Abstract
Purpose
Cancer-related fatigue (CRF) is a common and relevant symptom in patients with advanced cancer that significantly decreases their quality of life. The aim of this study was to evaluate the effect of a physiotherapy programme on CRF and other symptoms in patients diagnosed with advanced cancer.
Methods
The study was designed as a randomized controlled trial. Sixty patients diagnosed with advanced cancer receiving palliative care were randomized into two groups: the treatment group (n = 30) and the control group (n = 30). The therapy took place three times a week for 2 weeks. The 30-min physiotherapy session included active exercises, myofascial release and proprioceptive neuromuscular facilitation (PNF) techniques. The control group did not exercise. The outcomes included Brief Fatigue Inventory (BFI), Edmonton Symptom Assessment Scale (ESAS) and satisfaction scores.
Results
The exercise programme caused a significant reduction in fatigue scores (BFI) in terms of severity of fatigue and its impact on daily functioning. In the control group, no significant changes in the BFI were observed. Moreover, the physiotherapy programme improved patients’ general well-being and reduced the intensity of coexisting symptoms such as pain, drowsiness, lack of appetite and depression. The analysis of satisfaction scores showed that it was also positively evaluated by patients.
Conclusion
The physiotherapy programme, which included active exercises, myofascial release and PNF techniques, had beneficial effects on CRF and other symptoms in patients with advanced cancer who received palliative care. The results of the study suggest that physiotherapy is a safe and effective method of CRF management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Cancer-related fatigue (CRF) is one of the most common and complex symptoms experienced by patients diagnosed with cancer. The National Comprehensive Cancer Network (NCCN) defines CRF as “a distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity and interferes with usual functioning” [1]. Fatigue associated with cancer has a complex aetiology. It results from the interaction of two factors: those related to the disease itself or its treatment, and reduced physical activity [2, 3]. For this reason, the treatment of CRF should be multi-faceted and include, among others, physiotherapy [1]. The maintenance of physical activity plays an important role in the treatment of fatigue. The application of selected physiotherapy methods enables patients to increase their physical activity, reduce fatigue and improve their functional status, which has a direct positive impact on their quality of life [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27]. The issues of evaluating the effectiveness of physiotherapy programmes in the treatment of CRF have been the subject of interest for numerous researchers. Most studies were conducted in patient populations undergoing an intensive anticancer regime (i.e. chemotherapy or radiation therapy) or those successfully treated [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. Much less interest was devoted to the merits of inclusion of physiotherapy in the treatment of CRF in patients with advanced cancer who are not given causal treatment anymore and receive palliative care [23,24,25,26,27]. The following study constitutes an attempt to assess the advisability of including physiotherapy as a treatment for CRF in patients with advanced cancer who were receiving palliative care. The aims of the study were to assess the effect of authorial physiotherapy programme on the intensity of CRF and comorbid symptoms and to evaluate whether the patients were satisfied with such kind of treatment.
Methods
Participants
The study was designed as a randomized, controlled trial. The study protocol was approved by the Bioethics Committee of the L. Rydygier Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Torun (KB 156/2009). Participants were recruited from the Palliative Care Department, Bydgoszcz University Hospital No. 1 and from the in-patient and home care provided by the Blessed Father Popieluszko Hospice in Bydgoszcz between January 2010 and May 2011. Eligible patients admitted to the palliative care service were identified by their physicians and informed about the study. After giving their preliminary consent to participating in the study, patients were offered detailed information and had the opportunity to ask questions. Patients had 2 days to decide whether to participate, which was confirmed by their submission of written consent. The inclusion criteria were diagnosis of advanced cancer, intensity of fatigue ≥4 in a 10-point NRS (Numerical Rating Scale) obtained during the first visit, survival expectancy of a month at the very least, functional status allowing the patient to participate in the proposed therapy, ≥18 years old and written consent to participate in the study. The exclusion criteria were anaemia (haemoglobin ≤8 g/dl), the existence of comorbidities causing fatigue (e.g. multiple sclerosis, Parkinson’s disease, heart failure), infection requiring antibiotics, age <18 and inability to understand written and spoken Polish.
Randomization
Patients were randomized into the therapy group and the control group at the ratio of 1:1. Patients were assigned to respective groups using a list of numbers ranked in no particular order, with each new patient assigned a subsequent available number from the list. Even numbers designated the therapy group, while odd ones the control group.
Sample size calculation
At the planning stage of the research protocol, the number of patients required to meet the objectives of the study was specified. The following assumptions were adopted for the calculation of the number of sub-groups: normal distribution of obtained values in the sample, target test power >90% and the value of statistical significance for the difference—alpha <0.05 (type I error), beta (type II error) <10%, combined standard deviation (sigma) of 10% of the average and a two-way test of the null hypothesis assuming no differences in mean values of the studied parametres between the two groups. Moreover, the following effectiveness criteria of the therapeutic methods (differences in mean values of the evaluated parametres) were applied:
-
Comparison of two dependent means—effective final treatment effect was defined as a 25% reduction in fatigue after 2 weeks of physiotherapy [28,29,30]
-
Comparison of two independent means (therapeutic and control groups)—the final difference in fatigue severity between the therapy group and the control group was set at 25%
The required numbers were similar and totalled respectively 21 and 23. Due to the specifics of the population studied—the severity of the disease and the high risk of discontinuation of the study due to deterioration in the general condition of the patient or death, the target number of patients in each group (therapy and control) was set at 30.
Main outcome measures
The primary outcomes were use to measure the severity of fatigue and its impact on daily functioning and well-being (Brief Fatigue Inventory—BFI) and intensity of other symptoms associated with the disease (Edmonton Symptom Assessment Scale—ESAS).
The BFI has nine items, with the items measured on 0–10 numeric rating scales. Three items ask patients to rate the severity of their fatigue at its “worst”, “usual” and “now” during normal waking hours, with 0 being “no fatigue” and 10 being “fatigue as bad as you can imagine”. Six items assess the extent to which fatigue interfered with different aspects of the patient’s life during the past 24 h. The interference items include general activity, mood, walking ability, normal work (includes both work outside the home and housework), relations with other people and enjoyment of life. The interference items are measured on a 0–10 scale, with 0 being “does not interfere” and 10 being “completely interferes” [31]. The selection of this particular tool was dictated by its concise and simple form as well as the capacity to assess both the fatigue severity and its impact on patient’s daily activities.
ESAS assists in the assessment of nine symptoms common in patients diagnosed with cancer: pain, fatigue, nausea, depression, anxiety, drowsiness, appetite, well-being and breathlessness. The severity at the time of assessment of each symptom is rated from 0 to 10 on a numerical scale, 0 meaning that the symptom is absent and 10 that it is of the worst possible severity [32].
Additionally, patient satisfaction was also evaluated in the treatment group (satisfaction scores, SS). To that end, points of satisfaction were used ranging from −3 to +3 (where −3 means complete dissatisfaction, 0 no change and +3 complete satisfaction).
Additionally, data were collected on the following variables:
-
Demographic details such as gender, age and primary diagnosis
-
Karnofsky Performance Scale Index
Interventions
Patients in the therapy group were included into the physiotherapy program. During the 2-week study period, there were six therapy sessions in total (three per week). Each individual session lasted 30 min. The physiotherapy programme included active exercises of the upper and lower limbs, selected techniques of myofascial release (MFR) and selected techniques of proprioceptive neuromuscular facilitation (PNF). Physiotherapy sessions were always conducted by the same therapist, licensed in PNF method and trained in the application of myofascial release techniques.
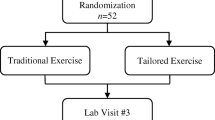
For the study design, see Fig. 1.
Parallel treatment
In line with the research protocol, no restrictions were imposed on parallel pharmacological treatment. Patients received their previous medications, which were entered in the clinical outcomes record. In the event that during the study a patient was started on a new regimen that might affect fatigue severity, it was decided that the patient should be excluded from the statistical analysis evaluating the effect of physiotherapy on CRF.
Additionally, throughout the study, the intensity of symptoms was monitored using ESAS.
The study protocol assumed that any increase in the severity of symptoms such as pain, nausea, depression, anxiety and breathlessness by at least two points on a 0–10 scale (observed during two consecutive visits) excluded a patient from the statistical analysis that assessed the effect of physiotherapy on CRF. Such an assumption was based on observations from the study by Yennu et al. and Yennurajalingam et al. [33, 34] in an advanced cancer population, which showed that the intensity of these symptoms strongly correlated with fatigue severity.
Statistical analysis
The statistical analysis of the study results was performed using Statistica 9.1 for Windows.
The obtained data are presented as mean or median values ± SD (standard deviation) or 95% CI (confidence interval). The distribution of variables was verified using the Shapiro-Wilk test. Comparisons of statistical significance of differences between the median values of parametres on successive observation days and between groups were performed using one- and two-way ANOVA (analysis of variance) with an appropriate number of repeats. In order to assess the significance of differences in the tested parametres at individual measurement points, a post hoc LSD (least significant difference) test was used. The significance of differences between mean values in the treatment and control groups was assessed using Student’s t test for independent samples (normal variable distribution) or the Mann-Whitney U test. The power of the statistical analysis was 90%; the differences between groups or the analysed time points were considered statistically significant at P < 0.05.
Results
Characteristics of study participants
The study included 60 patients (n = 60). Participants were randomized into the therapy group and the control group at the ratio of 1:1. Study groups (therapy and control) did not differ significantly with respect to age, tumour location and the study site. However, a significant gender difference was observed with respect to the assignment to the control or therapy groups, respectively (P = 0.03). Demographic and clinical characteristics of the patients qualified for the study are shown in Table 1.
Parallel treatment
In the course of the study, drug regimen was modified in two patients (one in each group) whose general condition had deteriorated, which excluded them from the study. These patients were also excluded from the statistical analysis of the impact of physiotherapy on the fatigue level. None out of the 60 patients in the study sample was on the anticancer therapy.
Discontinuation of the study
The study was discontinued for two patients (n = 1, therapy group and n = 1, control group). The cause of their death was advanced cancer. Those patients were excluded from the statistical analysis of the impact of physiotherapy on the severity of fatigue. They were the same patients who needed modified pharmacological treatment.
Effect of physiotherapy program on fatigue (BFI)
The analysis of the impact of physiotherapy program on the severity of fatigue included 29 patients from the treatment group and 29 patients from the control group. It was found that physiotherapy program significantly reduced fatigue severity in patients evaluated using the BFI. After 12 days, the results demonstrated a significant decrease in fatigue scores (BFI) compared with baseline (Wilcoxon test):
-
In the treatment group on all the questions, mean score 6.4 ± 1.0 vs. 4.4 ± 1.4, P < 0.01
-
In the control group on questions 1 and 3, mean score 6.13 ± 1.4 vs. 5.9 ± 1.44, P < 0.01
As compared with the control group, the treated individuals had significantly lower scores on the BFI on questions 1, 2, 3, 4a, 4b, 4e and 4f. Significant differences were observed on average as of day 8 of physiotherapy (Figs. 2 and 3).
Impact of physiotherapy program on the severity of fatigue and other symptoms (ESAS)
Throughout the study, the severity of symptoms was evaluated using ESAS both in the treatment and in the control groups. At baseline, no significant differences were observed regarding ESAS parametre values between the groups (Table 2). However, the comparison of scores for individual symptoms between baseline and the evaluation at the end of the study revealed a statistically significant beneficial effect of therapy in terms of reduced severity of the following: pain, fatigue, depression, anxiety, drowsiness, well-being and improved appetite (P < 0.01) (Table 3). Similar effects were not observed in the control group (Table 4). After 14 days of physiotherapy, the therapy group compared with the control group reported a statistically significant reduced severity of fatigue and drowsiness; moreover, patients in the therapy group rated their well-being higher (Table 2, Fig. 4).
Satisfaction with physiotherapy program
At the end of physiotherapy program, the mean level of patient satisfaction was 1.6 ± 0.8 (min. = 0, max. = 3). Of the 29 patients under observation, 26 rated the therapy as positive (+3, n = 3; +2, n = 14; +1, n = 9), whereas three patients rated it as neither positive nor negative.
Discussion
One of the elements of multifaceted symptom management in palliative care is physiotherapy. The main aim of physiotherapy in this patient population is to improve quality of life by way of alleviating troublesome symptoms and allowing the patients to function at an optimal level [35]. The effectiveness of physiotherapy in the treatment of selected symptoms in patients with advanced cancer has been confirmed on numerous occasions. These symptoms include, among others, myofascial pain, lymphoedema, breathlessness, constipation or motor deficits secondary to neurological disorders [36,37,38,39,40,41].
CRF is rarely recognized as an indication for physiotherapy. The effect of physiotherapy programs on CRF in patients with advanced cancer had not been extensively studied. So far, the issue of physical exercises used for relieving fatigue in patients with advanced cancer was analysed only by Porock et al., Buss et al., Oldervoll et al., Van den Dungen et al. and Cheville et al. [24,25,26,27,28]. In their study, Porock et al. [24] included only 11 patients with advanced cancer, suffering from fatigue. The study lasted 28 days and patients did not follow a single exercise therapy. The therapy involved exercises in bed, exercises in a sitting position, treadmill walking, cycle-ergometer exercises and dancing to the rhythm of favourite music. The exercise programs were tailored to the needs and physical capacity of individual patients. Therefore, individual interventions differed significantly in duration (ranging from 22 to 180 min per week). Although the authors did not observe any significant reduction in fatigue levels within the studied group, they pointed to the fact that the therapy regimens patients received did not increase their fatigue levels. Furthermore, the applied therapy regimens were positively evaluated by the patients, as they tangibly increased patients’ daily physical activity. Buss et al. also attempted to assess the effectiveness of exercise interventions in reducing fatigue in the terminal hospice cancer patients [25]. They assessed the effect of a single, well-defined, reproducible across the entire group of patients’ exercise program on quality of life and fatigue in the hospice terminal cancer patients. The study group comprised 38 patients. Their analysis showed that, on average, after 3 weeks of a physical therapy exercise program, a significant decrease in fatigue levels was observed, while in the control group, it increased after 2 weeks of observation. It should be noted, however, that patients with short life expectancy (approx. 1–2 months) were among those admitted into the study by Buss et al. A similar criterion was used in the present study, i.e. approx. 1–3 months. For that reason, a timeline for the study was set at 2 weeks. Extending time frames of interventions in the case of short life expectancy patients increases a risk of their non-completion of a study. This is usually associated with deterioration of general condition, disease progression or death. Oldevoll et al. [26] pursued their study for 8 weeks. Patients with advanced cancer with a life expectancy <2 years were included in the study. Out of 231 patients, 68 (29%) were lost as a result of disease progression. The study evaluated the effects of a group exercise intervention, supervised by a physiotherapist. The exercise group had two exercise sessions per week over an 8-week period. Each session lasted 50–60 min and included a warm-up (10–15 min), circuit training with six stations (30 min) and stretching/relaxation (10–15 min). The analysis showed no significant reduction in fatigue levels in the study group. The applied intervention enhanced physical performance. The gait and muscle strength test results were significantly improved after 8 weeks of physical exercise. Improvement in physical fitness was also noted by van den Dungen et al. [27]. Their non-randomized pilot study comprised 26 palliative care patients with advanced cancer. Participants followed an individually graded group exercise program, consisting of resistance training and aerobic exercise, twice a week during 6 weeks. Apart from improved physical fitness, the authors observed improved quality of life and reduced fatigue in patients. Cheville et al. [28] assessed the effectiveness of a home-based physiotherapy. Sixty-six adults with stage IV lung or colorectal cancer were admitted into the study. They were randomized, in an 8-week trial, to usual care or incremental walking and home-based strength training. The exercising participants were instructed during a single physiotherapy visit and subsequently exercised 4 days or more per week; training and step-count goals were advanced during bimonthly telephone calls. A home-based exercise program seems capable of improving the mobility, fatigue and sleep quality of patients with stage IV lung and colorectal cancer.
Much more research on the evaluation of physiotherapy treatment in terms of CRF reduction was conducted in populations of patients undergoing an intensive oncological regimen and those who have been successfully treated. Results of research in this area show that the treatment groups achieve a statistically more effective fatigue reduction compared with controls. The authors have identified exercise as a beneficial and valuable form of treatment for fatigue among patients undergoing intensive anticancer therapy and patients with chronic fatigue that persists despite completed oncological treatment. At the same time, they signalled the need for research aimed at optimizing the type, intensity and duration of specific therapeutic interventions. The need to develop clear guidelines on the use of physiotherapy in the treatment of fatigue was also confirmed by a survey conducted among British physiotherapists working with cancer patients and members of the Association of Chartered Physiotherapists in Oncology and Palliative Care (ACPOPC) [42].
Studies evaluating the effectiveness of selected physiotherapy methods in the treatment of fatigue support the use of this form of therapy among patients diagnosed with cancer. However, there are substantial differences among individual researchers concerning the duration of the therapy and its frequency. The authors of the publications studied, among others, the effectiveness of an exercise regimen carried out individually or in groups 2–7 times a week for 2–8 weeks. The duration of a single therapy session ranged from 20 to 90 min. The protocol adopted for the present study included 30-min physiotherapy sessions three times a week for 2 weeks. The planned follow-up period proved to be long enough to observe changes in fatigue severity due to physiotherapy, since statistically significant differences were already observed on average as of day 8 of the intervention. Simultaneously, in the vast majority of patients (n = 58), there was no disease progression or increased severity of symptoms; hence, they did not require additional pharmacological treatment. The comparison of ESAS scores between baseline and the day the observation ended showed statistically significant beneficial effects of the physiotherapy. It may have had a significant impact on the high level of treatment satisfaction.
The proposed physiotherapy program, including active exercises of upper and lower extremities, selected techniques of myofascial relaxation and PNF, was devised by the author of the study. The selection of individual components of the treatment program reflected the desire to devise a treatment plan specially tailored to the condition of the patients participating in the study. However, the formulation of specific guidelines on physical therapy programs used as part of fatigue treatment requires more research. In most published studies, the selection of specific physiotherapy techniques is quite varied. Therapies include, among others, active exercises (resisted and unresisted), balance exercises, breathing and relaxation and ergometer training [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27]. The selection of specific therapies should be based on a careful individual analysis of the potential and limitations of particular patients. This is especially important in a population of patients diagnosed with advanced cancer receiving palliative care. They tend to be reluctant to undertake physical activity giving reasons such as limited fitness and functional capacity [43]. Moreover, in this population, fatigue is often accompanied by the anorexia-cachexia syndrome. The patient who notes a progressive loss of body mass and suffers from anorexia, whose fatigue increases with each movement, may at first refuse to participate in any treatment proposed by a physiotherapist for fear that his/her exhaustion may increase. Hence, the physiotherapy program should include both the treatment elements that do not require large expenditures of energy on the part of the patients and methods that actively engage them. For this reason, the proposed program included relaxation techniques (myofascial relaxation, breathing stimulation) and more active methods (active exercises, selected PNF techniques).
The rationale for the use of this kind of fatigue treatment programs was evaluated in studies conducted by Fernández-Lao et al. [44, 45] among patients with breast cancer once they completed their anticancer treatment. The proposed physiotherapy regime included core stability exercises and elements of myofascial release. Results of the study indicate a high effectiveness of the proposed physiotherapy program in relieving fatigue and other symptoms associated with anxiety and depression. Moreover, the treatments improved the patients’ muscle strength and their overall fitness. Similar positive therapeutic effects were not observed in the control group.
In devising physiotherapy programs for the treatment of fatigue, it is very important to include simple exercises easy to remember by the patient. The inclusion of such therapy forms is of great importance since they can be used as part of movement activation exercises to be performed by each patient individually.
The results of the present study clearly demonstrate that cancer-related fatigue in patients with advanced cancer constitutes an indication for the inclusion of physiotherapy in their non-pharmacological treatment. However, the issue requires more detailed research involving large groups of advanced cancer patients receiving palliative, hospice and home care, respectively.
The main limitation of the study was the fact that despite the randomization, the process of group assignment itself showed a significant association with gender (P = 0.03). It is worth noting, however, that there was no significant correlation between gender and the effect of physiotherapy on the severity of fatigue.
Conclusions
The proposed physiotherapy program significantly reduces the severity of fatigue in patients diagnosed with advanced cancer receiving palliative care. Additionally, this program improves the general well-being of patients and reduces the severity of their comorbid symptoms, especially pain, drowsiness, loss of appetite and depression. The proposed physiotherapy program was positively rated by patients who completed treatment satisfaction questionnaire. Non-pharmacological treatment of fatigue in advanced cancer patients receiving palliative care should include an appropriate selection of physiotherapy methods.
ANOVA, analysis of variance; BFI, Brief Fatigue Inventory; CI, confidence interval; CRF, cancer-related fatigue; ESAS, Edmonton Symptom Assessment Scale; LSD, least significant difference; MFR, myofascial release; NCCN, National Comprehensive Cancer Network; NRS, Numerical Rating Scale; P, borderline level of statistical significance; PNF, proprioceptive neuromuscular facilitation; SD, standard deviation; SS, satisfaction scores
Change history
15 June 2017
An erratum to this article has been published.
References
NCCN Clinical practice guidelines in oncology: cancer-related fatigue, version I.2017 - December 19, 2016 https://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf. Accessed 22 Jan 2017
Winningham ML, Nail LM, Burke MB et al (1994) Fatigue and cancer experience. Oncol Nurs Forum 2:23–36
Peters ME, Goedendorp MM, Verhagen CA et al (2016) Fatigue and its associated psychosocial factors in cancer patients on active palliative treatment measured over time. Support Care Cancer 24:1349–1355. doi:10.1007/s00520-015-2909-0
Windsor PM, Nicol KF, Potter J (2004) A randomized controlled trial of aerobic exercise for treatment-related fatigue in men receiving radical external beam radiotherapy for localized prostate carcinoma. Cancer 3:550–557
Mock V, Dow KH, Meares C et al (1997) Effects of exercise on fatigue, physical functioning and emotional distress during radiation therapy for breast cancer. Oncol Nurs Forum 24:991–1000
Schwartz A, Mor M, Gao R et al (2001) Exercise reduces daily fatigue in women with breast cancer receiving chemotherapy. Med Sci Sports Exerc 33:717–723
Segal R, Reid R, Courneya KS et al (2003) Resistance exercise in men receiving androgen deprivation therapy for prostate cancer. J Clin Oncol 21:1653–1659
Duijts SF, Faber MM, Oldenburg HS et al (2011) Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors—a meta-analysis. Psychooncology 2:115–126
Losito JM, Murphy SO, Thomas ML (2006) The effects of group exercise on fatigue and quality of life during cancer treatment. Oncol Nurs Forum 4:821–825
Campbell A, Mutrie N, White F et al (2005) A pilot study of a supervised group exercise program as a rehabilitant treatment for women with breast cancer receiving adjuvant treatment. Eur J of Oncol Nurs 9:56–63
Courneya KS, Mackey JR, Jones LW (2000) Coping with cancer. Can exercise help? Phys Sportsmed 28:49–73
Courneya KS, Segal R, Mackey J et al (2007) Effect of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. J Clin Oncol 25:4396–4404
Adamsen L, Midtgaard J, Rorth M et al (2003) Feasibility, physical capacity, and health benefits of a multidimensional exercise program for cancer patients undergoing chemotherapy. Support Care Cancer 11:707–716
Conn V, Hafdahl A, Porock D et al (2006) A meta-analysis of exercise interventions among people treated for cancer. Support Care Cancer 14:699–712
Cramp F, Daniel J (2008) Exercise for the management of cancer-related fatigue in adults (review). Cochrane Database Sys Rev. doi:10.1002/14651858.CD006145
Knobel H, Loge JH, Nordøy T et al (2000) High level of fatigue in lymphoma patients treated with high dose therapy. J Pain Symptom Manag 6:446–456
Bower JE, Ganz PA, Aziz N et al (2003) T-cell homeostasis in breast cancer survivors with persistent fatigue. J Natl Cancer Inst 15:1165–1168
Fosså SD, Dahl AA, Loge JH (2003) Fatigue, anxiety, and depression in long-term survivors of testicular cancer. J Clin Oncol 7:1249–1254
Rüffer JU, Flechtner H, Tralls P et al (2003) Fatigue in long-term survivors of Hodgkin’s lymphoma; a report from the German Hodgkin Lymphoma Study Group (GHSG). Eur J Cancer 15:2179–2186
Weert E, Hoekstra-Weebers J, Otter R et al (2006) Cancer-related fatigue: predictors and effects of rehabilitation. Oncologist 11:184–196
Courneya KS, Mackey JR, Bell GJ et al (2003) Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulmonary and quality of life outcomes. J Clin Oncol 9:1660–1668
Dimeo CF, Thomas F, Raabe-Manssen C et al (2004) Effect of aerobic exercise and relaxation training on fatigue and physical performance of cancer patients after surgery. A randomized controlled trial. Support Care Cancer 12:774–779
Porock D, Kristjanson LJ, Tinnelly K et al (2000) An exercise intervention for advanced cancer patients experiencing fatigue: a pilot study. J Palliat Care 3:30–36
Buss T, de Walden-Gałuszko K, Modlińska A (2010) Kinesitherapy alleviates fatigue in terminal hospice cancer patients—an experimental, controlled study. Support Care Cancer 6:743–749
Oldervoll LM, Loge J, Lydersen S et al (2011) Physical exercise for cancer patients with advanced disease: a randomized controlled trial. Oncologist 16:1649–1657
van den Dungen IA, Verhagen CA, Van den Graaf WT et al (2014) Feasibility and impact of a physical exercise program in patients with advanced cancer: a pilot study. J Palliat Med. doi:10.1089/jpm.2013.0638
Cheville AL., Kollasch J, Vandenberg J et al. (2012) A home-based exercise program to improve function, fatigue, and sleep quality in patients with IV stage lung cancer and colorectal cancer: a randomized controlled trial. doi: 10.1016/j.jpainsymman.2012.05.006
Reddy S, Bruera E, Pace A et al (2007) Clinically important improvement in the intensity of fatigue in patients with advanced cancer. J Palliat Med 5:1068–1075
Cella D, Eton DT, Lai JS et al (2002) Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manag 24:547–561
Patrick DL, Gagnon DD, Zagari MJ (2003) Assessing the clinical significance of health-related quality of life (HRQoL) improvements in anaemic cancer patients receiving epoetin alfa. Eur J Cancer 39:335–345
Mendoza TR, Wang XS, Cleeland CS et al (1999) The rapid assessment of fatigue severity in cancer patients. Use of the Brief Fatigue Inventory. Cancer 85:1186–1196
Bruera E, Kuehn N, Miller MJ et al (1991) The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 7:6–9
Yennu S, Urbauer DL, Bruera E (2012) Factors associated with the severity and improvement of fatigue in patients with advanced cancer presenting to an outpatient palliative care clinic. BMC Palliative Care 11:16. doi:10.1186/1472-684X-11-16
Yennurajalingam S, Palmer JL, Zhang T et al (2008) Association between fatigue and other cancer-related symptoms in patients with advanced cancer. Support Care Cancer 16:1125–1130
Tookman AJ, Hopkins K, Scharpen-von-Heussen K (2004) Rehabilitation in palliative medicine. In: Doyle D, Hanks G, Cherny N, Calman K (eds) Textbook of palliative medicine, 3rd edn. Oxford University Press, Oxford, pp 1021–1032
Hately J, Laurence V, Scott A et al (2003) Breathlessness clinics within palliative care settings can improve the quality of life and functional capacity of patients with lung cancer. Palliat Med 17:410–417
Belletti M, Mallia L, Lucidi F et al (2010) Complementary therapy and support services for formal and informal caregivers in Italian palliative care hospices: an exploratory and descriptive study. doi: 10.1007/s00520-010-1034-3
Cassileth BR, Vickers AJ (2004) Massage therapy for symptom control: outcome study at a major cancer centre. J Pain Symptom Manag 3:244–249
Polubiński JP, West L (2005) Implementation of a massage therapy program in the home hospice setting. J Pain Symptom Manag 1:104–106
Preece J (2002) Introducing abdominal massage in palliative care for the relief of constipation. Compl Ther Nurs Midwifery 8:101–105
Pyszora A, Wójcik A, Krajnik M (2010) Are soft tissue therapies and Kinesio Taping useful for symptom management in palliative care? Three case reports. Adv Pall Med 3:89–94
Donnelly CM, Lowe-Strong A, Rankin JP et al (2010) Physiotherapy management of cancer-related fatigue: a survey of UK current practice. Support Care Cancer 7:817–825
Blaney J, Lowe-Strong A, Rankin J et al (2010) The cancer rehabilitation journey: barriers to and facilitators of exercise among patients with cancer-related fatigue. Phys Ther 8:1135–1147
Fernández-Lao C, Cantarero-Villanueva I, Díaz-Rodríguez L et al (2012) Attitudes towards massage modify effects of manual therapy in breast cancer survivors: a randomized clinical trial with crossover design. Eur J Cancer Care 2:233–241
Cantarero-Villanueva I, Fernández-Lao C, Del Moral-Avila R (2012) Effectiveness of core stability exercises and recovery myofascial release massage on fatigue in breast cancer survivors: a randomized controlled clinical trial. Evid Based Complement Alternat Med. doi:10.1155/2012/620619
Acknowledgments
The authors thank all medical and nursing staff of the Blessed Father Jerzy Popieluszko Hospice in Bydgoszcz and of the Palliative Care Department, University Hospital No. 1 in Bydgoszcz, where patients were recruited. Finally, the authors wish to thank all the participating patients.
Author information
Authors and Affiliations
Contributions
AP conceived the idea for the study. AP, MK, JB and AW contributed to the design of the research. AP and APr were involved in data collection. AP, MK and JB analysed the data. MK coordinated funding for the project (institutional funding). All authors edited and approved the final version of manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Funding
Funding for this study was provided by the Nicolaus Copernicus University Collegium Medicum, Bydgoszcz, Poland (institutional funding).
Consent for publication
Not applicable.
Ethical approval and consent to participate
Written informed consent was obtained from all participants. Confidentiality and anonymity were guaranteed. The study protocol was approved by the Bioethics Committee of the L. Rydygier Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Torun (KB 156/2009).
Additional information
An erratum to this article is available at https://doi.org/10.1007/s00520-017-3779-4.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Pyszora, A., Budzyński, J., Wójcik, A. et al. Physiotherapy programme reduces fatigue in patients with advanced cancer receiving palliative care: randomized controlled trial. Support Care Cancer 25, 2899–2908 (2017). https://doi.org/10.1007/s00520-017-3742-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3742-4