Abstract
Background
Pancreatic ductal occlusion can accompany pancreatic head cancer, leading to pancreatic exocrine insufficiency (PEI) and adverse effects on nutritional status and postoperative outcomes. We investigated its impact on nutritional status, body composition, and postoperative outcomes in patients with pancreatic head cancer undergoing neoadjuvant therapy (NAT).
Methods
We analyzed 136 patients with pancreatic head cancer who underwent NAT prior to intended pancreaticoduodenectomy (PD) between 2015 and 2022. Nutritional and anthropometric indices (body mass index [BMI], albumin, prognostic nutritional index [PNI], Glasgow prognostic score, psoas muscle index, subcutaneous adipose tissue index [SATI], and visceral adipose tissue index) and postoperative outcomes were compared between the occlusion (n = 78) and non-occlusion (n = 58) groups, in which 61 and 44 patients, respectively, ultimately underwent PD.
Results
The occlusion group showed significantly lower post-NAT BMI, PNI, and SATI (p = 0.011, 0.005, and 0.015, respectively) in the PD cohort. The occlusion group showed significantly larger main pancreatic duct, smaller pancreatic parenchyma, and greater duct–parenchymal ratio (p < 0.001), and these morphological parameters significantly correlating with post-NAT nutritional and anthropometric indices. Postoperative 3-year survival and recurrence-free survival (RFS) rates were significantly poorer (p = 0.004 and 0.013) with pancreatic ductal occlusion, also identified as an independent postoperative risk factor for overall survival (hazard ratio [HR]: 2.31, 95% confidence interval [CI] 1.08–4.94, p = 0.030) and RFS (HR: 2.03, 95% CI 1.10–3.72, p = 0.023), in multivariate analysis.
Conclusions
Pancreatic ductal occlusion may be linked to poorer postoperative outcomes due to PEI-related malnutrition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer has an extremely poor prognosis, with the worst 5-year survival rate (12%) among cancers covered by United States statistics [1]. Pancreatectomy remains the only curative option; however, it is highly invasive, entails risks of postoperative pancreatic fistula (POPF) [2], delayed gastric emptying (DGE) [3], and post-pancreatectomy hemorrhage (PPH) [4], and is associated with a high (79%) early postoperative recurrence rate [5]. Postoperative outcomes could be improved by identifying novel prognostic indicators to inform clinical decision making.
Tumor size and differentiation, lymph node metastasis, and resection margin are known prognosticators of pancreatic cancer [6, 7]; however, the relevant data cannot be obtained preoperatively. Consequently, preoperative clinical assessment items have been investigated as potential prognosticators, including prognostic nutritional index (PNI) [8], Glasgow prognostic score (GPS) [9], psoas muscle index (PMI) [10], and subcutaneous adipose tissue (SAT), and visceral adipose tissue (VAT) [11].
Neoadjuvant treatment (NAT) has recently become the mainstream treatment for pancreatic cancer and is reportedly associated with prolonged survival [12,13,14]. However, NAT tends to extend the waiting period prior to surgery, and is reportedly associated with impaired nutritional status [15, 16] and body composition [17,18,19]. Furthermore, NAT-associated impaired body composition is a potential negative prognosticator in patients with pancreatic cancer [19]. Malnutrition should thus be assessed during NAT, using blood biochemical and imaging examinations.
Pancreatic head cancer can have a poorer prognosis when the tumor causes ductal occlusion resulting in exocrine insufficiency (PEI)-related malnutrition [20, 21]; however, the impact of pancreatic ductal occlusion has not previously been characterized in patients with this cancer.
Accordingly, in this study, we aimed to investigate the effects of pancreatic ductal occlusion on nutritional status, body composition, and postoperative outcomes in patients with pancreatic head cancer who underwent NAT prior to intended pancreaticoduodenectomy (PD).
Methods
This retrospective observational study was conducted in compliance with the Declaration of Helsinki, and was approved by the Institutional Review Bord of Kagoshima University Hospital. The requirement for obtaining informed consent was waived owing to the retrospective nature of the study; however, the content of the study was publicly disclosed on the Kagoshima University Hospital homepage, enabling the participants or their designated representatives to opt out of participation.
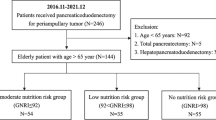
Patients
We identified 173 consecutive patients diagnosed with pancreatic head cancer who underwent NAT prior to intended PD at Kagoshima University Hospital, between January 1, 2015 and December 31, 2022. The analysis set comprised 136 patients after excluding cases corresponding to absence of pre-NAT computed tomography (CT) images (n = 5), preoperative ductal stent placement (n = 5), pancreatic enzyme replacement therapy (PERT) (n = 24), or variance in clinical course (n = 3). All clinical data were obtained from the electronic medical records of Kagoshima University Hospital and its affiliated institutions.
Evaluation and definition of pancreatic ductal occlusion
Pancreatic ducts were evaluated for occlusion (Fig. 1A, B) or non-occlusion (Fig. 1C, D) by a radiologist (TA, KT) and the principal investigator (YH) using pre-NAT CT images. Magnetic resonance cholangiopancreatography images were referenced when available.
Representative images of cases with and without pancreatic ductal occlusion. A and B CT (A) and MRCP images (B) of a 69-year-old man with pancreatic ductal occlusion showing pancreatic cancer (arrows) and a dilated main pancreatic duct (arrowhead). C and D, CT (C) and MRCP images (D) of a 73-year-old man without pancreatic ductal occlusion showing pancreatic cancer (arrows) and an undilated main pancreatic duct (arrowhead). CT computed tomography, MRCP magnetic resonance cholangiopancreatography
Pancreatic ductal occlusion was defined as tumor obstruction of both the main and accessory ducts and a dilated upstream main pancreatic duct (MPD) ≥ 3 mm, which was set as the cutoff referring to a previous report [22]. The MPD was measured on cross-sectional CT images of the presumed transection line of the pancreas near the portal vein.
Neoadjuvant treatment and adjuvant chemotherapy
The NAT regimens in this study were as follows: (i) gemcitabine plus tegafur/gimeracil/oteracil (S-1) therapy (GS therapy) (n = 43) [23]; (ii) nab-paclitaxel plus gemcitabine therapy (GN therapy) (n = 50) [24]; (iii) chemoradiotherapy (CRT) with or without additional GS or GN therapy (CRT) (n = 35); and (iv) other treatments (n = 8). CRT included external-beam radiation with concurrent S-1 administration. Other regimens included a modified combination therapy of folinic acid, fluorouracil, irinotecan, and oxaliplatin (mFOLFIRINOX) (n = 1) [25]; any two chemotherapy regimens from S-1 monotherapy, GS, GN, and mFOLFIRINOX therapy (n = 4); S-1 plus proton therapy (n = 2); and radiation-alone therapy (n = 1). The content, intensity, and cycles of NAT were established in accordance with standard protocols, but were adjusted when necessary, by the attending physician based on the patient's condition and treatment efficacy.
In this study, adjuvant chemotherapy involved a 6-month regimen of S-1 monotherapy as the standard protocol [26]. Patients who experienced adverse reactions to S-1 then received gemcitabine monotherapy (n = 6) [26] or GN therapy (n = 1). Twenty patients did not receive adjuvant chemotherapy.
Clinicopathological data
The following data were collected: age, sex, resectability (based on the National Comprehensive Cancer Network guidelines version 2. 2021), NAT regimen, completion of NAT and PD, and the interval (days) from the initiation of NAT to surgery. In addition, we collected data on complications and determined from a history of treatment or preoperative blood biochemical examination findings (diabetes: hemoglobin A1c ≥ 6.5%; chronic kidney disease: estimated glomerular filtration rate < 60 mL/min/1.73 m2), pre- and post-NAT carbohydrate antigen 19–9 (CA 19–9) levels, the provision of preoperative biliary drainage, hematologic adverse events after NAT (≥ grade 3 based on Common Terminology Criteria for Adverse Event version 5.0), NAT treatment effect (based on Response Evaluation Criteria in Solid Tumors version 1.1), tumor-node-metastasis stage (based on the Union for International Cancer Control 8th edition), pathological tumor size, histological type and grade, Evans’ criteria [27], resection margin, operation time, operative blood loss, postoperative hospital stay, postoperative complications (Clavien–Dindo classification ≥ grade IIIa; POPF ≥ grade B [2]; DGE ≥ grade B [3]; and PPH ≥ grade B [4]), and provision of adjuvant chemotherapy and postoperative PERT.
Nutritional assessment
Body mass index (BMI) was obtained at pre- and post-NAT assessments. Albumin concentration (g/dL), lymphocyte count (/mm3), and C-reactive protein (CRP) (mg/dL) were obtained at pre- and post-NAT blood biochemical assessments. Pre-NAT BMI and blood biochemical data were obtained 18.0 days (interquartile range [IQR] 2.0–26.0 days) and 24.0 days (IQR 17.0–33.0 days) before NAT initiation, respectively. Post-NAT BMI and blood biochemical data were obtained 2.0 days (IQR 1.0–3.0 days) and 18.0 days (IQR 13.0–27.0 days) before PD, respectively.
Onodera’s PNI (10 × albumin g/dL + 0.005 × lymphocyte /mm3) [8] and GPS (GPS score = 2: both CRP > 1.0 mg/dL and albumin < 3.5 g/dL; GPS score = 1: CRP > 1.0 mg/dL or albumin < 3.5 g/dL; GPS score = 0: neither CRP > 1.0 mg/dL nor albumin < 3.5 g/dL) [9] were evaluated as described previously, using pre- and post-NAT blood biochemical data.
Image analysis
Pre-NAT CT images were obtained 32.0 days (IQR 21.0–42.0 days) before NAT initiation, and post-NAT CT images were obtained 24.0 days (IQR 14.0–41.0 days) before PD. Pancreatic morphology was evaluated using pre-NAT cross-sectional CT images. The MPD (mm) and pancreas (mm) were measured on the presumed transection line of the pancreas near the portal vein. Pancreatic parenchyma (mm) was calculated as follows:
Pancreatic parenchyma (mm) = size of the pancreas (mm) – size of the MPD (mm).
In addition, the ratio of the MPD to parenchymal thickness was calculated as follows [28]:
Duct–parenchymal ratio = size of the MPD (mm)/size of the pancreas (mm).
To evaluate muscle mass, L3-level cross-sectional CT images obtained pre- and post-NAT were used. The cross-sectional area of the bilateral psoas muscles (cm2) was measured by manual tracing, and the PMI was calculated as follows [10]:
PMI = Area of bilateral psoas muscle/height2 (cm2/m2).
To evaluate adipose tissue content, Dicom images corresponding to the L3-level cross-sectional CT images obtained pre- and post-NAT were analyzed automatically using SYNAPSE VINCENT software (Fujifilm Medical Co., Ltd., Tokyo, Japan). Tissue HU thresholds were set as follows: −190 to −30 HU for SAT and −150 to −50 HU for VAT [29]. SAT (cm2) and VAT (cm2) were divided by the square of the height to calculate the SAT index (SATI) and VAT index (VATI), respectively, as follows:
SATI = SAT/height2 (cm2/m2).
VATI = VAT/height2 (cm2/m2).
Statistical analyses
Data are presented as percentage or median and IQR values. Differences between groups were evaluated using the χ2 test, Fisher’s exact test, or Mann–Whitney U test. A two-sided p < 0.05 was regarded as statistically significant. Relationships between pancreatic morphology and nutritional and anthropometric indices were analyzed with Spearman’s rank correlation coefficient (rs). The Kaplan–Meier method was used to evaluate the 3-year survival and recurrence-free survival (RFS) rates after PD, and comparisons between groups were performed using the log-rank test. Univariate and multivariate analyses were performed using the Cox proportional-hazard model to identify potential prognostic factors influencing overall survival (OS) and RFS after PD. In the multivariate model, age, sex, and pancreatic ductal occlusion were selected as the clinically relevant variables, while resectability, pathological TNM stage and tumor size were selected as risk adjusting variables clinically influencing the survival analysis of this study. Stata version 18 (Stata Corp LLC, College Station, TX, USA) was used for all analyses.
Results
Clinicopathological characteristics
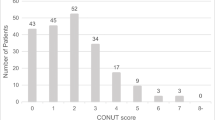
A total of 136 patients were assigned to the occlusion (n = 78) or non-occlusion (n = 58) group, and 105 of these patients ultimately underwent PD (occlusion group: n = 61; non-occlusion group: n = 44) (Table 1). For these 105 patients (PD cohort) showed, the histological tumor classifications were as follows: adenocarcinoma (n = 58), adenosquamous carcinoma (n = 1), and residual carcinoma (n = 2) in the occlusion group; and adenocarcinoma (n = 42), adenosquamous carcinoma (n = 1), and high-grade pancreatic intraepithelial neoplasia (n = 1) in the non-occlusion group.
The occlusion group showed significantly larger MPD, smaller pancreatic parenchyma, and greater duct–parenchymal ratio (p < 0.001). Patients in the occlusion group also experienced fewer postoperative complications, with significantly lower incidences of Clavien–Dindo classification ≥ grade IIIa complications (p = 0.038) and POPF (p < 0.001).
Nutritional and anthropometric indices at the pre- and post-NAT assessments
At pre-NAT, ductal occlusion was associated with significantly lower BMI and VATI for all patients (p = 0.015 and 0.028), and significantly lower BMI (p = 0.048) in the PD cohort (Table 2).
At post-NAT, ductal occlusion was associated with significantly lower BMI, PNI, SATI, and VATI in all patients (p = 0.002, 0.023, 0.007, and 0.014, respectively), and significantly lower BMI, PNI, and SATI in the PD cohort (p = 0.011, 0.05, and 0.015, respectively) (Table 3).
Correlations between pancreatic morphology and post-NAT nutritional and anthropometric indices
All patients and the PD cohort showed significant correlations between pancreatic morphology and nutritional and anthropometric indices; between MPD and BMI, PNI, and SATI (inversely); between parenchyma and BMI, PMI, SATI, and VATI; and between duct–parenchymal ratio and BMI, PMI, SATI, and VATI (Table 4).
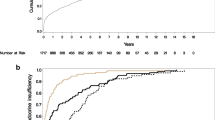
Survival analysis after PD
Median post-PD follow-up was 749.0 days (IQR, 399.0–1091.0 days) for all patients and 792.5 days (IQR, 412.0–1132.0 days) for censored patients. During the follow-up period, 41 patients died and 59 patients experienced recurrence. The occlusion group showed significantly lower postoperative 3-year survival and RFS rates (p = 0.004 and 0.013) (Fig. 2A, B).
Risk factors for survival were evaluated with univariate and multivariate analyses (Table 5). The former revealed pancreatic morphology (ductal occlusion and MPD dilation), post-NAT nutritional indices (albumin and GPS), pathological TNM and N stages, and histological grade as significant postoperative risk factors for both OS and RFS. The latter revealed pancreatic ductal occlusion as an independent postoperative risk factor for OS (hazard ratio [HR], 2.31; 95% confidence interval [CI] 1.08–4.94, p = 0.030) and RFS (HR, 2.03; 95% CI 1.10–3.72; p = 0.023).
Discussion
Our results indicate that pancreatic ductal occlusion is associated with impaired post-NAT nutritional status and adipose tissue content in patients with pancreatic head cancer undergoing NAT, and that it serves as a postoperative risk factor for PD. To our knowledge, this is the first report to describe the influence of pancreatic ductal occlusion on the treatment of pancreatic head cancer.
In other studies, NAT has been linked with impaired nutritional status and body composition, and significantly decreased PNI [15, 16], BMI and subcutaneous fat [17], visceral fat [18], and skeletal muscle and visceral and subcutaneous fat [19] in patients with pancreatic cancer. Reduced skeletal muscle and visceral fat during NAT may indicate poor prognosis [19]. In this study, the occlusion group showed significantly poorer post-NAT nutritional and anthropometric indices. This group also showed significantly larger MPD, smaller parenchyma, and greater D–P ratio and these morphological parameters significantly correlated with post-NAT nutritional and anthropometric indices. Furthermore, poorer postoperative 3-year survival and RFS rates were associated with occlusion. Given that pancreatic morphology and post-NAT nutritional indices were significant postoperative risk factors for both OS and RFS, PEI-related malnutrition during NAT may negatively affect prognosis of pancreatic head cancer patients. Pancreatic ductal occlusion was also an independent postoperative risk factor for OS and RFS, suggesting its potential as prognosticator mediated by PEI-related malnutrition.
Patients with pancreatic head cancer may develop preoperative PEI due to pancreatic ductal occlusion [20, 21], and preoperative pancreatic atrophy may lead to postoperative PEI. Preoperative CT evaluation of pancreatic morphology can thus be utilized to access PEI-related malnutrition. In patients with pancreatic cancer, the pancreatic exocrine secretory capacity reportedly begins to decline when more than 60% of the pancreatic duct is obstructed, with an exponentially greater decline when the obstruction is located closer to the ductal orifice [30]. The incidence of PEI is 44% following PD and 20% following distal pancreatectomy (DP), with corresponding postoperative prevalence rates of 74% (range, 36–100%) and 67–80% [31]. Pylorus-preserving PD reportedly yielded a significantly greater decrease in pancreatic exocrine capacity than DP, as well as a significantly greater MPD, thinner pancreatic parenchyma, and larger duct-to-parenchymal ratio in preoperative CT evaluations of pancreatic morphology [32]. In another study, patients judged to have a hard pancreas during surgery showed significantly larger MPD and smaller pancreatic parenchyma on preoperative CT images, as well as a significantly larger fibrosis ratio and smaller lobular ratio histologically, and a significantly lower incidence of POPF [33]. These reports are consistent with our findings that the occlusion group showed significantly larger MPD, smaller pancreatic parenchyma, and greater duct–parenchymal ratio in pre-NAT CT examinations and a significantly lower incidence of POPF. Furthermore, our study showed pancreatic morphology significantly correlated with nutritional and anthropometric indices, suggesting that PEI should be suspected when pancreatic-head-cancer-related ductal occlusion with concomitant CT-detectable morphological changes are observed. One study reported only 1.9% of patients with pancreatic cancer underwent PEI testing [34]. This low testing rate may be explained by difficulties in conducting relevant diagnostic tests (e.g., fecal esterase-1, coefficient of fat absorption [CFA], and 13C-mixed triglyceride breath test). CT assessments of pancreatic ductal occlusion and concomitant morphological changes thus have potential utility as practical indicators of PEI in pancreatic head cancer patients.
Pancreatic-ductal-occlusion-related PEI should be addressed during the initial phase of pancreatic head cancer management. PERT is the standard therapy for PEI; however, the effect of this therapy has primarily been investigated in unresectable pancreatic cancer or post-pancreatectomy. In one such study, patients with unresectable pancreatic cancer and suspected pancreatic ductal obstruction showed significantly improved body weight (BW) after PERT [35]. In another study, PERT significantly improved the post-pancreatectomy CFA, BW, and BMI [36]. PERT is also an independent prognosticator following PD (HR: 0.75, 95% CI 0.57–0.99, p = 0.046), significantly improving survival in patients with MPD ≥ 3 mm (HR: 0.64, 95% CI 0.47–0.89, p = 0.006), but not in those with MPD < 3 mm (HR: 1.01, 95% CI 0.66–1.55, p = 0.970) [37]. Endoscopic pancreatic stenting may also be an effective treatment option for pancreatic ductal occlusion, since it significantly delayed the development of PEI in chronic pancreatitis patients with MPD stenosis [38]. Effective treatment of PEI due to pancreatic ductal occlusion can improve nutritional status and survival outcomes; thus, evaluation of pancreatic ductal occlusion is crucial in pancreatic head cancer cases.
This study has several limitations. First, the results may have been influenced by heterogeneity such as that arising from variations in NAT regimens and duration. Second, the evaluation of the pancreatic ductal occlusion was not blinded. Third, we cannot rule out the possibility that patients assigned to the non-occlusion pre-NAT CT group developed occlusion while undergoing NAT. Fourth, some missing data were identified, but they showed no skewed intergroup distribution; thus, statistical analysis was performed with the missing data included.
In conclusion, pancreatic ductal occlusion may be linked to poorer postoperative outcomes through PEI-related malnutrition.
References
Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17–48.
Bassi C, Marchegiani G, Dervenis C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years After. Surgery. 2017;161:584–91.
Wente MN, Bassi C, Dervenis C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761–8.
Wente MN, Veit JA, Bassi C, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20–5.
Groot VP, Gemenetzis G, Blair AB, et al. Defining and predicting early recurrence in 957 patients with resected pancreatic ductal adenocarcinoma. Ann Surg. 2019;269:1154–62.
Riediger H, Keck T, Wellner U, et al. The lymph node ratio is the strongest prognostic factor after resection of pancreatic cancer. J Gastrointest Surg. 2009;13:1337–44.
Geer RJ, Brennan MF. Prognostic indicators for survival after resection of pancreatic adenocarcinoma. Am J Surg. 1993;165:68–72.
Kanda M, Fujii T, Kodera Y, et al. Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg. 2011;98:268–74.
Yamada S, Fujii T, Yabusaki N, et al. Clinical implication of inflammation-based prognostic score in pancreatic cancer: glasgow prognostic score is the most reliable parameter. Medicine (Baltimore). 2016;95:e3582.
Okumura S, Kaido T, Hamaguchi Y, et al. Impact of preoperative quality as well as quantity of skeletal muscle on survival after resection of pancreatic cancer. Surgery. 2015;157:1088–98.
Pecorelli N, Carrara G, De Cobelli F, et al. Effect of sarcopenia and visceral obesity on mortality and pancreatic fistula following pancreatic cancer surgery. Br J Surg. 2016;103:434–42.
Versteijne E, Suker M, Groothuis K, et al. Preoperative chemoradiotherapy versus immediate surgery for resectable and borderline resectable pancreatic cancer: results of the Dutch randomized Phase III PREOPANC trial. J Clin Oncol. 2020;38:1763–73.
Jang JY, Han Y, Lee H, et al. Oncological benefits of neoadjuvant chemoradiation with gemcitabine versus upfront surgery in patients with borderline resectable pancreatic cancer: a prospective, randomized, open-label, multicenter Phase 2/3 trial. Ann Surg. 2018;268:215–22.
Mokdad AA, Minter RM, Zhu H, et al. Neoadjuvant therapy followed by resection versus upfront resection for resectable pancreatic cancer: a propensity score matched analysis. J Clin Oncol. 2017;35:515–22.
Sho M, Akahori T, Tanaka T, et al. Pathological and clinical impact of neoadjuvant chemoradiotherapy using full-dose gemcitabine and concurrent radiation for resectable pancreatic cancer. J Hepatobiliary Pancreat Sci. 2013;20:197–205.
Tashiro M, Yamada S, Sonohara F, et al. Clinical impact of neoadjuvant therapy on nutritional status in pancreatic cancer. Ann Surg Oncol. 2018;25:3365–71.
Naumann P, Habermehl D, Welzel T, et al. Outcome after neoadjuvant chemoradiation and correlation with nutritional status in patients with locally advanced pancreatic cancer. Strahlenther Onkol. 2013;189:745–52.
Sandini M, Patino M, Ferrone CR, et al. Association between changes in body composition and neoadjuvant treatment for pancreatic cancer. JAMA Surg. 2018;153:809–15.
Cooper AB, Slack R, Fogelman D, et al. Characterization of anthropometric changes that occur during neoadjuvant therapy for potentially resectable pancreatic cancer. Ann Surg Oncol. 2015;22:2416–23.
Roeyen G, Berrevoet F, Borbath I, et al. Expert opinion on management of pancreatic exocrine insufficiency in pancreatic cancer. ESMO Open. 2022;7:100386.
Vujasinovic M, Valente R, Del Chiaro M, et al. Pancreatic exocrine insufficiency in pancreatic cancer. Nutrients. 2017;9:183.
Toshima F, Watanabe R, Inoue D, et al. CT abnormalities of the pancreas associated with the subsequent diagnosis of clinical Stage I pancreatic ductal adenocarcinoma more than 1 year later: a case-control study. AJR Am J Roentgenol. 2021;217:1353–64.
Motoi F, Ishida K, Fujishima F, et al. Neoadjuvant chemotherapy with gemcitabine and S-1 for resectable and borderline pancreatic ductal adenocarcinoma: results from a prospective multi-institutional phase 2 trial. Ann Surg Oncol. 2013;20:3794–801.
Okada KI, Hirono S, Kawai M, et al. Phase I study of nab-paclitaxel plus gemcitabine as neoadjuvant therapy for borderline resectable pancreatic cancer. Anticancer Res. 2017;37:853–8.
Okada K, Kawai M, Hirono S, et al. Impact of treatment duration of neoadjuvant FIRINOX in patients with borderline resectable pancreatic cancer: a pilot trial. Cancer Chemother Pharmacol. 2016;78:719–26.
Uesaka K, Boku N, Fukutomi A, et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet. 2016;388:248–57.
Evans DB, Rich TA, Byrd DR, et al. Preoperative chemoradiation and pancreaticoduodenectomy for adenocarcinoma of the pancreas. Arch Surg. 1992;127:1335–9.
Karasawa E, Goldberg HI, Moss AA, et al. CT pancreatogram in carcinoma of the pancreas and chronic pancreatitis. Radiology. 1983;148:489–93.
Mourtzakis M, Prado CM, Lieffers JR, et al. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008;33:997–1006.
DiMagno EP, Malagelada JR, Go VL. The relationships between pancreatic ductal obstruction and pancreatic secretion in man. Mayo Clin Proc. 1979;54:157–62.
Tseng DS, Molenaar IQ, Besselink MG, et al. Pancreatic exocrine insufficiency in patients with pancreatic or periampullary cancer: a systematic review. Pancreas. 2016;45:325–30.
Sato N, Yamaguchi K, Chijiiwa K, et al. Duct-parenchymal ratio predicts exocrine pancreatic function after pancreatoduodenectomy and distal pancreatectomy. Am J Surg. 1998;176:270–3.
Sugimoto M, Takahashi S, Kojima M, et al. In patients with a soft pancreas, a thick parenchyma, a small duct, and fatty infiltration are significant risks for pancreatic fistula after pancreaticoduodenectomy. J Gastrointest Surg. 2017;21:846–54.
Forsmark CE, Tang G, Xu H, et al. The use of pancreatic enzyme replacement therapy in patients with a diagnosis of chronic pancreatitis and pancreatic cancer in the US is infrequent and inconsistent. Aliment Pharmacol Ther. 2020;51:958–67.
Bruno MJ, Haverkort EB, Tijssen GP, et al. Placebo controlled trial of enteric coated pancreatin microsphere treatment in patients with unresectable cancer of the pancreatic head region. Gut. 1998;42:92–6.
Seiler CM, Izbicki J, Varga-Szabó L, et al. Randomised clinical trial: a 1-week, double-blind, placebo-controlled study of pancreatin 25 000 Ph. Eur. minimicrospheres (Creon 25000 MMS) for pancreatic exocrine insufficiency after pancreatic surgery, with a 1-year open-label extension. Aliment Pharmacol Ther. 2013;37:691–702.
Roberts KJ, Schrem H, Hodson J, et al. Pancreas exocrine replacement therapy is associated with increased survival following pancreatoduodenectomy for periampullary malignancy. HPB (Oxford). 2017;19:859–67.
Seza K, Yamaguchi T, Ishihara T, et al. A long-term controlled trial of endoscopic pancreatic stenting for treatment of main pancreatic duct stricture in chronic pancreatitis. Hepatogastroenterology. 2011;58:2128–31.
Acknowledgements
We thank Henry Smith, Specially Appointed Associate Professor, Joint Faculty of Veterinary Medicine, Kagoshima University, for advice and suggestions relating to the English terminology in this manuscript.
Funding
Open access funding provided by Kagoshima University.
Author information
Authors and Affiliations
Contributions
YH, ST, TO, and CK contributed to the study conception and design. Data collection was performed by YH, TA, and KT. Data analysis was performed by YH, ST, TO, and CK. All authors contributed to the interpretation of analyzed data. The first draft of the manuscript was written by YH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hidaka, Y., Tanoue, S., Ayukawa, T. et al. Impact of pancreatic ductal occlusion on postoperative outcomes in pancreatic head cancer patients undergoing neoadjuvant therapy. J Gastroenterol (2024). https://doi.org/10.1007/s00535-024-02125-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00535-024-02125-8