuillemin V et al (2011) Standardized way for imaging of the sagittal spinal balance. Eur Spine J 20 Suppl 5 (Suppl 5):602–608. doi:https://doi.org/10.1007/s00586-011-1927-y
Krott NL, Wild M, Betsch M (2020) Meta-analysis of the validity and reliability of rasterstereographic measurements of spinal posture. Eur Spine J 29(9):2392–2401. https://doi.org/10.1007/s00586-020-06402-x
Schroeder J, Reer R, Braumann KM (2015) Video raster stereography back shape reconstruction: a reliability study for sagittal, frontal, and transversal plane parameters. Eur Spine J 24(2):262–269. https://doi.org/10.1007/s00586-014-3664-5
Pua YH, Wrigley TV, Cowan SM et al (2008) Intrarater test-retest reliability of hip range of motion and hip muscle strength measurements in persons with hip osteoarthritis. Arch Phys Med Rehabil 89(6):1146–1154. https://doi.org/10.1016/j.apmr.2007.10.028
Viveiro LAP, Gomes GCV, Bacha JMR, et al. (2019) Validity, and Ability to Identity Fall Status of the Berg Balance Scale, Balance Evaluation Systems Test (BESTest), Mini-BESTest, and Brief-BESTest in Older Adults Who Live in Nursing Homes. J Geriatr Phys Ther. 2019 Oct/Dec;42(4):E45-E54. doi: https://doi.org/10.1519/JPT.0000000000000215.
Berg K, Wood-Dauphine S, Williams JI et al (1989) Measuring balance in the elderly: preliminary development of an instrument. Physiother Can 41(6):304–311. https://doi.org/10.3138/ptc.41.6.304
Austin PC, Steyerberg EW (2015) The number of subjects per variable required in linear regression analyses. J Clin Epidemiol 68(6):627–636. https://doi.org/10.1016/j.jclinepi.2014.12.014
Portney L, Watkins M (2009) Foundations of clinical research. Pearson Education Inc., New Jersey
Wasserstein RL, Lazar NA (2016) The ASA statement on p-values: context, process, and purpose. Am Stat 70(2):129–133. https://doi.org/10.1080/00031305.2016.1154108
González-Gálvez N, Gea-García GM, Marcos-Pardo PJ (2019) Effects of exercise programs on kyphosis and lordosis angle: a systematic review and meta-analysis. PLoS ONE 14(4):e0216180. https://doi.org/10.1371/journal.pone.0216180
Bayattork M, Sköld MB, Sundstrup E et al (2020) Exercise interventions to improve postural malalignments in head, neck, and trunk among adolescents, adults, and older people: systematic review of randomized controlled trials. J Exerc Rehabil 16(1):36–48. https://doi.org/10.12965/jer.2040034.017
Gottipati P, Stine R, Ganju A et al (2018) The effect of positive sagittal spine balance and reconstruction surgery on standing balance. Gait Posture 62:227–234. https://doi.org/10.1016/j.gaitpost.2018.03.024
Diebo BG, Ferrero E, Lafage R et al (2015) Recruitment of compensatory mechanisms in sagittal spinal malalignment is age and regional deformity dependent: a full-standing axis analysis of key radiographical parameters. Spine 40(9):642–649. https://doi.org/10.1097/brs.0000000000000844
Pourtaheri S, Sharma A, Savage J et al (2017) Pelvic retroversion: a compensatory mechanism for lumbar stenosis. J Neurosurg Spine 27(2):137–144. https://doi.org/10.3171/2017.2.Spine16963
Barrey C, Roussouly P, Perrin G et al (2011) Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J 20 (5):626. doi:https://doi.org/10.1007/s00586-011-1930-3
Saimon Y, Goh AC, Momose K et al (2020) Correlation between radiographic sagittal alignment, range of motion, muscle strength, and quality of life in adults with spinal deformities. J Phys Ther Sci 32(2):140–147. https://doi.org/10.1589/jpts.32.140
Iyer S, Lenke LG, Nemani VM et al (2016) Variations in sagittal alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine 41(23):1826–1836. https://doi.org/10.1097/brs.0000000000001642
Shimizu M, Kobayashi T, Chiba H et al (2019) Adult spinal deformity and its relationship with hip range of motion: a cohort study of community-dwelling females. The Spine Journal 19(7):1202–1209. https://doi.org/10.1016/j.spinee.2019.02.006
Roussouly P, Pinheiro-Franco LH et al (2019) Sagittal balance of the spine: from normal to pathology: a key for treatment strategy. Thieme, New York
Ogon I, Takebayashi T, Takashima H et al (2017) Magnetic resonance spectroscopic analysis of multifidus muscles lipid content and association with spinopelvic malalignment in chronic low back pain. Br J Radiol 90(1073):20160753. https://doi.org/10.1259/bjr.20160753
Machino M, Ando K, Kobayashi K et al (2020) Influence of global spine sagittal balance and spinal degenerative changes on locomotive syndrome risk in a middle-age and elderly community-living population. BioMed Res Int 2020:3274864. https://doi.org/10.1155/2020/3274864
Makhni MC, Shillingford JN, Laratta JL et al (2018) Restoration of sagittal balance in spinal deformity surgery. J Korean Neurosurg Soc 61(2):167–179. https://doi.org/10.3340/jkns.2017.0404.013
Acknowledgements
Prof Armando Teixeira-Pinto (Biostatistician) for assistance with statistics.
Funding
Apart from author MS, no authors received support from any organization for the submitted work. MS received support from the University of Sydney SOAR fellowship.
Author information
Authors and Affiliations
Contributions
Author LC was involved with the conception, data collection, data analysis and write up of the manuscript. Author SD was involved with the conception, data collection, data analysis and write up of the manuscript. Author MS was involved with the conception, data collection, data analysis and write up of the manuscript. Author EP was involved with the conception, data collection, data analysis and write up of the manuscript. Author KR was involved with the data collection, data analysis and write up of the manuscript. LC, EP, SD, MS: Substantial contributions to the conception or design of the work (or), LC, EP, KR, SD, MS: acquisition, analysis, or interpretation of data for the work (and), LC, EP, KR, SD, MS: Drafting the work or revising it critically for important intellectual content (and), LC, EP, KR, SD, MS: Final approval of the version to be published
Corresponding author
Ethics declarations
Conflicts of interest
Author LC is a physiotherapist and has a financial interest at UprightCare clinic in Sydney Australia.
Ethics approval (include appropriate approvals or waivers)
Ethics approval was granted by Sydney University ethics committee. Ref 2016/1031.
Consent to participate (include appropriate statements)
All participants consented in writing to participate in study.
Consent for publication (include appropriate statements)
All authors consent to the publication of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cohen, L., Pappas, E., Refshauge, K. et al. Associations between potentially modifiable clinical factors and sagittal balance of the spine in older adults from the general population. Spine Deform 10, 433–441 (2022). https://doi.org/10.1007/s43390-021-00435-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00435-y