Abstract
Purpose
Several reports in the literature have described the effects of positive end-expiratory pressure (PEEP) level upon functional residual capacity (FRC) in ventilated patients during general anesthesia. This study compares FRC in mechanically low tidal volume ventilation with different PEEP levels during upper abdominal surgery.
Methods
Before induction of anesthesia (awake) for nine patients with upper abdominal surgery, a tight-seal facemask was applied with 2 cmH2O pressure support ventilation and 100 % O2 during FRC measurements conducted on patients in a supine position. After tracheal intubation, lungs were ventilated with bilevel airway pressure with a volume guarantee (7 ml/kg predicted body weight) and with an inspired oxygen fraction (FIO2) of 0.4. PEEP levels of 0, 5, and 10 cmH2O were used. Each level of 5 and 10 cmH2O PEEP was maintained for 2 h. FRC was measured at each PEEP level.
Results
FRC awake was significantly higher than that at PEEP 0 cmH2O (P < 0.01). FRC at PEEP 0 cmH2O was significantly lower than that at 10 cmH2O (P < 0.01). PaO2/FIO2 awake was significantly higher than that for PEEP 0 cmH2O (P < 0.01). PaO2/FIO2 at PEEP 0 cmH2O was significantly lower than that for PEEP 5 cmH2O or PEEP 10 cmH2O (P < 0.01). Furthermore, PEEP 0 cmH2O, PEEP 5 cmH2O after 2 h, and PEEP 10 cmH2O after 2 h were correlated with FRC (R = 0.671, P < 0.01) and PaO2/FIO2 (R = 0.642, P < 0.01).
Conclusions
Results suggest that PEEP at 10 cmH2O is necessary to maintain lung function if low tidal volume ventilation is used during upper abdominal surgery.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Pulmonary gas exchange and respiratory mechanics are usually impaired during general anesthesia and muscle paralysis. Functional residual capacity (FRC) decreases approximately 20 % during induction of anesthesia [1]. Intraabdominal surgery might aggravate FRC loss. Reduced FRC can be restored somewhat through ventilation using positive end-expiratory pressure (PEEP). Nevertheless, few reports in the literature describe studies of the influence of PEEP level upon FRC in ventilated patients during administration of general anesthesia. FRC was reduced by induction of anesthesia, but no report in the literature has described a comparison of FRC values with those of stepwise increase of PEEP during upper abdominal surgery. We measured FRC for mechanically ventilated general anesthesia with different PEEP levels during upper abdominal surgery and subsequently compared them with awake levels measured for the subject in the supine position. We hypothesized that FRC, compliance, and arterial oxygenation show positive effects of increased PEEP, and that 5 cmH2O PEEP or 10 cmH2O PEEP increased FRC nearly to the awake level. Different techniques have been developed and evaluated recently for FRC measurements during mechanical ventilation. The wash-in or wash-out of a tracer gas in a multiple breath maneuver is apparently best applied at bedside. Promising techniques for nitrogen or oxygen wash-in/wash-out with reasonable accuracy and repeatability have been presented [2]. This technique, which estimates FRC with good precision using a change of FIO2 of only 0.1, has been evaluated in volunteers and in patients with acute respiratory distress syndrome [3].
Materials and methods
We studied nine patients with American Society of Anesthesiologists Physical Status Classification System grade 1 or grade 2 who had been scheduled for elective upper abdominal surgery. Informed consent was obtained from each patient. The study was approved by the Tohoku University Hospital Ethics Committee. No patient had cardiac or pulmonary disease. The arterial line, inserted under local anesthesia, was used for the study protocol. Monitoring included invasive arterial blood pressure, a continuous electrocardiogram, and peripheral oxygen saturation (SpO2). After induction of anesthesia and tracheal intubation, end-tidal carbon dioxide concentration (ETCO2), airway pressure, tidal volume, and respiratory rate were monitored and recorded.
Anesthesia
No premedication was administered. Before induction of anesthesia (Awake), a tight-seal facemask was used for spontaneous ventilation (Engström Carestation; GE Healthcare, Madison, WI, USA). The facemask was applied with 2 cmH2O pressure support ventilation using an inspired oxygen fraction (FIO2) of 1.0 during FRC measurement (FRC INview). The FRC was designated as the facemask FRC value minus facemask dead space (100 ml). Arterial blood gas samples were collected from subjects who were in a supine position (Fig. 1). Patients were ventilated with 2 cmH2O pressure support ventilation at awake time. Anesthesia was induced as target-controlled infusion of propofol 4–5 μg/ml with a calculated target plasma, fentanyl 1–2 μg/kg i.v., and rocuronium bromide 0.6 mg/kg i.v.
Predicted body weight was calculated as 45.4 + 0.91 × [height (cm) − 152.4] for women or 49.9 + 0.91 × [height (cm) − 152.4] for men. After tracheal intubation, anesthesia was maintained with a propofol target plasma drug concentration of 2.5–3 μg/ml and remifentanil 0.2–0.4 μg/kg/min with thoracic epidural analgesia. A neuromuscular block was monitored continuously using a nerve stimulator. Rocuronium bromide was infused as necessary.
Lungs were ventilated in bilevel airway pressure with volume guarantee (pressure-regulated volume control). Upper airway pressure was maintained for 1.3 s and with FIO2 0.4. Ventilation was started. The tidal volume of 7 ml/kg was estimated according to the predicted body weight. The respiratory rate was adjusted to maintain ETCO2 at 35–40 mmHg. FRC measurements and arterial blood gas samples were taken from 30 min after intubation (pre-ope). From 1 h after intubation, FRC measurements and arterial blood gas samples were obtained during upper abdominal surgery (opeP0). The abdominal cavity was opened for opeP0.
Subsequent ventilations started with PEEP 5 cmH2O. After 1 and 2 h PEEP 5 cmH2O, FRC measurements and arterial blood gas samples were collected (opeP5.1 and opeP5.2). FRC measurements and arterial blood gas samples were also collected at 1 and 2 h after the stepwise increase of PEEP 10 cmH2O (opeP10.1 and opeP10.2).
The quasistatic compliance of the respiratory system was calculated as the tidal volume divided by the inspiratory plateau pressure minus the end-expiratory pressure. Values are expressed as mean ± SD. Comparison among groups was performed using two-way analysis of variance for repeated one-way measurements. Correlation between PEEP and FRC or the PaO2/FIO2 ratio was analyzed using Pearson’s correlation. For all comparisons, P < 0.05 was considered significant.
Results
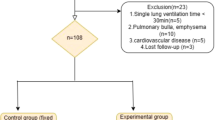
Figure 1 presents patient data of the nine patients studied.
Figure 2 shows data obtained for FRC. The value of FRC awake was significantly higher than that for pre-ope or opeP0 (P < 0.01). The FRC ope10.1 and ope10.2 values were significantly higher than that for opeP5.1 (P < 0.01). The FRC for opeP10.2 was significantly higher than that for ope5.2 (P < 0.01).
Figure 3 presents oxygenation data. The PaO2/FIO2 awake was significantly higher than that for pre-ope, opeP0, or ope5.1 (P < 0.01). PEEP 5 cmH2O and PEEP 10 cmH2O were significantly higher than either pre-ope or opeP0 (P < 0.01) (Table 1).
Correlation
PEEP levels at opeP0, opeP5.2, and opeP10.2 were correlated with FRC (R = 0.671, P < 0.01) and PaO2/FIO2 (R = 0.642, P < 0.01) (Fig. 4).
Quasistatic compliance (Table 2)
Compliance was significantly higher for opeP10.2 than for opeP5.1 (P < 0.01).
Hemodynamics (Table 2)
Maximum arterial pressure and heart rate were lowest at pre-ope. No significant difference was found in hemodynamics among different PEEP groups.
Discussion
The first main finding of our study was that PEEP showed positive effects on FRC, compliance, and PaO2/FIO2 ratio, indicating that patients undergoing upper abdominal surgery might benefit from PEEP 10 cmH2O.
The FRC examinations were performed using an Engström Carestation (GE Healthcare) equipped with the FRC Inview monitoring feature. The FRC is determined using the change of lung nitrogen volume after a step change in the inspired oxygen fraction. In the Engström Carestation, when ventilated with FIO2 1.0, where the O2 consumption was calculated from the CO2 production with a default RQ of 0.85, very high measurement precision was attained [2].
Results show that FRC was reduced by 37 % from the awake level after the induction of anesthesia. As previously reported, FRC is reduced by approximately 15 % during anesthesia induced with thiopentone and maintained with halothane at FIO2 0.35 [4]. Our protocol was FIO2 1.0 at induction of anesthesia, which engendered absorption atelectasis because of the high concentration of oxygen. The mechanisms underlying reduction of FRC include muscle paralysis, decreased chest wall recoil, increased abdominal pressure, atelectasis formation, and gas entrapment behind a closed airway [5]. Our results showed no significant change in FRC between that after induction of anesthesia and that during operation at zero end-expiratory pressure (ZEEP). During abdominal operation, FRC increased transiently when the cavity was opened [6]. However, during the surgery procedure, FRC decreased and returned to post-induction levels at the end of the procedure. Indeed, pulmonary gas exchange, which is impaired following induction of anesthesia, deteriorates during laparotomy but not during peripheral surgery. The difference is probably explained by the effect of surgical influences (packs, retractors, etc.) on FRC [1]. At opeP0, surgical influences (retractors) were started.
Results of this study demonstrated that PEEP 10 cmH2O reached nearly the same FRC level as that of awake FRC. No data exist to elucidate waking FRC for different PEEP levels, showing intraoperative FRC changes. Neumann et al. [7] presented measured mean FRC data for postoperative patients at different PEEP levels (0, 5, 10 cmH2O). Their study revealed that PEEP increased FRC at levels of PEEP 5 and 10 cmH2O; PEEP decreased FRC after reversion to PEEP of 0 cmH2O. Pelosi et al. [8] reported that PEEP 10 cmH2O did not improve respiratory function in paralyzed or anesthetized postoperative patients. Their mean PaO2/FIO2 ratio was 436 mmHg, and their tidal volume was 8–12 ml/kg ideal body weight. Our mean PaO2/FIO2 ratio was 253 mmHg, and tidal volume was 7 ml/kg ideal body weight at PEEP 0 cmH2O intraoperatively. Lower tidal volume might engender atelectasis, especially if PEEP is low or not used at all. Sufficient PEEP must be used to minimize atelectasis and to maintain oxygenation [9].
Determann et al. described a randomized controlled nonblinded preventive trial comparing mechanical ventilation with tidal volume of 10 versus 6 ml/kg in critically ill patients without acute lung injury (ALI) at the onset of mechanical ventilation. Mechanical presentation with 10 ml/kg is associated with sustained cytokine production in plasma [10]. Those results suggest that mechanical ventilation with conventional tidal volumes contributed to the development of lung injury in patients without ALI at the onset of mechanical ventilation. This theory applies to mechanical ventilation during surgery.
Administration of PEEP alone increased the normally aerated lung fraction, which combined with a reduction of poorly aerated lung tissue while atelectasis remained unchanged [10]. An earlier study of postoperative mechanically ventilated obese patients (mean body mass index, 51) after abdominal surgery showed that PEEP 10 cmH2O increased PaO2, respiratory compliance, and FRC [8]. PEEP at 10 cmH2O was sufficient to maintain substantial improvement of respiratory function. Reportedly, PEEP higher than 10 cmH2O is associated with marked derangement of hemodynamics [11]. Rothen et al. [12] reported that static compliance and the amount of atelectasis estimated using computed tomography (CT) did not change in parallel. Maisch et al. [13] described that compliance indicates an optimal level of PEEP after recruitment in anesthetized patients, reporting that optimal PEEP was 10 cmH2O because, at that pressure level, the highest compliance value in conjunction with the lowest dead space fraction revealed a maximum amount of effectively expanded alveoli. Our results demonstrated that the quasistatic compliance was significantly higher for opeP 10.2 than for opeP 5.1. PEEP 10 cmH2O did not produce the pre-operation level of PaO2/FIO2, probably because of a ventilation and circulation mismatch by mechanical ventilation or because recruitment maneuvers were not used. The increased intrapleural pressure caused by PEEP might also increase the risk of barotrauma and cause changes to cardiovascular dynamics. Two trials reported postoperative barotrauma in both PEEP and ZEEP [14, 15]. The event rate was zero in both groups in both trials. The Imberger G group calculated an effect estimate of cardiac complication. Their comparison revealed RR of 0.3 for the PEEP group, which was not statistically significant [16]. It remains unclear whether the increases in FRC and P/F ratio are attributable to the increase in PEEP level, or to a time-dependent effect of PEEP, or both. During a time study of 5 h operation, PaO2 showed constant values at much lower tidal volumes of 6 ml/kg and PEEP 10 cmH2O (21 patients were enrolled; 13 cases were upper abdominal surgeries with abdominal opening) [17]. Following coronary artery bypass grafting, significant reduction of P (A–a) O2 during positive pressure ventilation at 10 cmH2O PEEP was compared with 0 cmH2O PEEP and 5 cmH2O PEEP during 6 h [18]. These data show that pulmonary oxygenation might maintain constant values at equal PEEP levels.
As one limitation of our study, PEEP was applied in a stepwise increasing fashion. We have no data for P/F ratio and FRC on time-dependent effect of PEEP. However, the same PEEP level was maintained for 2 h. Two hours after changing PEEP, the FRC data were slightly higher than at 1 h after changing PEEP, but the values were not significantly different. The PEEP levels at opeP0, opeP5.2, and opeP10.2 were correlated with FRC and with PaO2/FIO2. Consequently, the PEEP increase was inferred to have engendered the FRC increase. The PEEP levels might be applied in a random sequence to mitigate this potential bias in the results.
Conclusions
Data reported herein suggest that if low tidal volume ventilation is used during upper abdominal surgery, then PEEP 10 cmH2O is necessary to maintain lung function.
References
Wahba RW. Perioperative functional residual capacity. Can J Anaesth. 1991;38:384–400.
Olegård C, Söndergaard S, Houltz E, Lundin S, Stenqvist O. Estimation of functional residual capacity at the bedside using standard monitoring equipment: a modified nitrogen wash-out/wash-in technique requiring a small change of the inspired oxygen fraction. Anesth Analg. 2005;101:206–12.
Choncholas G, Sondergaard S, Heinonen E. Validation and clinical application of a first order step response equation for nitrogen clearance during FRC measurement. J Clin Monit Comput. 2008;22:1–9.
Hewlett AM, Hulands GH, Nunn JF, Milledge JS. Functional residual capacity during anaesthesia III: artificial ventilation. Br J Anaesth. 1974;46:495–503.
Wahba RM. Airway closure and intraoperative hypoxaemia: twenty-five years later. Can J Anaesth. 1996;43:1144–9.
Damia G, Mascheroni D, Croci M, Tarenzi L. Perioperative changes in functional residual capacity in obese patients. Br J Anaesth. 1988;60:574–8.
Neumann P, Zinserling J, Haase C, Sydow M, Burchardi H. Evaluation of respiratory inductive plethysmography in controlled ventilation. Chest. 1998;113:443–51.
Pelosi P, Ravagnan I, Giurati G, Panigada M, Bottino N, Tredici S, Eccher G, Gattinoni L. Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology. 1999;91:1221–31.
Schultz MJ, Haitsma JJ, Slutsky AS, Gajic O. What tidal volumes should be used in patients without acute lung injury? Anesthesiology. 2007;106:1226–31.
Determann RM, Royakkers A, Wolthuis EK, Vlaar AP, Choi G, Paulus F, Hofstra JJ, de Graaff MJ, Korevaar JC, Schultz MJ. Ventilation with lower tidal volumes as compared to conventional tidal volumes for patients without acute lung injury—a preventive randomized controlled trial. Crit Care. 2010;14:R1.
Reinius H, Jonsson L, Gustafsson S, Sundbom M, Duvernoy O, Pelosi P, Hedenstierna G, Freden F. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology. 2009;111:979–87.
Rothen HU, Sporre B, Engberg G, Wegenius G, Hogman M, Hedenstierna G. Influence of gas composition on recurrence of atelectasis after a reexpansion maneuver during general anesthesia. Anesthesiology. 1995;82:832–42.
Maisch S, Reissmann H, Fuellekrug B, Weismann D, Rutkowski T, Tusman G, Bohm SH. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg. 2008;106:175–81.
Almarakbi WA, Fawzi HM, Alhashemi JA. Effects of four intraoperative ventilatory strategies on respiratory compliance and gas exchange during laparoscopic gastric banding in obese patients. Br J Anaesth. 2009;102:862–8.
Talab HF, Zabani IA, Abdelrahman HS, Bukhari WL, Mamoun I, Ashour MA, Sadeq BB, El Sayed SI. Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg. 2009;109:1511–6.
Imberger G, McIlroy D, Pace NL, Wetterslev J, Brok J, Møller AM. Positive end-expiratory pressure (PEEP) during anaesthesia for the prevention of mortality and postoperative pulmonary complications. Cochrane Database Syst Rev 2010;8:CD007922.
Wolthuis EK, Choi G, Dressing MC, Bresser P, Lutter R, Dzolijic M, Poll T, Vroom MB, Hollmann M, Schultz MJ. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology. 2008;108:46–54.
Marvel SL, Elliott CG, Tocino I, Greenway LW, Metcalf SM, Chapman RH. Positive end-expiratory pressure following coronary artery bypass grafting. Chest. 1986;90:537–41.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Satoh, D., Kurosawa, S., Kirino, W. et al. Impact of changes of positive end-expiratory pressure on functional residual capacity at low tidal volume ventilation during general anesthesia. J Anesth 26, 664–669 (2012). https://doi.org/10.1007/s00540-012-1411-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-012-1411-9