Abstract
Purpose
There are distinct differences in strategy amongst experienced surgeons from different ‘scoliosis schools’ around the world. This study aims to test the hypothesis that, due to the 3-D nature of AIS, different strategies can lead to different coronal, axial and sagittal curve correction.
Methods
Consecutive patients who underwent posterior scoliosis surgery for primary thoracic AIS were compared between three major scoliosis centres (n = 193). Patients were treated according to the local surgical expertise: Two centres perform primarily an axial apical derotation manoeuvre (centre 1: high implant density, convex rod first, centre 2: low implant density, concave rod first), whereas centre 3 performs posteromedial apical translation without active derotation. Pre- and postoperative shape of the main thoracic curve was analyzed using coronal curve angle, apical rotation and sagittal alignment parameters (pelvic incidence and tilt, T1–T12, T4-T12 and T10-L2 regional kyphosis angles, C7 slope and the level of the inflection point). In addition, the proximal junctional angle at follow-up was compared.
Results
Pre-operative coronal curve magnitudes were similar between the 3 cohorts and improved 75%, 70% and 59%, from pre- to postoperative, respectively (P < 0.001). The strategy of centres 1 and 2 leads to significantly more apical derotation. Despite similar postoperative T4-T12 kyphosis, the strategy in centre 1 led to more thoracolumbar lordosis and in centre 2 to a higher inflection point as compared to centre 3. Proximal junctional angle was higher in centres 1 and 2 (P < 0.001) at final follow-up.
Conclusion
Curve correction by derotation may lead to thoracolumbar lordosis and therefore higher risk for proximal junctional kyphosis. Focus on sagittal plane by posteromedial translation, however, results in more residual coronal and axial deformity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The generally accepted goals of surgery for adolescent idiopathic scoliosis are: avoiding further progression through solid fusion and correction of the deformity into a balanced configuration to restore postural balance [1, 2]. There is increasing evidence that successful restoration of a harmonious, balanced spine may have a protective effect on the unfused discs, as well as that a critical thoracic kyphosis is required to prevent sagittal plane deterioration and adding on, as well as proximal junctional kyphosis [3,4,5,6]. A common problem in posterior thoracic fusion for primary thoracic adolescent idiopathic scoliosis, however, is the flattening effect on the thoracic sagittal profile when derotation and coronal correction are performed [7, 8].
It is well known that AIS is a 3-D deformity of the spine, characterized by rotation, coronal deviation and apical lordosis (Fig. 1) [9,10,11,12]. Recently, Acaroglu et al. hypothesized that, due to an intrinsic component of AIS, posterior surgery cannot correct all three planes at the same time [13]. The anterior aspect of the rotated apex is longer than the posterior column in AIS. This length discrepancy is observed in the vertebral bodies, but mostly located in the discs [14]. In an attempt to surgically correct the coronal deviation and axial rotation, the additional anterior length, that has ‘escaped’ to the side, is rotated back to the midline, creating a thoracic hypokyphosis/lordosis at the level of the apex. The hypothesis by Acaroglu et al. has recently been confirmed by Hershkovitz et al.: They demonstrated that significant correction in the coronal plane is associated with postoperative hypokyphosis [13, 15]. Therefore, less significant coronal or axial correction may be required to achieve more kyphosis restoration.
There are distinct ‘schools’ for scoliosis surgery around the world with very different surgical strategies. Some surgeons perform primarily an apical axial derotation manoeuvre by different techniques of incremental rod bending and (in)direct vertebral derotation [7, 8, 16]. In contrast, others may focus primarily on the sagittal plane by translation techniques without apical concave instrumentation and avoid active derotation manoeuvres (Figs. 2 and 3). Because each strategy consists of correction manoeuvres that primarily provide correction in one plane or the other, different ‘schools’ make use of different implants and implant densities to achieve their goals. As far as the authors know, to date, no study has directly compared the effect of different strategies on the correction of the coronal, axial and sagittal spinal deformation in AIS.
An illustration of the ‘philosophy’ of the correction manoeuvres performed at each centre. In summary, the centre 3 mostly used a translation manoeuvre for main thoracic curve correction with sometimes concave laminar bands around the apex, whereas centre 1 (high implant density) and centre 2 (low implant density) relied on segmental derotation manoeuvres
The aim of this multinational study was to test the hypothesis that different strategies lead to different coronal and sagittal curve correction, and that there is an interaction between the correction of the deformity in the different planes. We retrospectively collected three consecutive cohorts in three major scoliosis centres that have different surgical strategies and evaluated the differences in coronal, axial and sagittal curve correction.
Materials and methods
Study population
Three consecutive series of patients who underwent posterior scoliosis surgery for primary thoracic AIS curves were retrospectively collected from three major scoliosis centres in the USA (centre 1), the Netherlands (centre 2) and France (centre 3). Centres were selected based on known differences in the philosophy for correction of the curvatures. All three centres perform more than 100 scoliosis surgeries annually. Patients were treated according to the local surgical expertise by two experienced surgeons per centre and were included if they had biplanar full-spine radiographs available at less than 3 months preoperative (baseline), before hospital discharge (postoperative) and at one or two year follow-up. While in centres 1 and 3, it was standard protocol to radiographically follow patients for at least 24 months postoperative, patients in centre 2 were radiographically followed for 15 months. Gender, age at surgery and the radiographic curve characteristics were recorded (Table 1). Patients with non-idiopathic scoliosis, other spinal pathology, known neural axis abnormalities on MRI, primary lumbar AIS, radiographs without the high thoracic levels visible or previous spinal surgery were excluded. This retrospective study was approved by the local institutional review boards.
Surgical cascade
The local surgeons described the different steps of their strategy in detail according to predefined criteria: use of pre-operative templating, patient positioning, implant type, implant density and implant strategy, ligamentous releases, rod contouring and order of insertion of the rods as well as their surgical technique (Table 1). In summary, centres 1 and 2 focused primarily on correcting the coronal and axial plane by different techniques of incremental rod bending and direct vertebral derotation, with pedicle screws around the apex. The difference in strategy between centres 1 and 2 is the implant density and rod insertion technique. Mean implant density was 100% in centre 1, and 60% in centre 2. Centre 1 started the correction on the convex side, centre 2 at the concave side. On the contrary, the surgeons in centre 3 focus primarily on the sagittal plane by a posteromedial translation technique without apical concave instrumentation and do not use active derotation manoeuvres. Concave laminar bands around the apex were added by one of the surgeons in centre 3.
Radiographic outcomes
Similar protocols for radiographic acquisition of digital, plain, full-length lateral radiographs (General Electric AL01F (General Electric, Schenectady, NY, USA); Philips Digital Diagnost (Philips B.V., Best, The Netherlands); Siemens VERTIX (Siemens, Erlangen, Germany); EOS (EOS imaging, SA, Paris, France) were used in the three centres. Acquisition was performed in an upright standing position with the hips, anterior superior iliac spines and shoulders perpendicular to the cassette, subjects were standing with their shoulders in 45° anteflexion and with their hips and knees straight, and they were instructed to stand in a comfortable manner and to look straight ahead with the hand on the zygoma’s or on the clavicles. Conventional coronal, sagittal and axial parameters of the instrumented main thoracic curve were measured using dedicated software (Surgimap®, Nemaris Inc.™, New York, NY, USA) by two observers and compared between the three strategies. Differences in pre- and first erect postoperative main thoracic spinal morphology were determined by coronal Cobb angle, axial rotation (Perdriolle method) and sagittal parameters (pelvic incidence, sacral slope, pelvic tilt, Roussouly types for spinopelvic alignment, T1-T12 and T4-T12 kyphosis, T10-L2 sagittal angle, C7 slope, Abelin-Genevois sagittal pattern, level of inflection point) [17]. For comparison of the effect of the different strategies on potential sagittal deterioration, proximal junctional angle (PJA, UIV – UIV + 2) was measured pre-operative and at latest available follow-up.
Statistical analysis
The statistical analyses were performed using statistical software SPSS 23 for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics were computed for the cohorts, providing means and standard deviations for continuous data, modus for ordinal data, and frequencies and percentages for binominal data. Comparison of demographic and outcome parameters between the different strategies was performed using one-way ANOVA for continuous data and Chi-square for ordinal data. For one-way ANOVA analyses a Bonferroni correction was applied for multiple testing. The level of statistical significance was set at P < 0.05.
Results
Demographics of the subjects in the three cohorts are shown in Table 1. Pre- and postoperative radiographic parameters are shown in Table 2. Pre-operative coronal curve magnitudes did not differ between the cohorts. Range of the coronal curve angles were 44–85°, 45–94° and 41–105°, respectively. In centre 1, 28 were Lenke type 1, 10 type 2 and 6 type 3. In centre 2, 24 were type 1, 10 type 2, 11 type 3 and 6 type 4. In centre 3, 60 were type 1, 19 type 2 and 19 type 3. Radiographs for curve flexibility were obtained in different positions in the participating centres and were therefore not included for comparison.
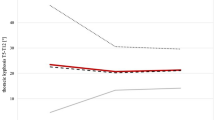
The strategy of centre 1 (derotation, high implant density, concave rod first) resulted in 75% coronal curve angle correction, compared to 70% in centre 2 (derotation, low implant density, convex rod first) and 59% in centre 3 (posterior translation) (Tables 2 and 3, P < 0.001). Apical rotation improved from 18° to 3°, 5° and 13° on average in the three centres, respectively. Pre- and postoperative pelvic incidence and Roussouly spinopelvic alignment types did not significantly differ between the cohorts. Patients in centre 1 had significantly larger preoperative T10-L2 lordosis and T4-T12 kyphosis as well as a larger number of hyperkyphotic patients, compared to centres 2 and 3. Despite similar postoperative T4-T12 kyphosis (22.4°, 21.7° vs. 20.6°, respectively), the strategy of centre 3 showed the most harmonious sagittal profile, because the strategy of centre 1 led to significantly more thoracolumbar lordosis (-7 ± 9°) compared to centre 3 (-4 ± 5). The strategy of centre 2 led to a higher inflection point (T11-12) compared to centres 1 and 3 (thoracolumbar junction). At follow-up, PJA was significantly higher and C7 slope lower in centres 1 and 2 as compared to centre 3 (Tables 2 and 3, P < 0.001).
Discussion
Comparison of the pre- and postoperative shape of the main thoracic curve between three different ‘schools’ for scoliosis surgery supports the hypothesis that significant coronal and axial correction tends to go at the detriment of the sagittal plane correction, and vice versa [13, 15]. From the AIS pathoanatomy follows that with greater coronal correction and axial derotation, there is relative anterior lengthening of the spine because the apical lordosis is derotated to the midsagittal plane. With limited kyphosis restoration, this could be a contributing factor to sagittal deterioration at the proximal junction of the instrumented spine at late follow-up.
The primary goal of scoliosis surgery has always been to prevent further progression and provide a balanced spine in the coronal and sagittal plane while fusing as few vertebrae as possible. There is evidence, however, that recreating a normal harmonious spine is beneficial to the remaining, unfused areas of the spine [3,4,5,6]. Even with modern day surgical implants, it remains difficult to recreate the normal shape of the adolescent spine and avoid problems like thoracic hypokyphosis and junctional decompensation [7, 8]. For corrective scoliosis surgery, thorough understanding of the three-dimensional pathoanatomy of the deformity could help to overcome the obstacles to reduction.
Lordotic deformation is together with rotation and lateral deviation an integral part of the complex three-dimensional deformity in AIS [9,10,11,12, 18]. Scoliosis surgery aims to correct the spinal deformation by combinations of corrections in the six degrees of freedom: translation, derotation and kyphosis restoration [16]. To achieve kyphosis recreation, different posterior releases are often used to allow for lengthening the posterior aspect of the spine. The strategies of centres 1 and 2 mostly relied on segmental derotation manoeuvres with pedicle screws around the apex. Theoretically, derotation of the apical lordosis back to the midline will lead to a compromise in the sagittal plane since it rotates the longer anterior column back to the midline and therefore induces a regional hypokyphosis (Fig. 4) [7, 8]. On the contrary, centre 3 primarily uses a translation manoeuvre, and no active derotation. Recently, concave sub-laminar bands around the apex were added in some patients to aim for more posterior translation of the apical area to recreate physiological global (T4-T12) thoracic kyphosis. This can only be achieved by shortening of the anterior column by compression of the anterior intervertebral discs and/or allowing the longer anterior column to stay deviated laterally and rotated. This technique may lead to a more harmonious sagittal profile by more kyphosis restoration, but leads to less coronal and axial correction.
Factors such as the coronal curve magnitude and flexibility, the use of hooks and implant density have all been implicated in the development of postoperative hypokyphosis. A randomized controlled trial that takes these confounders into account would be optimal to study the outcomes of specific correction strategies. In this retrospective experience-based cohort study, surgeons performed correction techniques in which they have expertise, with their preferred implants and implant strategy. An expertise-based RCT, where patients are not randomized for different treatments by one surgeon, but randomized to surgeons that only deliver the technique in which they have expertise, has been proposed as an alternative for surgical RCT’s. Randomization of an AIS patient for surgeons performing their own technique seems theoretically possible, except for the fact that different surgical strategies are often topographically bound.
The aim of this study was not to compare the differences in clinical outcomes of different correction techniques, but to better understand the interaction between the correction of the triplanar deformity in AIS. Recently, Herzkovich et al. demonstrated that focus on correction in the coronal plane is associated with difficulties in restoring normal alignment in the sagittal plane. In the present retrospective study, patients were not matched based on their preoperative sagittal parameters. Preoperatively, the fundamental parameter pelvic incidence and Roussouly spino-pelvic alignment types were comparable between the centres. In centre 1, however, more patients were hypokyphotic and the mean T10-L2 angle was smaller (more lordosis). The lack of comparability of all preoperative sagittal parameters may give risk of type-1-error and is a limitation of this retrospective study. Postoperatively, we observed that the two centres that primarily use apical derotation experience difficulties in re-creating neutral sagittal alignment of the thoracolumbar junction or inflection point. Despite the preoperative differences, we assume that this could be explained by the effect of derotation. The translation strategy in centre 3 was more successful for the sagittal plane then in the coronal plane correction compared to centres 1 and 2. Long-term radiographic follow-up was not available for all patients, but we observed that the proximal junctional kyphosis angles at standard radiographic follow-up after surgery (15 months to 2 years) were smaller and C7 slope larger in centre 3. Pelvic tilt remained comparable. The effect of the different strategies on the chest as well as whether the difference in coronal and sagittal plane curve correction has an impact on the clinical outcome for patients cannot be derived from this comparative study and needs further investigation to provide recommendations.
In conclusion, based on comparison of three different ‘scoliosis schools’, it seems that derotational strategies lead to more coronal and axial correction as compared to a posteromedial translation strategy. Apical derotation, however, inevitably leads to difficulties in re-creating kyphosis in the apical region and may be a risk factor for iatrogenic thoracolumbar lordosis, a non-physiological inflection point, and therefore proximal junctional problems. A posterior and medial translation manoeuvre, however, often results in a sagittal harmonious spine, but significantly less coronal and axial correction. Therefore, in scoliosis surgery, an emphasis on obtaining the best possible result in whichever plane, by the nature of the disorder, automatically leads to a compromise in the other planes. Of course, awareness of this coupling of the outcomes in all three planes has led to modifications of each strategy, mostly sacrificing some correction in the other planes. The effect of extensive releases, implant strategies (such as stronger and stiffer rods) and more emphasis on recreating a patient specific harmonious kyphosis needs to be investigates by modern 3-D imaging techniques that allow for study of the correction of AIS in more detail.
References
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371:1527–1537. https://doi.org/10.1016/S0140-6736(08)60658-3
de Kleuver M, Lewis SJ, Germscheid NM, Kamper SJ, Alanay A, Berven SH et al (2014) Optimal surgical care for adolescent idiopathic scoliosis: an international consensus. Eur Spine J 23:2603–2618. https://doi.org/10.1007/s00586-014-3356-1
Abelin-Genevois K, Estivalezes E, Briot J, Sevely A, Sales de Gauzy J, Swider P (2015) Spino-pelvic alignment influences disc hydration properties after AIS surgery: a prospective MRI-based study. Eur Spine J 2015(24):1183–1190. https://doi.org/10.1007/s00586-015-3875-4
Akazawa T, Kotani T, Sakuma T, Minami S, Orita S, Fujimoto K et al (2017) Spinal fusion on adolescent idiopathic scoliosis patients with the level of L4 or lower can increase lumbar disc degeneration with sagittal imbalance 35 years after surgery. Spine Surg Relat Res 1:72–77. https://doi.org/10.22603/ssrr.1.2016-0017
Ilharreborde B (2018) Sagittal balance and idiopathic scoliosis: does final sagittal alignment influence outcomes, degeneration rate or failure rate? Eur Spine J 27:48–58. https://doi.org/10.1007/s00586-018-5472-9
Mimura T, Ikegami S, Oba H, Uehara M, Koseki M, Takahashi J (2019) Factors leading to postoperative pain in adolescent idiopathic scoliosis patients including sagittal alignment and lumbar disc degeneration. Eur Spine J 28:3085–3091. https://doi.org/10.1007/s00586-019-06152-5
Hayashi K, Upasani VV, Pawelek JB, Aubin CE, Labelle H, Lenke LG, et al. (2009) Three-dimensional analysis of thoracic apical sagittal alignment in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 34:792–797. doi: https://doi.org/10.1097/BRS.0b013e31818e2c36
Mladenov KV, Vaeterlein C, Stuecker R (2011) Selective posterior thoracic fusion by means of direct vertebral derotation in adolescent idiopathic scoliosis: effects on the sagittal alignment. Eur Spine J 20:1114–1117. https://doi.org/10.1007/s00586-011-1740-7
Roaf R (1966) The basic anatomy of scoliosis. J Bone Joint Surg Br 48:786–792
Deacon P, Flood BM, Dickson RA (1984) Idiopathic scoliosis in three dimensions. A radiographic and morphometric analysis. J Bone Joint Surg Br 66:509–512
Newton PO, Fujimori T, Doan J, Reighard FG, Bastrom TP, Misaghi A (2015) Defining the “Three-Dimensional Sagittal Plane” in Thoracic Adolescent Idiopathic Scoliosis. J Bone Joint Surg Am 97:1694–1701. https://doi.org/10.2106/JBJS.O.00148
Schlosser TP, van Stralen M, Chu WC, Lam TP, Ng BK, Vincken KL et al (2016) Anterior overgrowth in primary curves, compensatory curves and junctional segments in adolescent idiopathic scoliosis. PLoS ONE 11:e0160267. https://doi.org/10.1371/journal.pone.0160267
Acaroglu E, Doany M, Cetin E, Castelein R (2019) Correction of rotational deformity and restoration of thoracic kyphosis are inversely related in posterior surgery for adolescent idiopathic scoliosis. Med Hypotheses 133:109396. https://doi.org/10.1016/j.mehy.2019.109396
Schlosser TP, van Stralen M, Brink RC, Chu WC, Lam TP, Vincken KL et al (2014) Three-dimensional characterization of torsion and asymmetry of the intervertebral discs versus vertebral bodies in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 39:E1159–1166. https://doi.org/10.1097/BRS.0000000000000467
Hershkovich O, D'Souza A, Rushton PRP, Onosi IS, Yoon WW, Grevitt MP (2020) Essential lordosis revisited. Bone Joint J. 102-B:513–518. https://doi.org/10.1302/0301-620X.102B4.BJJ-2019-1069.R1
Shah SA (2007) Derotation of the spine. Neurosurg Clin N Am 18:339–345. https://doi.org/10.1016/j.nec.2007.02.003
Abelin-Genevois K, Sassi D, Verdun S, Roussouly P (2018) Sagittal classification in adolescent idiopathic scoliosis: original description and therapeutic implications. Eur Spine J 27:2192–2202. https://doi.org/10.1007/s00586-018-5613-1
Pasha S, Hassanzadeh P, Ecker M, Ho V (2019) A hierarchical classification of adolescent idiopathic scoliosis: Identifying the distinguishing features in 3D spinal deformities. PLoS ONE 14:e0213406. https://doi.org/10.1371/journal.pone.0213406
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors has any potential conflict of interest
Competing interests
One or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article:
IRB approval
This study was reviewed by a local IRB using expedited review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schlösser, T.P., Abelin-Genevois, K., Homans, J. et al. Comparison of different strategies on three-dimensional correction of AIS: which plane will suffer?. Eur Spine J 30, 645–652 (2021). https://doi.org/10.1007/s00586-020-06659-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06659-2