Abstract
Purpose
This observational study was designed to evaluate the clinical value of cardiac output (CO) obtained via bioreactance (NICOM™) as compared with values of CO obtained via thermodilution (using pulmonary artery catheter, Vigilance™) and the thoracic bioimpedance (BioZ.com™), in patients undergoing off-pump coronary artery bypass surgery.
Methods
Fifty American Society of Anesthesiologists physical status I–III patients, aged 38–81 years, scheduled for off-pump coronary artery bypass surgery were enrolled in this study. CO data (NCO, BCO, PCO) were recorded during the operative period at ten time points after stable hemodynamic conditions were achieved.
Results
The equation of the relationship between the PCO and NCO is PCO = 0.945 × NCO + 0.328 (r = 0.77), and that of PCO and BCO is PCO = 0.965 × BCO + 0.729 (r = 0.63). Furthermore, no statistical difference was found between PCO versus NCO (mean (SD): 4.4 (1.1) versus 4.4 (0.9), p = 0.431). A significant correlation was found between PCO and NCO (r = 0.77, p < 0.001). Correlation was also found between PCO and BCO (r = 0.63, p < 0.001).
Conclusions
The NICOM device is a safe, convenient, and reliable device for measuring continuous non-invasive cardiac output and cardiac index, and the trends of change in CO during the surgery are similar between NICOM and PAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac output and cardiac index are key parameters of hemodynamics and can be used to evaluate cardiac pump function and calculate other parameters like SVR or PVR and so on. In patients undergoing cardiac surgery, thermodilution using a pulmonary artery catheter (PAC) is still the reference gold standard. However, although the incidence of complications with the PAC is relatively low, the technique is still quite invasive and up to now, there is no clear evidence of improved outcomes associated with its insertion and use to guide therapy [1–5]. Therefore, several less-invasive methods have been proposed [6, 7]. Non-invasive methods could be preferable, especially for low-risk patients in whom CO monitoring is increasingly used nowadays, as non-invasive methods have fewer side effects as compared to invasive procedures. One of these non-invasive methods is thoracic bioimpedance, which analyzes intrabeat variations of transthoracic voltage in response to an input high-frequency current; however, inconsistent measurements were found in intensive care [8, 9, 16].
Recently, a new signal-processing method has been developed which is called NICOM. Its signal is based on the frequency modulation and phase modulation of the output voltage. This advanced bioreactance technology improves the signal-to-noise ratio 100-fold. However, the accuracy of NICOM has not been confirmed, especially when compared with the PAC technique in patients undergoing off-pump coronary artery bypass surgery. Therefore, we conducted the following investigation.
The aim of this study was to evaluate the accuracy of CO measured by NICOM in patients undergoing off-pump coronary artery bypass surgery, and to compare the results with the other two devices: (1) the BioZ.com™ system with thoracic bioimpedance, and (2) continuous CO monitoring using a PAC with thermodilution.
Patients and methods
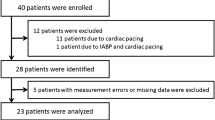
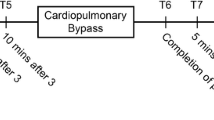
Patients undergoing off-pump coronary artery bypass surgery gave their informed consent to the study, which was approved by the Ethics Committee of Shanghai Ruijin Hospital (2013/NO.69). Inclusion criteria were ASA I–III or NYHA I–II. A total of 50 patients were recruited for the current study with the insertion of PAC. When the patients arrived in the operating room, they were connected to patient with the NICOM and the BioZ.com placed on the each side of the thorax. The CO data and standard hemodynamic data (HR, MAP, SV, and SVI) from all devices were record by an observer who was not responsible for the patient’s anesthesia. The measurements were free of interference from surgery or infusion boluses (such as Ringer’s solution and succinylated gelatin or vasoactive agents). Predefined measurement points were: T1 = immediate after induction of anesthesia (study initiation), T2 = 5 min post-induction, T3 = 10 min post-induction, T4 = sternotomy, T5 = 5 min post-sternotomy, T6 = 10 min post-sternotomy, T7 = opening of pericardial, T8 = pericardial closure, T9 = sternal closure, T10 = 5 min post-sternal closure.
Statistics
Data are expressed as mean (SD) or median (range) for non-normally distributed variables or number and percentage as appropriate. CO values obtained from NICOM and PAC or BioZ.com and PAC were also using ANOVA. The correlation of CO was determined by linear regression. The Bland–Altman analysis was used to compare bias and limits of agreement.
A p value of 0.05 was considered as statistically significant and all p values were two-tailed. Statistical analysis was done by using SPSS for Windows Release 20.0 (SPSS Inc., Chicago, IL, USA).
Results
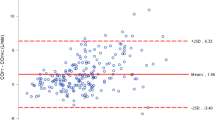
Baseline characteristics for the 50 subjects are indicated in Table 1. No statistical difference was found between PCO versus NCO (p = 0.431) (Table 2). Figure 1a shows the relationship of CO data between PAC and NICOM; the equation of the relationship is PCO = 0.945 × NCO + 0.328 (r = 0.77). Figure 1b shows the relationship of CO data between PAC and Bioz.com; the equation of the relationship is PCO = 0.965 × BCO + 0.729 (r = 0.63). Figure 2 shows the variations in CO for PAC, NICOM and BioZ.com in different measurement points during the surgery. PCO and NCO increase at a slower rate from T1 to T7 but increase at a faster rate from T8 to T10, whereas BCO increases gradually from T1 to T10. The Bland–Altman analysis was used to compare the bias, precision (SD of bias), and limits of agreement [bias (1.96 SD)]. The bias and limits of agreement of CO between PAC and NICOM are depicted in Fig. 3a and the bias and limits of agreement of CO between PAC and BioZ.com are depicted in Fig. 3b.
Discussion
Our study shows that NICOM is convenient and safe in a clinical setting, as it only requires the placement of two double electrodes on the patient’s thorax. Correlation coefficient of PCO and NCO (r = 0.77) is better than those of PCO with BCO (r = 0.63). Although NICOM up to now cannot replace the use of PAC, it provides consistent continuous non-invasive measurements of CO and CI and seems to be able to track in real time the trends and the change with the time. There is literature that suggests that real-time tracking of the trends of change in CO could be more important than the ability of the monitor to deliver a highly accurate single measurement under stable conditions [10]. In the current study, the trends of change in CO during the surgery are similar among the three devices, and the trends by NICOM are closer to PAC than by BioZ.com (Fig. 2). From Fig. 3a we can deduce that for values of CO between 4 and 6 NICOM and PAC values have a good correlation. For values of CO below 4, NICOM overestimates values of CO as compared to PAC. For values of cardiac output above 6, NICOM underestimates values of CO as compared to PAC. Similarly, from Fig. 3b we can deduce that for values of CO between 4 and 6, BioZ.com and PAC values have a good correlation. For values of CO below 4, BioZ.com overestimates values of CO as compared to PAC. For values of CO above 6, BioZ.com underestimates values of CO as compared to PAC.
As an invasive hemodynamic monitor, PAC was regarded as a gold standard of reference because we have no better reference for continuous CO monitoring [11–14]. We therefore compared the relationship between non-invasive cardiac output monitor (NICOM) with PAC. In the current study, we are still not sure if NICOM can replace the PAC as a means to measure CO. A meta-analysis study literature also showed that none of the four tested alternative methods (pulse contour analysis, esophageal Doppler, thoracic electrical bioimpedance) achieved agreement with PAC [15]. However, considering that the scope of PAC’s applicability is limited, and that it also brings a lot of risks and complications (e.g., infection) [20], the clinical hemodynamic monitoring is moving towards less invasive or even non-invasive methods.
Bioimpedance is based on the fact that the conductivity of a high-frequency, low-magnitude alternating current passed through the thorax changes as blood flow varies with each cardiac cycle. These changes can be measured using electrodes placed on a patient’s chest and used to generate a waveform from which cardiac output can be calculated. However, its accuracy is always in doubt, as the technique has its own limitation [16].
Bioreactance is developed out of bioimpedance and measures changes in the frequency of the electrical currents traversing the chest, rather than changes in impedance, potentially making it less sensitive to noise [17, 18]. Also, bioreactance-based NICOM has acceptable accuracy in challenging clinical environments [19]. Furthermore, one study suggests that NICOM can be clinically valid when used in ICU patients [21, 22], but the accuracy of NICOM and Bioz.com have not been confirmed, especially compared with the PAC technique in patients undergoing off-pump coronary artery bypass surgery. This is why we compare the three devices to evaluate the accuracy of CO measurements in patients undergoing off-pump coronary artery bypass surgery. The measurement points in this study were defined according to clinical importance of surgical step, as they are also very common in cardiac surgery.
The limitations of the current study are as follows: Firstly, all the data for the patient group were collected after induction of anesthesia. PAC values before anesthesia are unavailable, because we abstained from placing a PAC in the patient who is awake so as not to further increase discomfort before surgery. Secondly, the study was limited only to patients undergoing cardiac surgery and did not take into account post-surgical patients in the ICU. Thirdly, the current study did not evaluate the ability of the NICOM to predict fluid responsiveness.
In conclusion, the NICOM is a safe, convenient device, and reliable to continuously and non-invasively monitoring cardiac output and cardiac index, and could track the trend of changes under dynamic conditions. Although the device cannot replace PAC for patients undergoing off-pump coronary artery bypass surgery at present stage, it may potentially be used in a wide range such as during laparoscopic surgery or for the patients with heart diseases undergoing non-cardiac surgery, when invasive monitoring is not an option or not desired.
References
Connors AF Jr, Speroff T, Dawson NV, Thomas C, Harrell FE Jr, Wagner D, Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson WJ Jr, Vidaillet H, Broste S, Bellamy P, Lynn J, Knaus WA. The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA. 1996;276:889–97.
Guyatt G. A randomized control trial of right-heart catheterization in critically ill patients. Ontario Intensive Care Study Group. Intensive Care Med. 1991;6:91–5.
Sandham JD, Hull RD, Brant RF, Knox L, Pineo GF, Doig CJ, Laporta DP, Viner S, Passerini L, Devitt H, Kirby A, Jacka M. A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. N Engl J Med. 2003;348:5–14.
Takala J. The pulmonary artery catheter: the tool versus treatments based on the tool. Crit Care. 2006;10:162.
Shah MR, Hasselblad V, Stevenson LW, Binanay C, O’Connor CM, Sopko G, Califf RM. Impact of the pulmonary artery catheter in critically ill patients: meta-analysis of randomized clinical trials. JAMA. 2005;294:1664–70.
Sphör F, Hettrich P, Hass H, Martin E, Böttiger BW. Comparison of two methods for enhanced continuous circulatory monitoring in patients with septic shock. Intensive Care Med. 2007;33:1805–10.
De Wilde RB, Schreuder JJ, van den Berg PC, Jansen JR. An evaluation of cardiac output by five arterial pulse contour techniques during cardiac surgery. Anaesthesia. 2007;62:760–8.
Leslien S, McKee S, Newby D, Webb D, Denvir M. Non-invasive measurement of cardiac output in patients with chronic heart failure. Blood Press Monit. 2004;9:277–80.
Engoren M, Barbee D. Comparison of cardiac output determined by bioimpedance, thermodilution, and the Fick method. Am J Crit Care. 2005;14:40–5.
Critchley LA, Lee A, Ho AM. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–92.
Boldt J, Menges T, Menges T, Wollbruck M, Hammermann H, Hempelmann G. Is continuous cardiac output measurement using thermodilution reliable in the critically ill patient? Crit Care Med. 1994;22:1913–8.
Haller M, Zollner C, Briegel J, Forst H. Evaluation of a new continuous thermodilution cardiac output monitor in critically ill patients: a prospective criterion standard study. Crit Care Med. 1995;23:860–6.
Nelson LD. The new pulmonary artery catheters: continuous venous oximetry, right ventricular ejection fraction, and continuous cardiac output. Crit Care Clin. 1996;12:795–818.
Mihm FG, Gettinger A, Han son C, Gilbert HC, Stover EP, Vender JS, Beerle B, Haddow G. A multicenter evaluation of a new continuous cardiac output pulmonary artery catheter system. Crit Care Med. 1998;26:1346–50.
Peyton PJ, Chong SW. Minimally invasive measurement of cardiac output during surgery and critical care. Anesthesiology. 2010;113:1220–35.
Hirschl MM, Kittler H, Woisetchläger C, Siostrzonek P, Staudinger T, Kofler J, Oschatz E, Bur A, Gwechenberger M, Laggner AN. Simultaneous comparison of thoracic bioimpedance and arterial pulse waveform-derived cardiac output with thermodilution measurement. Crit Care Med. 2000;28:1798–802.
Keren H, Burkhoff D, Squara P. Evaluation of a non-invasive continuous cardiac output monitoring system based on thoracic bioreactance. Am J Physiol. 2007;293:583–9.
Squara P, Rotcajg D, Denjean D, Estagnasie P, Brusset A. Comparison of monitoring performance of bioreactance vs. pulse contour during lung recruitment maneuvers. Crit Care. 2009;13:R125.
Raval NY, Squara P, Cleman M, Yalamanchili K, Winklmaier M, Burkhoff D. Multicenter evaluation of noninvasive cardiac output measurement by bioreactance technique. J Clin Monit Comput. 2008;22:113–9.
Schwann NM, Hillel Z, Hoeft A, Barash P, Möhnle P, Miao Y, Mangano DT. Lack of effectiveness of the pulmonary artery catheter in cardiac surgery. Anesth Analg. 2011;133:994–1002.
Marik PE, Levitov A, Young A, Andrews L. The use of bioreactance and carotid Doppler to determine volume responsiveness and blood flow redistribution following passive leg raising in hemodynamically unstable patients. Chest. 2013;143:364–70.
Brahim B, Ouattara A, Estagnasie P, Brusset A, Squara P. Fluid responsiveness predicted by noninvasive bioreactance-based passive leg raise test. Intensive Care Med. 2010;36:1875–81.
Acknowledgments
The authors thank the company Cheetah Medical (Wilmington, DE, USA) for kindly providing the facilities necessary for hemodynamic monitoring with the NICOM device. The manufacturer had no conduct of the study or in the decision to submit the manuscript for publication.
Conflict of interest
The authors have no competing interests to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Cheung, H., Dong, Q., Dong, R. et al. Correlation of cardiac output measured by non-invasive continuous cardiac output monitoring (NICOM) and thermodilution in patients undergoing off-pump coronary artery bypass surgery. J Anesth 29, 416–420 (2015). https://doi.org/10.1007/s00540-014-1938-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1938-z