Abstract
Objective
To compare a modified pulmonary artery catheter (PAC) and pulse-contour analysis by the PiCCO (Pulsion Medical Systems, Munich, Germany) system for continuous assessment of cardiac output in patients with septic shock. In addition, to assess the relationships between an index of global end-diastolic volume (GEDV) derived by the PiCCO system with traditional PAC-derived indicators of filling: central venous pressure; pulmonary artery occlusion pressure; and right ventricular end-diastolic volume (RVEDV).
Design
Prospective cohort study.
Setting
Surgical intensive care unit of a university hospital.
Patients and participants
14 patients with septic shock.
Interventions
None.
Measurements and results
A significant correlation was found between continuous cardiac output by PAC (CCOPAC) and by pulse-contour analysis (r 2 = 0.714, p < 0.0001), accompanied by a bias of 0.1 l min−1 and a precision of 2.7 l min−1. The correlation between CCOPAC and cardiac output measured by transcardiopulmonary thermodilution was also significant (r 2 = 0.781, p < 0.0001). There was a bias for the two methods of 0.2 l min−1, and a precision of 2.2 l min−1. The GEDV showed no correlation with central venous pressure, pulmonary artery occlusion pressure, or RVEDV.
Conclusion
In patients with septic shock, the averaged bias in continuous measurement of cardiac output by both a modified pulmonary artery catheter and pulse-contour analysis was small, but variability was large. No correlation was found between GEDV and RVEDV. The clinical importance of different cardiac filling parameters needs further investigation.
Similar content being viewed by others
Introduction
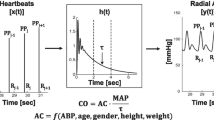
Reliable bedside measurement of cardiac output is desirable for purposeful interventions in patients with septic shock. Although intermittent measurement of cardiac output using a pulmonary artery catheter has widely been accepted as the clinical reference method [1], intermittent techniques may not provide sufficient information for long periods throughout a day in patients with septic shock who are frequently haemodynamically unstable. In addition, intermittent measurements using cold fluid boli may cause bacterial contamination [2] or fluid overload in fluid-sensitive patients. The pulsed warm thermodilution technique uses a modified pulmonary artery catheter and allows continuous or semi-continuous assessment of cardiac output, right ventricular ejection fraction (RVEF) and right ventricular end-diastolic volume (RVEDV) [3–5]. Because right ventricular function may be the limiting factor in determining cardiac output in patients with septic shock [6], this technique may be advantageous in septic patients; however, since this invasive procedure may be infrequently associated with severe complications [7], less invasive techniques for monitoring of cardiac output may be an attractive alternative. The PiCCO system, which uses transpulmonary thermodilution for calibration, is regarded as being less invasive because it only requires the placement of a central venous and arterial catheter, which are routinely used in critically ill patients [8].
Traditionally, central venous pressure (CVP) and pulmonary artery occlusion pressure (PAOP) have been considered to be measures of right and left ventricular preload; however, it has become increasingly clear that a poor correlation between these filling pressures and ventricular preload may be found under experimental [9] and clinical [10] conditions, even in healthy subjects [11]. In contrast, end-diastolic volume estimates are supposed to be better indicators for the degree of myocardial fibre stretch, i.e. cardiac preload according to the Frank-Starling law [10, 11]. The RVEDV has been demonstrated to reflect cardiac preload in critically ill patients [12], although the clinical usefulness of this variable has not been conclusively elucidated. The PiCCO system is able to calculate another global parameter for cardiac preload, the global end-diastolic volume (GEDV). The GEDV has recently been demonstrated to reflect cardiac filling in patients with septic shock [13].
In this prospective study, we compared the PiCCO system and the modified pulmonary artery catheter in patients with septic shock. The specific goals of the study were to: (a) study the reliability and accuracy of the PiCCO system compared with the modified pulmonary artery catheter with regard to continuous monitoring of cardiac output; (b) define a correlation between RVEDV and GEDV and the widely used cardiac filling pressures (CVP and PAOP); and (c) determine a correlation between the two preload variables, RVEDV and GEDV.
Patients and methods
This prospective study was conducted in a surgical 14-bed ICU in a university hospital. The study protocol was approved by the local ethics committee, and written informed consent was obtained by the legal representatives of each patient.
We studied 14 patients with septic shock as defined by the criteria of the International Sepsis Definitions Conference in 2001 [14]. All patients were equipped with a central venous catheter (jugular or subclavian), a modified pulmonary artery catheter inserted in the right jugular vein (774HF75, Edwards Lifesciences, Irvine, Calif.), and a 4-F thermistor-tipped arterial catheter (PV2015L13, Pulsion Medical Systems, Munich, Germany), which was inserted in the left femoral artery and advanced to the abdominal aorta. All patients received mechanical ventilation, vasopressor therapy (norepinephrine 0.1–0.7 μg/kg min−1) and inotropic support by epinephrine (0.1–0.5 μg/kg min−1, 9 patients) and/or dobutamine (3–10 μg/kg min−1, 10 patients). Ventilator settings and infusion rates of catecholamines were adapted by the attending physician according to clinical requirements.
Haemodynamic measurements
Patients were studied in a supine position. During haemodynamic measurement, the dose of catecholamines was maintained constantly, and no additional fluids were given. Central venous pressure (CVP) and pulmonary artery occlusion pressure (PAOP) were measured at end-expiration. Continuous assessment of cardiac output (CCOPAC) and right ventricular end-diastolic volume (RVEDV) were performed using a modified pulmonary artery catheter thermodilution technique described elsewhere [3–5]. Continuous cardiac output using pulse contour analysis was measured by the PiCCOplus system (version 5.2.2, Pulsion Medical Systems, Munich, Germany). Cardiac output measured by transcardiopulmonary thermodilution (COTCP) and GEDV were determined discontinuously by thermodilution using a triplicate injection of 15 ml ice-cold saline administered through the central venous catheter. This method has also been described elaborately elsewhere [8, 15].
Study protocol
Measurements were started when diagnostic criteria of septic shock were fulfilled, i.e. when persistent arterial hypotension unexplained by other causes occurred [14]. All haemodynamic measurements were recorded hourly in a time period when no significant arrhythmias or haemodynamic instability were present. Measurement of CCOPCCO was performed 30 min after assessment of COTCP by averaging three measurements of CCOPCCO taken within 3 min. Single measurements were repeated if deviation between two measurements was more than 20%. Ventilator settings, volume resuscitation and infusion rates for catecholamines were controlled at the attending physician's discretion. Data recording was terminated when the patient required no more catecholamines. To minimize patients' effects due to unequal numbers of measurement among the patients, data points from each patient were randomly selected until the number of data points selected equalled the number of measurements in the patient with the fewest number. By this means, 13 data points per patient were used for evaluation.
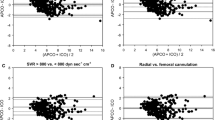
Statistical analysis
Data are presented as means ± standard deviation (SD). Data pairs were analysed using linear correlations and Pearson's correlation coefficient. Bias and limits of agreement of data pairs were determined as described by Bland and Altman. Bias represents the systemic error between two methods and was calculated as the mean difference between CCOPAC and CCOPCCO, and between CCOPAC and COTCP. Upper and lower limits of agreement, calculated as bias ± 1.96 SD, define the range in which 95% of the differences are expected to lie. The relative error was calculated as 100 × (CCOPAC-CCOPCCO)/[(CCOPAC+CCOPCCO)] and 100 × (CCOPAC-CCOTCP)/[(CCOPAC+CCOTCP)], as proposed by Rödig et al. [16].
Results
Patients
The mean age of patients was 59 ± 17 years (range 30–81 years), body weight was 86 ± 14 kg, height was 177 ± 8 cm, and body surface area was 2.00 ± 0.14 m2. Thirteen data sets per patient measured over a median time period of 15.5 h were used for statistical calculation, resulting in a total number of 182 data sets.
Cardiac output measurement
The mean CCOPAC was 8.8 ± 2.2 l min−1. The mean CCOPCCO and COTCP were 8.9 ± 2.5 and 9.0 ± 2.4 l min−1, respectively. The range of CCOPAC was 3.6–12.8 l min−1, the range of CCOPCCO was 3.5–14.8 l min−1 and the range of COTCP was 4.2–13.5 l min−1. Differences between the methods are reported in Table 1. The correlation between CCOPAC and CCOPCCO was highly significant (r 2 = 0.714, p < 0.0001), accompanied by a bias of 0.1 l min−1 and 95% limits of agreement between −2.5 l and 2.8 l min−1 (Fig. 1a). The correlation between CCOPAC and COTCP was also highly significant (correlation coefficient r 2 = 0.781, p < 0.0001). There was a bias for the two methods of 0.2 l min−1 and 95% limits of agreement ranging from −2.0 to 2.4 l min−1 (Fig. 1b). The median relative error of comparisons between CCOPAC and CCOPCCO was 1.5 and 2.5% for comparisons between CCOPAC and CCOTCP. It was within 15% for 72.5% of comparisons between CCOPAC and CCOPCCO, and for 75.1% of comparisons between CCOPAC and CCOTCP.
Comparison of preload variables
The mean CVP and mean PAOP were 13.9 ± 6.8 and 17.6 ± 5.5 mm Hg, respectively. The mean RVEDV was 289.4 ± 85.8 ml, and mean GEDV was 1787.3 ± 372.4 ml. There was no clinically relevant correlation between CVP and RVEDV (r 2 = 0.119, p < 0.0001; Fig. S.F1a), and no correlation between CVP and GEDV (r 2 = 0.001, p = 0.736; Fig. S.F2a). In addition, PAOP did not correlate with RVEDV or GEDV (r 2 = 0.015, p = 0.102 and r 2 = 0.013, p = 0.127 respectively; Figs. S.F1b, S.F2b). Measurement of RVEDV by pulmonary artery catheter did not correlate with GEDV measured by the PiCCO system (r 2 = 0.005, p = 0.336; Fig. S.F3).
Discussion
Our results show an excellent correlation, a small median relative error and a small mean difference (bias) of CCOPCCO as compared with CCOPAC for continuous cardiac output measurement in patients with septic shock. There was, however, a considerable variability of corresponding data pairs. No correlation was found between GEDV and the traditional preload markers CVP and PAOP, as well as between GEDV and REDV.
This is the first study that compares two methods for continuous monitoring of cardiac output in patients with septic shock. Both continuous and intermittent measurement of cardiac output by the PiCCO system showed a small systematic error (bias) compared with CCOPAC in patients with septic shock. Although the median relative error between CCOPAC and CCOPCCO and between CCOPAC and COTCP was small, the 95% limits of agreement between CCOPAC and CCOPCCO and between CCOPAC and COTCP in our patients appeared to be relatively high; however, similar variabilities in cardiac output using the two methods have been reported by numerous studies focusing on the perioperative period [17–20]. The variability of cardiac output data in our study may have been caused by haemodynamic changes and changing doses of catecholamines that may have occurred over hours. Since the CCOPAC displays the averaged cardiac output of the previous 3–6 min [5], acute haemodynamic changes may be apprehended less rapidly by this system. In addition, mechanical ventilation causing cyclic changes in temperature of pulmonary arterial blood and venous return may have influenced cardiac output measurement by pulmonary thermodilution [1, 4].
Several authors have shown a good agreement between CCOPAC and cardiac output assessed by intermittent measurement via a pulmonary artery catheter [21–23]. It has been suggested that CCOPAC may be accepted itself as a reference method for measuring cardiac output [22]; therefore, in order to limit the time needed to perform the measurements, and to avoid fluid overload in these septic patients, we chose CCOPAC as a reference method.
Our data show that in patients with septic shock, CVP or PAOP do not show a correlation with RVEDV or GEDV. The importance of CVP and PAOP as markers of ventricular preload has been questioned by several studies before [9–11]. Our patients represented a relatively heterogeneous population regarding age, concomitant cardiovascular diseases and cause for septic shock; therefore, the ventricular compliance may have varied significantly between patients and even in the same patient over time. In addition, cardiomyopathy may occur during sepsis [24], and therefore, hidden heart failure may have also contributed to the poor relationship between filling pressures and GEDV or RVEDV.
Since RVEDV and GEDV have been suggested to estimate ventricular preload more precisely, we hypothesized that a correlation be detectible between RVEDV and GEDV. Previous investigations on RVEDV as an index of cardiac preload have yielded conflicting results. While some studies in critically ill patients found changes in RVEDV to predict changes in cardiac output [12, 25], others did not find RVEDV to be a reliable predictor of the response to fluid challenge [26, 27]. Numerous studies have shown that GEDV was a more reliable indicator of cardiac preload than CVP and PAOP in patients undergoing cardiac surgery [28, 29] and critically ill patients [30]. The GEDV was shown to reflect echocardiographic changes in left ventricular preload [31] and has been suggested to be a useful indicator of cardiac preload in patients with septic shock [13, 32].
Since our data showed no correlation between RVEDV and GEDV, these variables appear to be not equally suitable to estimate cardiac preload in patients with septic shock. Further studies are required to show which measurement is most appropriate for estimation of cardiac preload in patients with septic shock.
Conclusion
We found an excellent correlation and a small bias of CCOPCCO as compared with CCOPAC for continuous cardiac output measurement in patients with septic shock. The precision of single CCOPCCO measurements compared with CCOPAC, however, appeared to be limited. No correlation was found between RVEDV and GEDV, suggesting that they are not equally suitable for estimation of cardiac preload in patients with septic shock.
References
Nishikawa T, Dohi S (1993) Errors in the measurement of cardiac output by thermodilution. Can J Anaesth 40:142–153
Mermel LA, Maki DG (1994) Infectious complications of Swan-Ganz pulmonary artery catheters. Pathogenesis, epidemiology, prevention, and management. Am J Respir Crit Care Med 149:1020–1036
Boldt J, Menges T, Wollbruck M, Hammermann H, Hempelmann G (1994) Is continuous cardiac output measurement using thermodilution reliable in the critically ill patient? Crit Care Med 22:1913–1918
Böttiger BW, Soder M, Rauch H, Böhrer H, Motsch J, Bauer H, Martin E (1996) Semi-continuous versus injectate cardiac output measurement in intensive care patients after cardiac surgery. Intensive Care Med 22:312–318
Yelderman M (1990) Continuous measurement of cardiac output with the use of stochastic system identification techniques. J Clin Monit 6:322–332
Vincent JL, Reuse C, Frank N, Contempre B, Kahn RJ (1989) Right ventricular dysfunction in septic shock: assessment by measurements of right ventricular ejection fraction using the thermodilution technique. Acta Anaesthesiol Scand 33:34–38
Bossert T, Gummert JF, Bittner HB, Barten M, Walther T, Falk V, Mohr FW (2006) Swan-Ganz catheter-induced severe complications in cardiac surgery: right ventricular perforation, knotting, and rupture of a pulmonary artery. J Cardiac Surg 21:292–295
Gödje O, Höke K, Goetz AE, Felbinger TW, Reuter DA, Reichart B, Friedl R, Hannekum A, Pfeiffer UJ (2002) Reliability of a new algorithm for continuous cardiac output determination by pulse-contour analysis during hemodynamic instability. Crit Care Med 30:52–58
Lichtwarck-Aschoff M, Beale R, Pfeiffer UJ (1996) Central venous pressure, pulmonary artery occlusion pressure, intrathoracic blood volume, and right ventricular end-diastolic volume as indicators of cardiac preload. J Crit Care 11:180–188
Hansen RM, Viquerat CE, Matthay MA, Wiener-Kronish JP, DeMarco T, Bahtia S, Marks JD, Botvinick EH, Chatterjee K (1986) Poor correlation between pulmonary arterial wedge pressure and left ventricular end-diastolic volume after coronary artery bypass graft surgery. Anesthesiology 64:764–770
Kumar A, Anel R, Bunnell E, Habet K, Zanotti S, Marshall S, Neumann A, Ali A, Cheang M, Kavinsky C, Parrillo JE (2004) Pulmonary artery occlusion pressure and central venous pressure fail to predict ventricular filling volume, cardiac performance, or the response to volume infusion in normal subjects. Crit Care Med 32:691–699
Reuse C, Vincent JL, Pinsky MR (1990) Measurements of right ventricular volumes during fluid challenge. Chest 98:1450–1454
Michard F, Alaya S, Zarka V, Bahloul M, Richard C, Teboul JL (2003) Global end-diastolic volume as an indicator of cardiac preload in patients with septic shock. Chest 124:1900–1908
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Wesseling K, de Wit B, Ty Smith N (1983) A simple device for the continuous measurement of cardiac output. Adv Cardiovasc Phys 5:16–52
Rödig G, Prasser C, Keyl C, Liebold A, Hobbhahn J (1999) Continuous cardiac output measurement: pulse contour analysis vs thermodilution technique in cardiac surgical patients. Br J Anaesth 82:525–530
Della Rocca G, Costa MG, Pompei L, Coccia C, Pietropaoli P (2002) Continuous and intermittent cardiac output measurement: pulmonary artery catheter versus aortic transpulmonary technique. Br J Anaesth 88:350–356
Della Rocca G, Costa MG, Coccia C, Pompei L, Marco P di, Vilardi V, Pietropaoli P (2003) Cardiac output monitoring: aortic transpulmonary thermodilution and pulse contour analysis agree with standard thermodilution methods in patients undergoing lung transplantation. Can J Anaesth 50:707–711
Jakobsen CJ, Melsen NC, Andresen EB (1995) Continuous cardiac output measurements in the perioperative period. Acta Anaesthesiol Scand 39:485–488
Zink W, Nöll J, Rauch H, Bauer H, Desimone R, Martin E, Böttiger BW (2004) Continuous assessment of right ventricular ejection fraction: new pulmonary artery catheter versus transoesophageal echocardiography. Anaesthesia 59:1126–1132
Lichtenthal PR, Gordan D (1996) Testing the safety of Baxter continuous cardiac output monitoring system. J Clin Monit 12:243–249
Mielck F, Buhre W, Hanekop G, Tirilomis T, Hilgers R, Sonntag H (2003) Comparison of continuous cardiac output measurements in patients after cardiac surgery. J Cardiothorac Vasc Anesth 17:211–216
Schmid ER, Schmidlin D, Tornic M, Seifert B (1999) Continuous thermodilution cardiac output: clinical validation against a reference technique of known accuracy. Intensive Care Med 25:166–172
Parrillo JE (1989) The cardiovascular pathophysiology of sepsis. Annu Rev Med 40:469–485
Diebel LN, Wilson RF, Tagett MG, Kline RA (1992) End-diastolic volume. A better indicator of preload in the critically ill. Arch Surg 127:817–822
Wagner JG, Leatherman JW (1998) Right ventricular end-diastolic volume as a predictor of the hemodynamic response to a fluid challenge. Chest 113:1048–1054
Wiesenack C, Fiegl C, Keyser A, Laule S, Prasser C, Keyl C (2005) Continuously assessed right ventricular end-diastolic volume as a marker of cardiac preload and fluid responsiveness in mechanically ventilated cardiac surgical patients. Crit Care 9:R226–R233
Gödje O, Hoke K, Lamm P, Schmitz C, Thiel C, Weinert M, Reichart B (1998) Continuous, less invasive, hemodynamic monitoring in intensive care after cardiac surgery. Thorac Cardiovasc Surg 46:242–249
Wiesenack C, Prasser C, Keyl C, Rodig G (2001) Assessment of intrathoracic blood volume as an indicator of cardiac preload: single transpulmonary thermodilution technique versus assessment of pressure preload parameters derived from a pulmonary artery catheter. J Cardiothorac Vasc Anesth 15:584–588
Bindels AJ, van der Hoeven JG, Graafland AD, de Koning J, Meinders AE (2000) Relationships between volume and pressure measurements and stroke volume in critically ill patients. Crit Care 4:193–199
Hofer CK, Furrer L, Matter-Ensner S, Maloigne M, Klaghofer R, Genoni M, Zollinger A (2005) Volumetric preload measurement by thermodilution: a comparison with transoesophageal echocardiography. Br J Anaesth 94:748–755
Sakka SG, Bredle DL, Reinhart K, Meier-Hellmann A (1999) Comparison between intrathoracic blood volume and cardiac filling pressures in the early phase of hemodynamic instability of patients with sepsis or septic shock. J Crit Care 14:78–83
Acknowledgements
This study was supported, in part, by a grant from Edwards Lifesciences, Germany, to B.W.B., which might represent a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Spöhr, F., Hettrich, P., Bauer, H. et al. Comparison of two methods for enhanced continuous circulatory monitoring in patients with septic shock. Intensive Care Med 33, 1805–1810 (2007). https://doi.org/10.1007/s00134-007-0703-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0703-2