Abstract
Purpose
The aim of this study was to elucidate normative features of vagal motor-evoked potentials (MEPs) induced by transcranial electrical stimulation (TES) and to determine the influence of functional decline of the recurrent laryngeal nerve (RLN) on vagal MEPs during thyroid surgery.
Methods
A total of 54 patients undergoing elective thyroid surgery under general anesthesia were enrolled in this study. Vagal MEPs induced by TES were measured from the vocal cord using one of two types of electrodes (wire type or wide and flat type) mounted on an endotracheal tube. We investigated the effects of stimulation intensity and train pulse number on vagal MEP amplitude, the time course of vagal MEP amplitude during surgery, and the effects of functional decline of the RLN on vagal MEPs.
Results
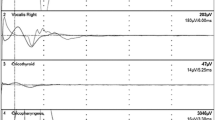
The success rate of vagal MEP monitoring with wide- and flat-type electrodes was significantly higher than that with wire-type electrodes. Reliable vagal MEPs were obtained at a stimulation intensity of approximately 300 V with 3 or more pulses in 91% of the patients without preoperative RLN palsy (RLNP), and the amplitude was augmented with increasing stimulation intensity and train pulse number. Vagal MEP amplitude decreased during thyroid surgery and then partially recovered at the end of surgery. Vagal MEP amplitude recorded from the electrode ipsilateral to preoperative RLNP was significantly lower than that on the contralateral intact side.
Conclusion
Vagal MEPs induced by TES can be obtained with a high success rate during thyroid surgery and would reflect functional status of the RLN.







Similar content being viewed by others
References
Macdonald DB, Skinner S, Shils J, Yingling C. Intraoperative motor evoked potential monitoring—a position statement by the American Society of Neurophysiological Monitoring. Clin Neurophysiol. 2013;124:2291–316.
Akagami R, Dong CC, Westerberg BD. Localized transcranial electrical motor evoked potentials for monitoring cranial nerves in cranial base surgery. Neurosurgery. 2005;57(Suppl 1):78–85.
Sala F, Manganotti P, Tramontano V, Bricolo A, Gerosa M. Monitoring of motor pathways during brain stem surgery: what we have achieved and what we still miss? Neurophysiol Clin. 2007;37:399–406.
Ito E, Ichikawa M, Itakura T, Ando H, Matsumoto Y, Oda K, Sato T, Watanabe T, Sakuma J, Saito K. Motor evoked potential monitoring of the vagus nerve with transcranial electrical stimulation during skull base surgeries. J Neurosurg. 2013;118:195–201.
Fukuda M, Oishi M, Hiraishi T, Saito A, Fujii Y. Pharyngeal motor evoked potentials elicited by transcranial electrical stimulation for intraoperative monitoring during skull base surgery. J Neurosurg. 2012;116:605–10.
Erman AB, Kejner AE, Hogikyan ND, Feldman EL. Disorders of cranial nerves IX and X. Semin Neurol. 2009;29:85–92.
Schlake HP, Goldbrunner RH, Milewski C, Krauss J, Trautner H, Behr R, Sörensen N, Helms J, Roosen K. Intra-operative electromyographic monitoring of the lower cranial motor nerves (LCN IX–XII) in skull base surgery. Clin Neurol Neurosurg. 2001;103:72–82.
Morota N, Deletis V, Epstein FJ, Kofler M, Abbott R, Lee M, Ruskin K. Brain stem mapping: neurophysiological localization of motor nuclei on the floor of the fourth ventricle. Neurosurgery. 1995;37:922–30.
Yang S, Zhou L, Lu Z, Ma B, Ji Q, Wang Y. Systematic review with meta-analysis of intraoperative neuromonitoring during thyroidectomy. Int J Surg. 2017;39:104–13.
Brajcich BC, McHenry CR. The utility of intraoperative nerve monitoring during thyroid surgery. J Surg Res. 2016;204:29–33.
Rödel RM, Olthoff A, Tergau F, Simonyan K, Kraemer D, Markus H, Kruse E. Human cortical motor representation of the larynx as assessed by transcranial magnetic stimulation (TMS). Laryngoscope. 2004;114:918–22.
Deletis V, Fernandez-Conejero I, Ulkatan S, Costantino P. Methodology for intraoperatively eliciting motor evoked potentials in the vocal muscles by electrical stimulation of the corticobulbar tract. Clin Neurophysiol. 2009;120:336–41.
Lu IC, Chu KS, Tsai CJ, Wu CW, Kuo WR, Chen HY, Lee KW, Chiang FY. Optimal depth of NIM EMG endotracheal tube for intraoperative neuromonitoring of the recurrent laryngeal nerve during thyroidectomy. World J Surg. 2008;32:1935–9.
Dionigi G, Bacuzzi A, Boni L, Rovera F, Dionigi R. What is the learning curve for intraoperative neuromonitoring in thyroid surgery? Int J Surg. 2008;6(Suppl 1):7–12.
Kim HY, Tufano RP, Randolph G, Barczyński M, Wu CW, Chiang FY, Liu X, Masuoka H, Miyauchi A, Park SY, Kwak HY, Lee HY, Dionigi G, Korean Intraoperative Neural Monitoring Society (KINMoS). Impact of positional changes in neural monitoring endotracheal tube on amplitude and latency of electromyographic response in monitored thyroid surgery: results from the Porcine Experiment. Head Neck. 2016;38(Suppl 1):E1004–8.
Dong CC, Macdonald DB, Akagami R, Westerberg B, Alkhani A, Kanaan I, Hassounah M. Intraoperative facial motor evoked potential monitoring with transcranial electrical stimulation during skull base surgery. Clin Neurophysiol. 2005;116:588–96.
Randolph GW, Dralle H, with the International Intraoperative Monitoring Study Group, Abdullah H, Barczynski M, Bellantone R, Brauckhoff M, Carnaille B, Cherenko S, Chiang FY, Dionigi G, Finck C, Hartl D, Kamani D, Lorenz K, Miccolli P, Mihai R, Miyauchi A, Orloff L, Perrier N, Poveda MD, Romanchishen A, Serpell J, Sitges-Serra A, Sloan T, Van Slycke S, Snyder S, Takami H, Volpi E, Woodson G. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011;121(Suppl 1):1–16.
Snyder SK, Sigmond BR, Lairmore TC, Govednik-Horny CM, Janicek AK, Jupiter DC. The long-term impact of routine intraoperative nerve monitoring during thyroid and parathyroid surgery. Surgery. 2013;154:704–13.
Rickett T, Connell S, Bastijanic J, Hegde S, Shi R. Functional and mechanical evaluation of nerve stretch injury. J Med Syst. 2011;35:787–93.
Barczyński M, Randolph GW, Cernea CR, Dralle H, Dionigi G, Alesina PF, Mihai R, Finck C, Lombardi D, Hartl DM, Miyauchi A, Serpell J, Snyder S, Volpi E, Woodson G, Kraimps JL, Hisham AN, with the International Neural Monitoring Study Group. External branch of the superior laryngeal nerve monitoring during thyroid and parathyroid surgery: International Neural Monitoring Study Group standards guideline statement. Laryngoscope. 2013;123(Suppl 4):1–14.
Mikuni N, Satow T, Taki J, Nishida N, Enatsu R, Hashimoto N. Endotracheal tube electrodes to map and monitor activities of the vagus nerve intraoperatively. Technical note. J Neurosurg. 2004;101:536–40.
Eisele DW. Intraoperative electrophysiologic monitoring of the recurrent laryngeal nerve. Laryngoscope. 1996;106:443–9.
Hayward NJ, Grodski S, Yeung M, Johnson WR, Serpell J. Recurrent laryngeal nerve injury in thyroid surgery: a review. ANZ J Surg. 2013;83:15–21.
Malik R, Linos D. Intraoperative neuromonitoring in thyroid surgery: a systematic review. World J Surg. 2016;40:2051–8.
Lombardi CP, Carnassale G, Damiani G, Acampora A, Raffaelli M, De Crea C, Bellantone R. “The final countdown”: is intraoperative, intermittent neuromonitoring really useful in preventing permanent nerve palsy? Evidence from a meta-analysis. Surgery. 2016;160:1693–706.
Chan WF, Lo CY. Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg. 2006;30:806–12.
Thomusch O, Sekulla C, Machens A, Neumann HJ, Timmermann W, Dralle H. Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg. 2004;389:499–503.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The present research was supported solely by hospital and department sources. None of the authors have any financial interests in products related to this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ichino, T., Tanaka, S., Tanaka, R. et al. Transcranial motor-evoked potentials of laryngeal muscles for intraoperative neuromonitoring of the vagus nerve during thyroid surgery. J Anesth 33, 221–229 (2019). https://doi.org/10.1007/s00540-018-2601-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-018-2601-x