Abstract
Purpose
Refractory cancer-induced bone pain (CIBP) affects a patient’s functional capacity and quality of life, but there is limited evidence to guide opioid choice. We assessed the feasibility, tolerability and possible efficacy of methadone rotation (MR) compared to other opioid rotations (OOR) in this cohort.
Methods
Adults with CIBP and worst pain intensity ≥ 4/10 and/or opioid toxicity graded ≥ 2 on the Common Terminology Criteria for Adverse Events were randomised 1:1 to methadone or another opioid rotation. Standardised assessment tools were used at pre-defined study time points up to 14 days.
Results
Of 51 eligible participants, 38 (74.5%) consented, and 29 (76.3%, MR: 14, OOR: 15) completed the fourteen days follow-up post-opioid rotation. Both groups displayed significant reduction in average (MR: d = − 1.2, p = 0.003, OOR: d = − 0.8, p = 0.015) and worst pain (MR: d = − 0.9, p = 0.042, OOR: d = − 0.6, p = 0.048) and total pain interference score (MR: d = − 1.1, p = 0.042, OOR: d = − 0.7, p = 0.007). Oral morphine equivalent daily dose was reduced significantly in MR compared to the OOR group (d = − 0.8, p = 0.05). The incidence of opioid-related adverse events following MR was unchanged but lower in the OOR group (d = 0.9, 95% CI 0.1,1.7, p = 0.022). There were no within-group or between-group differences in satisfaction with analgesia at the end of the study.
Conclusion
This pilot study demonstrated that MR and OOR in patients with refractory CIBP are feasible, safe and acceptable to patients. Appropriately powered multi-centre randomised controlled studies are needed to confirm the efficacy of MR and OOR in this cohort.
Trial registration
ACTRN12621000141842 registered 11 February 2021.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer-induced bone pain (CIBP) is a common cancer pain syndrome, with a mixture of inflammatory, nociceptive and neuropathic pain requiring a multimodal approach to analgesia management [1]. Current treatments for CIBP include radiotherapy and radioisotopes, opioids, and co-analgesics, pharmaceuticals with antiresorptive properties, and targeted interventional procedures [2, 3]. Despite radiotherapy being the gold standard treatment for painful bone metastasis, studies estimated that 40% of patients fail to respond and only 30% experience complete pain relief [4]. Furthermore, it could take one to fifteen weeks following radiotherapy before pain reduction is observed [4].
Opioids are the foundation of cancer pain management and should be offered to treat moderate-to-severe cancer pain [5]. However, opioids remain underutilised in CIBP [2], with between 25.8% and 84% of patients with moderate-to-severe metastatic bone pain not receiving a strong opioid [6,7,8]. When an opioid is prescribed, the combination of background and breakthrough (spontaneous and incident) pain commonly seen in CIBP presents challenges in balancing analgesia and opioid adverse effects [9], with the prevalence of breakthrough cancer pain remaining at 59% [10, 11].
Animal modelling of CIBP has revealed a degree of opioid resistance and involvement of neuropathic pain mechanisms [1]. However, no clear clinical benefit has been noted with the routine use of neuropathic agents [3, 12]. A multi-centre, double-blind, randomised controlled trial (RCT) of pregabalin versus placebo in 233 patients with CIBP showed no statistically significant difference in average pain or pain interference between both groups [13]. Hence, there has been limited translation from laboratory knowledge of CIBP into clinical practice to guide the choice of analgesic treatments, including opioid choice [12].
Refractory cancer pain, whereby standard opioid and/or co-analgesic therapy provides inadequate pain relief and/or patients experience unacceptable analgesic adverse effects, is described in 10–20% of cancer patients [14]. The practice of switching from one opioid molecule to another (opioid rotation) for refractory cancer pain is widely supported in palliative care [14, 15]. Rotation to methadone is commonly considered in the management of refractory cancer pain due to methadone’s antagonistic property at the N-methyl-d-aspartate (NMDA) receptor and inhibition of serotonin and noradrenaline reuptake [15, 16].
Our preliminary retrospective study of 94 patients rotated to methadone for refractory CIBP demonstrated a reduction in pain intensity from 5.6 to 2.1, with 70% and 53% of patients achieving a ≥ 30% and ≥ 50% reduction in pain, respectively [17]. Methadone rotation (MR) resulted in a reduction in the mean number of daily breakthrough opioid analgesics, with over 70% of patients requiring an actual lower dose of methadone compared to their calculated daily methadone dose [17]. In this pilot trial, we aimed to assess the feasibility, acceptability, safety and possible efficacy of an MR compared to other opioid rotation (OOR) for patients with refractory CIBP. Changes in worst and average pain intensity, effect on pain interference, satisfaction with pain relief and change in opioid requirements will be reported. The trial was registered with the Australia New Zealand Clinical Trial Registry (ACTRN12621000141842) with a detailed study protocol previously published [18].
Method
Design and participants
This pilot, open-label, randomised, controlled trial with two parallel groups was conducted between March 2021 and March 2023 at an 850-bed metropolitan hospital in Melbourne, Australia. Convenience sampling was used to screen patients attending the palliative care and radiotherapy departments against eligibility criteria. Eligible participants were ≥ 18 years old with a cancer diagnosis, an estimated prognosis of ≥ 8 weeks and met the diagnostic criteria for CIBP as defined by The Analgesic, Anesthetic, and Addiction Clinical Trial Translations, Innovations, Opportunities, and Networks-American Pain Society (ACTTION-APS) [19]. Participants were additionally defined as having refractory CIBP if they (a) were established on a strong baseline opioid [20]; (b) had an ongoing worst pain score of ≥ 4/10 at CIBP site(s) [21]; and/or (c) demonstrated opioid toxicity, with severity grade of ≥ 2 on the Common Terminology Criteria for Adverse Events (CTCAE) v5.0 (Supplementary information 1) [22]. Participants with pain additional to CIBP were eligible for the study, but all pain assessments pertained to the sites where refractory CIBP arose.
Participants with a corrected QT interval of > 500 ms on an electrocardiogram [23], already on methadone, actively receiving radiotherapy or deemed unsuitable for clinical reasons were excluded. We initially excluded those within a week of completing radiotherapy but removed this exclusion due to recruitment challenges. Six patients were recruited prior to protocol alteration.
Study procedure and randomisation
Following written consent, participants were randomised in a 1:1 ratio using a computer-generated random number sequence with allocation concealed using sealed envelopes. Participants were enrolled and rotated in the inpatient setting from their existing opioid to racemic methadone or another strong opioid (morphine, oxycodone, or hydromorphone) based on best practice guidelines [24]. Participants and investigators were not blinded to the interventions to facilitate dose titration and mitigate the risk of toxicity. The statistician involved in data analysis was blinded to allocation during data analysis.
Opioid rotation
Opioid rotation was implemented based on published opioid conversion ratios (Supplementary information 2) [25]. For OOR, clinician investigators determined which opioid (morphine, oxycodone, or hydromorphone) to switch to depending on the participant’s opioid history, allergy profile, hepatic/renal function, and clinician preference, allowing for a 25–50% dose reduction to account for incomplete cross-tolerance [26].
MR was conducted using the rapid conversion stop-and-go method [23]. A daily dose of oral methadone (DDOM) was calculated using variable conversion ratios according to the pre-switch OMEDD, as illustrated in Supplementary information 3 [27,28,29], taking into account potential medication interactions, opioid tolerance and physiological changes affecting volume distribution [23, 25]. Racemic methadone was administered in three or four divided doses. Methadone dosing and frequency were adjusted to clinical effect and observed toxicity, with dose adjustment limited to ≤ 5 mg/ day [23], aiming for twice or thrice daily dosing on discharge.
Unlimited dosing of immediate-release (IR) and/or rapid-onset opioids (ROO) to manage breakthrough cancer pain was allowed. Titration of co-analgesic medications was restricted during the study period to ensure that the observed changes in pain intensity were attributable only to the study intervention. Adjustments to laxatives and other drugs used to manage opioid adverse effects were permitted. Participants were followed up for 14 days from the initiation of the study intervention using face-to-face or over-the-telephone assessments.
Study objectives
Feasibility was assessed by recruitment and retention rates. Considering a 20–30% attrition rate in palliative care studies, we aimed for > 70% of participants completing the study procedures by day 14 [30]. Acceptability was assessed by the rate of completed data at each study time point and patient satisfaction with analgesia at baseline, day 7 and day 14 post-opioid rotation.
Safety and tolerability of MR and OOR were evaluated using the CTCAE v.5, with grade 2 adverse effects considered moderate severity. A change in the CTCAE composite score for opioid side effects was calculated to compare safety and tolerability between the two study arms [22].
Clinical outcomes assessed were change in worst and average pain intensity on day 14, effect on pain interference, satisfaction with pain relief and overall change in opioid requirements.
Data collection and measures
Participants’ basic demographic and clinical information pertaining to cancer diagnosis, CIBP characteristics and analgesic use were obtained at baseline (Fig. 1). Data were collected at each time point via face-to-face or telephone assessment. The average and worst pain intensities were assessed as per the study procedure (Fig. 1) using a numerical rating score (NRS; 0 – no pain, 10 – most severe pain).
Study procedure. AKPS, Australia-modified Karnofsky Performance Scale; BPI, Brief Pain inventory; CTCAE, Common Terminology Criteria for Adverse Events; DN4, Douleur Neuropathique 4; ECG, electrocardiogram; EuroQOL, quality of life standardised measure; HADS, hospital anxiety and depression scale; NRS, numerical rating scale; OEI, opioid escalation index; OMEDD, oral morphine equivalent daily dose for long-acting opioid analgesia; PICF, patient information and consent form
The following standardised assessment tools were utilised as per the study protocol.
-
a)
Common Terminology Criteria for Adverse Events: measured opioid adverse events, with a composite score ranging from 0–38 [22].
-
b)
Australia-modified Karnofsky Performance Scale: measured performance status [31].
-
c)
Douleur Neuropathique 4 (DN4): assessed the neuropathic element of CIBP with a score of ≥ 4/10, suggesting the presence of neuropathic pain [32].
-
d)
Subscales of Brief Pain Inventory (BPI): assessed pain interference with daily activities (0 – does not interfere, 10 – complete interference) [33].
-
e)
Oral morphine equivalent daily dose (OMEDD): calculated to compare opioid requirements from baseline to end of study (Supplementary information 2).
-
f)
Hospital Anxiety and Depression Scale (HADS): screened for anxiety and depression [34].
-
g)
EuroQOL thermometer: rated quality of life (QOL) status from 0 (worst) to 100 (best possible) [34].
Study failure/withdrawal
Participants with severe adverse reactions secondary to MR/OOR, complications unrelated to the study intervention and those who required invasive analgesic techniques or radiation therapy during the study were withdrawn.
Sample size
With the assumption of a small effect size (0.2) between arms, we aimed to recruit a sample size of 25 per arm, as suggested by Whitehead et al. [35]. Recruitment was affected by the challenges imposed by the coronavirus-19 outbreaks, thus ceased at 38 participants.
Statistical analysis
The data analysis was performed using the complete case approach. Participants were included in the analysis if they contributed data for both baseline and day 14 assessments. Baseline differences between included and excluded participants were assessed using either the Student T-test or Wilcoxon rank-sum test for continuous data or Fisher’s exact test for categorical variables.
Summary statistics were used to describe study cohort categorical variables and either mean (SD) or median (IQR) for continuous variables. The changes in all outcomes were calculated as a difference between the baseline and the end of the study results. One-sample t-test was used to assess within-group change, while between-group differences were assessed using either the Student T-test or Wilcoxon rank-sum test for continuous data or Chi-square or Fisher’s exact test for categorical variables subject to data distribution and frequencies. Effect sizes were calculated using Cohen’s d to provide guidance about the strength of effect given the exploratory nature of this pilot work. Test for proportions was used to examine the between-group differences in the proportion of participants with ≥ 30% and ≥ 50% pain reduction at the end of the study.
Opioid escalation index (OEI%) [36], a surrogate marker of opioid responsiveness and/or opioid tolerance, was calculated using the following equation:
The oral methadone-to-oral morphine conversion ratio used to calculate OMEDD for participants in the methadone arm at day 14 was 1:4.7 [37]. The data analysis was performed using Stata17 (StataCorp LLC, College Station, TX, USA) with p < 0.05 considered statistically significant for all tests. All results have been interpreted with respect to both statistical significance and clinical relevance/importance.
Results
Feasibility: participant recruitment, characteristics and retention
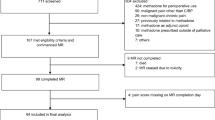
Figure 2 provides details of screening, randomisation and attrition. Of the 365 patients screened, 51 met the eligibility criteria and 38 (74.5%) consented and were randomised; 20 participants were randomised to MR and 18 to OOR (17 to hydromorphone due to clinician preference), with 14 (70.0%) and 15 (83.3%) participants completing the intervention, respectively (p = 0.454). The most common cause for study withdrawal was clinical deterioration unrelated to the intervention.
CONSORT (Consolidated Standards of Reporting Trials) participant flow diagram. MR, methadone rotation; OOR, other opioid rotation; QTc, corrected QT interval. aNine rotated from oxycodone, six from fentanyl, three rotated from morphine and two from hydromorphone. bEight rotated from fentanyl to hydromorphone, six rotated from morphine to hydromorphone, three rotated from oxycodone to hydromorphone and one rotated from hydromorphone to oxycodone/naloxone. cWithdrawn from study
Table 1 details participants’ baseline demographic and clinical characteristics. Most were female (52.6%), with a mean age of 68 (SD 11.4) years, with a diagnosis of prostate cancer (26.3%) and required occasional care assistance. The spine was the most common site of CIBP (82.9%), with 65.8% of participants reporting multiple sites of CIBP. The median worse pain intensity was 8 (IQR 6–9). Half of the participants in the MR group and two-thirds in the OOR group also had ≥ 1 opioid adverse effects graded ≥ 2, with a mean composite CTCAE score of 4 (SD 2). Commonly reported adverse effects were constipation (31.5%) and somnolence (10.5%). The median OMEDD was 85 mg (IQR 60–120), and the mean analgesic satisfaction was 68.1% (SD 22.6).
The study arms were well balanced, with the only significant difference noted for a higher anxiety and depression score [MR: 3 (IQR 1–6) vs OOR: 6 (IQR 3.3–12), p = 0.028, and MR: 4.5 (IQR 3–7) vs OOR: 9 (IQR 5–12), p = 0.029, respectively]. Supplementary information 4 details a baseline comparison between study completers and non-completers. The arms in this cohort, too, were well balanced other than for the CTCAE composite score [MR: 3.0 (SD 2) vs OOR: 4.5 (SD 1.9), p = 0.041] and anxiety score [MR: 2 (IQR 1–4) vs OOR: 6 (IQR 3–7), p = 0.013].
Acceptability: data completion at each study time point and satisfaction with analgesia
Participants completed, on average, 17 datasets in the MR arm and 16 datasets in the OOR arm across five time points following baseline data collection (Fig. 2). Neither within-group nor between-group differences in satisfaction with analgesia rating reached statistical significance (Table 2).
Safety and tolerability
Table 3 details the number of reported grade ≥ 2 adverse events and the number of affected participants in the study groups. As illustrated, in most participants, these adverse events improved or resolved by the end of the study, with only 10 participants (6 MR, 4 OOR participants) with grade 2 adverse events (constipation, somnolence, dry mouth and nausea) and no reported grade 3 adverse events at the end of the study. The mean CTCAE composite scores at the end of the study were 3.4 (SD 2.2) for the MR group and 2.7 (SD 1.8) for the OOR group. Within the OOR group, there was a significant reduction in the CTCAE composite score on day 14, with a mean group difference of 2.3 (0.4 to 4.2), d = 0.9, p = 0.022. Of note, one participant in the OOR group was withdrawn from the study on day 10 due to poorly controlled pain and dose-limiting toxicity.
Intervention outcomes
Pain characteristics
Table 2 shows the significant within-group reduction in average [MR: d = − 1.2 (95% CI − 1.9 to − 0.4), p = 0.003 vs. OOR: d = − 0.8 (95% CI − 1.5 to − 0.1), p = 0.015] and worst [MR: d = − 0.9 (95% CI − 1.6 to − 0.2), p = 0.042 vs. OOR: d = − 0.6 (95% CI − 1.3 to 0.1), p = 0.048] pain intensities, with no statistical significance between groups [d = − 0.3 (95% CI − 1.0 to 0.5), p = 0.458, for average pain intensity and d = − 0.1 (95% CI − 0.8 to 0.6), p = 0.761 for worst pain intensity]. At least a 30% reduction in average pain intensity was observed in 10 participants on methadone (71.4%; 95% CI 47.7–95.1) vs eight participants in the OOR group (53.3%; 95% CI 28.1–78.5%), a mean group difference of 18.1 (95% CI − 16.5 to 52.7, p = 0.32). Similarly, at least a 50% reduction in average pain intensity was observed in eight participants on methadone (57.1%; 95% CI 31.2–83.0%) and four participants in the OOR group (26.7%; 95% CI 4.3–64.7%), a mean group difference of 30.4 (95% CI − 3.9 to 64.7, p = 0.097). The proportions of responders were less when the worst pain intensity was assessed [MR: 35.7% with at least 30% pain reduction and 28.6% with at least 50% pain reduction vs OOR: 26.7% and 6.7%, p = 0.7 and p = 0.169, respectively). Whilst both groups displayed improvement in average and worst pain intensities by day 3, the MR group appeared to benefit from further reduction in pain intensities up to day 14 (Fig. 3). Both MR and OOR participants demonstrated a significant reduction in total pain interference [MR: d = − 1.1 (95% CI − 1.8 to − 0.3), p = 0.0420; OOR: d = − 0.7, (95% CI − 1.4 to 0.001), p = 0.007] with no significant between-group differences (p = 0.772).
Opioid requirements
OMEDD following MR reduced significantly compared to OOR [d = − 0.8 (95% CI − 1.5 to − 0.001), p = 0.05], but there was no difference in the opioid escalation index between groups (p = 0.141).
Anxiety, depression and QOL
There were no significant differences between arms in participants’ HADS-Depression (p = 0.842) or quality of life scores (p = 0.835) at the end of the study. Participants in the OOR group demonstrated a non-significant reduction in the HADS-Anxiety score at the end of the study, resulting in a significant between-group difference (d = 0.8; p = 0.043).
Discussion
This pilot randomised trial was the first reported opioid rotation study for refractory CIBP. We demonstrated study feasibility and acceptability through the enrolment of 38 participants (75% participation), with 29 participants completing the study (76.3% retention) and only three missing data points amongst the 29 study completers. We found that patients with refractory CIBP were willing to participate in a palliative-focused study and accepted randomisation. We encountered recruitment challenges where patients screened were lost to follow-up with the initial eligibility criteria, requiring participants to wait at least a week following completion of radiotherapy before enrolment. Similarly, given radiotherapy is considered the gold standard treatment for CIBP, some eligible patients declined clinical trials with concern of delaying radiotherapy, and two participants dropped out from the methadone group to proceed with radiotherapy 10 days post-opioid rotation. The unexpected challenges imposed by COVID-19 affected this study recruitment with recruitment closed prior to achieving the targeted 50 participants.
This study participants started with a low CTCAE composite score, with no significant increase in score at the end of the study, suggesting that the study interventions were tolerable and safe. The significant reduction in the CTCAE composite score in the OOR group further suggests that opioid rotation can be beneficial in reducing toxicities through improved opioid responsiveness and resultant reduction in OMEDD.
The low baseline CTCAE composite score in this study implies the practice of ‘early’ opioid rotations before the undue escalation of existing opioids to the point of dose-limiting toxicity. Despite this, we noted a significant reduction in the OMEDD post-MR, suggesting improved opioid responsiveness with methadone. In addition to its action on the mu, delta and kappa opioid receptors, incomplete cross-tolerance may result from the methadone antagonistic effect at the NMDA receptor and the inhibition of serotonin and noradrenaline reuptake [16]. These additional properties of methadone are theoretically beneficial in the modulation of neuropathic pain and prevention of chronic pain, although neuropathic pain studies have demonstrated mixed results [38,39,40]. In this study, we have noted no difference in the prevalence of assessed neuropathic pain between groups to account for the improved opioid responsiveness seen with MR.
We observed early and sustained pain reduction with MR. Methadone’s greater analgesic potency with repeated administration can be explained by its lipophilic property and phased elimination, resulting in a long and variable half-life of 8–120 h [28]. A reduction in the average pain intensity was achieved in most participants in both groups, but a significant reduction in worst pain intensity was only observed in about a third of participants on methadone and a quarter of participants rotated to another opioid. In this study, we chose at least moderate worst pain intensity as an inclusion criterion, as worst pain has been shown to have a higher correlation with most functional interference scores and has been recommended to evaluate response to radiotherapy for bone metastases [41]. Despite the relatively small proportion of participants with significant worst pain reduction, both treatment groups demonstrated a statistically significant reduction in worst pain intensity and total pain interference.
Opioid rotation, whether to methadone or another opioid, is beneficial in reducing both average and worst pain intensities and pain interference. Although not adequately powered, this study suggests that methadone rotation may have the added benefit of further reducing overall opioid requirement, providing earlier and more sustained pain reduction over 14 days with no significant worsening of opioid toxicity compared to baseline.
In considering the implementation of MR in routine clinical practice, it is important that clinicians are familiar with its pharmacokinetics and dynamics. In this study, MR was initiated in the inpatient setting with close monitoring at pre-defined intervals over 14 days. Due to the complex pharmacokinetic and pharmacodynamic profile of methadone, we would emphasise the need for ongoing monitoring beyond 14 days in the ambulatory and community palliative care setting. This requires particular attention if the stop-and-go method of rotation is used due to a higher risk of adverse effects, especially in those on high OMEDD pre-switch.
Study limitations
This study could not exclude the potential impact of concurrent oncology-specific therapy. The generalisability of this study is limited by the small sample size of single-site recruitment, with most participants in the OOR group being rotated to hydromorphone. We are not able to identify any patient variables or pain characteristics to guide the selection of opioids (methadone vs other opioids). Furthermore, we are not able to firmly conclude on the observed difference in opioid toxicity reporting between groups nor the impact of pain perception by anxiety as the observed significant differences in CTCAE composite scores and anxiety scores between groups may be accounted for by their pre-existing baseline group differences.
Given the pilot nature of this study, we chose to conduct a per-protocol analysis to provide a better estimate of the true efficacy of the study interventions and provide guidance on future studies’ sample sizes. Based on the observed small effect size on pain intensities between groups, a future sample of 123 participants in each group will be required for the study to achieve 80% power to detect a small effect size (Cohen’s d = 0.2), assuming two-sided α of 0.05. Future studies will need to consider the high attrition rate in this study population, control for anxiety/depression and the impact of radiotherapy or other concurrent oncology-specific therapy. A larger multi-centre study may also explore patient variables and/or pain characteristics that can guide opioid selection in this patient cohort. To enable multi-centre recruitment and minimise the impact of inpatient access, future studies may consider a different method of MR, such as outpatient titration [18]. Studies of outpatient MR using the stop-and-go method have also been proven to be safe [42, 43] for patients without opioid toxicity pre-switch, although pain stabilisation may be achieved after a considerably longer time [44].
Conclusion
This pilot RCT demonstrates that rotation to methadone or other opioids in patients with refractory CIBP is feasible and acceptable with comparable efficacy. Methadone rotation provided the additional benefit of lower opioid requirements. This study supports the conduct of an appropriately powered multi-centre RCT to examine the impact of methadone versus other opioid rotation for the management of refractory CIBP.
Data availability
The datasets generated during the study will be available upon reasonable request.
References
Kane CM, Hoskin P, Bennett MI (2015) Cancer induced bone pain. BMJ 350:h315. https://doi.org/10.1136/bmj.h315
Colosia A, Njue A, Bajwa Z, Dragon E, Robinson RL, Sheffield KM, Thakkar S, Richiemer SH (2022) The burden of metastatic cancer-induced bone pain: a narrative review. J Pain Res 15:3399–3412. https://doi.org/10.2147/JPR.S371337
Middlemiss T, Laird BJ, Fallon MT (2011) Mechanisms of cancer-induced bone pain. Clin Oncol (Royal College of Radiologists (Great Britain)) 23(6):387–392. https://doi.org/10.1016/j.clon.2011.03.003
van der Velden JM, van der Linden YM, Versteeg AL, Verlaan JJ, Sophie Gerlich A, Pielkenrood BJ, Kasperts N, Verkooijen HM (2018) Evaluation of effectiveness of palliative radiotherapy for bone metastases: a prospective cohort study. J Radiat Oncol 7(4):325–333. https://doi.org/10.1007/s13566-018-0363-6
Paice JA, Bohlke K, Barton D, Craig DS, El-Jawahri A, Hershman DL, Kong LR, Kurita GP, LeBlanc TW, Mercadante S, Novick KLM, Sedhom R, Seigel C, Stimmel J, Bruera E (2023) Use of opioids for adults with pain from cancer or cancer treatment: ASCO guideline. J Clin Oncol 41(4):914–930. https://doi.org/10.1200/JCO.22.02198
Body JJ, von Moos R, Rider A, Hallworth P, Bhowmik D, Gatta F, Hechmati G, Qian Y (2019) A real-world study assessing the use of bone-targeted agents and their impact on bone metastases in patients with prostate cancer treated in clinical practice in Europe. J Bone Oncol 14:100212. https://doi.org/10.1016/j.jbo.2018.100212
Kirou-Mauro AM, Hird A, Wong J, Sinclair E, Barnes EA, Tsao M, Danjoux C, Chow E (2009) Has pain management in cancer patients with bone metastases improved? A seven-year review at an outpatient palliative radiotherapy clinic. J Pain Symptom Manage 37(1):77–84. https://doi.org/10.1016/j.jpainsymman.2007.12.014
Vieira C, Fragoso M, Pereira D, Medeiros R (2019) Pain prevalence and treatment in patients with metastatic bone disease. Oncol Lett 17(3):3362–3370. https://doi.org/10.3892/ol.2019.10013
Laird BJ, Walley J, Murray GD, Clausen E, Colvin LA, Fallon MT (2011) Characterization of cancer-induced bone pain: an exploratory study. Support Care Cancer 19(9):1393–1401. https://doi.org/10.1007/s00520-010-0961-3
Deandrea S, Corli O, Consonni D, Villani W, Greco MT, Apolone G (2014) Prevalence of breakthrough cancer pain: a systematic review and a pooled analysis of published literature. J Pain Symptom Manage 47(1):57–76. https://doi.org/10.1016/j.jpainsymman.2013.02.015
van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ (2016) Update on prevalence of pain in patients with cancer systematic review and meta-analysis. J Pain Symptom Manage 51(6):1070-1090 e1079. https://doi.org/10.1016/j.jpainsymman.2015.12.340
Zajaczkowska R, Kocot-Kepska M, Leppert W, Wordliczek J (2019) Bone pain in cancer patients: mechanisms and current treatment. Int J Mol Sci 20 (23). https://doi.org/10.3390/ijms20236047
Fallon M, Hoskin PJ, Colvin LA, Fleetwood-Walker SM, Adamson D, Byrne A, Murray GD, Laird BJ (2016) Randomized double-blind trial of pregabalin versus placebo in conjunction with palliative radiotherapy for cancer-induced bone pain. J Clin Oncol 34(6):550–556. https://doi.org/10.1200/JCO.2015.63.8221
Afsharimani B, Kindl K, Good P, Hardy J (2015) Pharmacological options for the management of refractory cancer pain-what is the evidence? Support Care Cancer 23(5):1473–1481. https://doi.org/10.1007/s00520-015-2678-9
Ding H, Song Y, Xin W, Sun J, Zhong L, Zhou Q, He C, Gong L, Fang L (2022) Methadone switching for refractory cancer pain. BMC Palliat Care 21(1):191. https://doi.org/10.1186/s12904-022-01076-2
McPherson ML, Walker KA, Davis MP, Bruera E, Reddy A, Paice J, Malotte K, Lockman DK, Wellman C, Salpeter S, Bemben NM, Ray JB, Lapointe BJ, Chou R (2019) Safe and appropriate use of methadone in hospice and palliative care: expert consensus white paper. J Pain Symptom Manage 57(3):635-645 e634. https://doi.org/10.1016/j.jpainsymman.2018.12.001
Sulistio M, Wojnar R, Key S, Kwok J, Al-Rubaie Z, Michael N (2021) The role of methadone in cancer-induced bone pain: a retrospective cohort study. Support Care Cancer 29(3):1327–1335. https://doi.org/10.1007/s00520-020-05606-7
Michael N, Sulistio M, Wojnar R, Gorelik A (2023) Methadone rotation versus other opioid rotation for refractory cancer induced bone pain: protocol of an exploratory randomised controlled open-label study. BMC Palliat Care 22(1):42. https://doi.org/10.1186/s12904-023-01160-1
Paice JA, Mulvey M, Bennett M, Dougherty PM, Farrar JT, Mantyh PW, Miaskowski C, Schmidt B, Smith TJ (2017) AAPT diagnostic criteria for chronic cancer pain conditions. J Pain: Off J Am Pain Soc 18(3):233–246. https://doi.org/10.1016/j.jpain.2016.10.020
Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI, Committee EG (2018) Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Ann Oncol 29(Suppl 4):iv166–iv191. https://doi.org/10.1093/annonc/mdy152
Thong ISK, Jensen MP, Miro J, Tan G (2018) The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain 18(1):99–107. https://doi.org/10.1515/sjpain-2018-0012
Basch E, Becker C, Rogak LJ, Schrag D, Reeve BB, Spears P, Smith ML, Gounder MM, Mahoney MR, Schwartz GK, Bennett AV, Mendoza TR, Cleeland CS, Sloan JA, Bruner DW, Schwab G, Atkinson TM, Thanarajasingam G, Bertagnolli MM, Dueck AC (2021) Composite grading algorithm for the National Cancer Institute’s Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE). Clin Trials 18(1):104–114. https://doi.org/10.1177/1740774520975120
McLean S, Twomey F (2015) Methods of rotation from another strong opioid to methadone for the management of cancer pain: a systematic review of the available evidence. J Pain Symptom Manage 50(2):248-259 e241. https://doi.org/10.1016/j.jpainsymman.2015.02.029
Caraceni A, Hanks G, Kaasa S, Bennett MI, Brunelli C, Cherny N, Dale O, De Conno F, Fallon M, Hanna M, Haugen DF, Juhl G, King S, Klepstad P, Laugsand EA, Maltoni M, Mercadante S, Nabal M, Pigni A, Radbruch L, Reid C, Sjogren P, Stone PC, Tassinari D, Zeppetella G, European Palliative Care Research C, European Association for Palliative C (2012) Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol 13 (2):e58-68. https://doi.org/10.1016/S1470-2045(12)70040-2
Mercadante S, Caraceni A (2011) Conversion ratios for opioid switching in the treatment of cancer pain: a systematic review. Palliat Med 25(5):504–515. https://doi.org/10.1177/0269216311406577
Fine PG, Portenoy RK (2009) Ad hoc expert panel on evidence review and guidelines for opioid rotation. Establishing “best practices” for opioid rotation: conclusions of an expert panel. J Pain Symptom Manage. 38(3):418–25. https://doi.org/10.1016/j.jpainsymman.2009.06.002
Ayonrinde OT, Bridge DT (2000) The rediscovery of methadone for cancer pain management. Med J Aust 173(10):536–540
Leppert W (2009) The role of methadone in cancer pain treatment–a review. Int J Clin Pract 63(7):1095–1109. https://doi.org/10.1111/j.1742-1241.2008.01990.x
Soares LG (2005) Methadone for cancer pain: what have we learned from clinical studies? Am J Hosp Palliat Care 22(3):223–227. https://doi.org/10.1177/104990910502200312
Oriani A, Fusi-Schmidhauser T, Guo P (2021) Should end-of-life patients be enrolled as participants in clinical research? A best-fit framework synthesis. J Adv Nurs 77(4):1656–1666. https://doi.org/10.1111/jan.14712
Abernethy AP, Shelby-James T, Fazekas BS, Woods D, Currow DC (2005) The Australia-modified Karnofsky Performance Status (AKPS) scale: a revised scale for contemporary palliative care clinical practice [ISRCTN81117481]. BMC Palliat Care 4:7. https://doi.org/10.1186/1472-684X-4-7
Timmerman H, Steegers MAH, Huygen F, Goeman JJ, van Dasselaar NT, Schenkels MJ, Wilder-Smith OHG, Wolff AP, Vissers KCP (2017) Investigating the validity of the DN4 in a consecutive population of patients with chronic pain. PLoS ONE 12(11):e0187961. https://doi.org/10.1371/journal.pone.0187961
Andersson V, Bergman S, Henoch I, Simonsson H, Ahlberg K (2020) Benefits of using the Brief Pain Inventory in patients with cancer pain: an intervention study conducted in Swedish hospitals. Support Care Cancer 28(8):3721–3729. https://doi.org/10.1007/s00520-019-05200-6
LoMartire R, Ang BO, Gerdle B, Vixner L (2020) Psychometric properties of Short Form-36 Health Survey, EuroQol 5-dimensions, and Hospital Anxiety and Depression Scale in patients with chronic pain. Pain 161(1):83–95. https://doi.org/10.1097/j.pain.0000000000001700
Whitehead AL, Julious SA, Cooper CL, Campbell MJ (2016) Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res 25(3):1057–1073. https://doi.org/10.1177/0962280215588241
Mercadante S (1997) Malignant bone pain: pathophysiology and treatment. Pain 69(1–2):1–18. https://doi.org/10.1016/s0304-3959(96)03267-8
Walker PW, Palla S, Pei BL, Kaur G, Zhang K, Hanohano J, Munsell M, Bruera E (2008) Switching from methadone to a different opioid: what is the equianalgesic dose ratio? J Palliat Med 11(8):1103–1108. https://doi.org/10.1089/jpm.2007.0285.PMID:18980450;PMCID:PMC2982711
Hanna V, Senderovich H (2021) Methadone in pain management: a systematic review. The journal of pain : official journal of the American Pain Society 22(3):233–245. https://doi.org/10.1016/j.jpain.2020.04.004
Rigo FK, Trevisan G, Godoy MC, Rossato MF, Dalmolin GD, Silva MA, Menezes MS, Caumo W, Ferreira J (2017) Management of neuropathic chronic pain with methadone combined with ketamine: a randomized, double blind, active-controlled clinical trial. Pain Physician 20(3):207–215
Madden K, Bruera E (2017) Very-low-dose methadone to treat refractory neuropathic pain in children with cancer. J Palliat Med 20(11):1280–1283. https://doi.org/10.1089/jpm.2017.0098
Harris K, Li K, Flynn C, Chow E (2007) Worst, average or current pain in the Brief Pain Inventory: which should be used to calculate the response to palliative radiotherapy in patients with bone metastases? Clin Oncol (Royal College of Radiologists (Great Britain)) 19(7):523–527. https://doi.org/10.1016/j.clon.2007.04.007
Porta-Sales J, Garzon-Rodriguez C, Villavicencio-Chavez C, Llorens-Torrome S, Gonzalez-Barboteo J (2016) Efficacy and safety of methadone as a second-line opioid for cancer pain in an outpatient clinic: a prospective open-label study. Oncologist 21(8):981–987. https://doi.org/10.1634/theoncologist.2015-0503
Parsons HA, de la Cruz M, El Osta B, Li Z, Calderon B, Palmer JL, Bruera E (2010) Methadone initiation and rotation in the outpatient setting for patients with cancer pain. Cancer 116(2):520–528. https://doi.org/10.1002/cncr.24754
Hagen NA, Wasylenko E (1999) Methadone: outpatient titration and monitoring strategies in cancer patients. J Pain Symptom Manage 18(5):369–375. https://doi.org/10.1016/s0885-3924(99)00083-4
Acknowledgements
The authors acknowledge Ioana Logan and Gaye Moore, who provided administrative research support, Dr Ian Porter, who supported the screening of patients for the study, and the patients who willingly participated.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This research was funded by the Cabrini Foundation Sambor Research Grant. The funding body was not involved in the study’s design, data collection, analysis interpretation or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
MS, NM and DK designed the initial study; MS piloted and modified the study design; MS, HJT and NM led recruitment; MS, AG, NM and DK conducted statistical analysis; MS wrote the initial manuscript, and all authors approved the final manuscript. MS is responsible for the overall content as guarantor.
Corresponding author
Ethics declarations
Ethics approval
This study involved human participants and was approved by the Monash Health Research Ethics Committee: RES-20–0000-869C) in accordance with the National Health and Medical Research Council National Statement on Ethical Conduct in Human Research 2007 (updated 2018) Australia. Participants gave written informed consent to participate in the study before taking part.
Consent for publication
Written informed consent was obtained from all patients.
Competing interests
The authors declare no competing interests.
Provenance and peer review
Not commissioned; externally peer-reviewed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sulistio, M., Gorelik, A., Tee, H.J. et al. Methadone versus other opioids for refractory malignant bone pain: a pilot randomised controlled study. Support Care Cancer 32, 495 (2024). https://doi.org/10.1007/s00520-024-08706-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08706-w