Abstract
Extreme heat alerts are the most common form of weather forecasting services used in Australia, yet very limited studies have documented their effectiveness in improving health outcomes. This study aimed to examine the temporal changes in temperature-related mortality in relation to the activation of the heat-health alert and response system (HARS) in the State of Victoria, Australia. We examined the relationship between temperatures and mortality using quasi-Poisson regression and the distributed lag non-linear model (dlnm) and compared the temperature-mortality association between the two periods: period 1– prior-HARS (1992–2009) and period 2– post-HARS (2010–2019). Since the HARS heavily weights heatwave effects, we also compared the main effects of heatwave events between the two periods. The heatwaves were defined for three levels, including 3 consecutive days at 97th, 98th, and 99th percentiles. We also controlled the potential confounding effect of seasonality by including a natural cubic B-spline of the day of the year with equally spaced knots and 8 degrees of freedom per year. The exposure-response curve reveals the temperature mortality was reduced in period 2 in comparison with period 1. The relative risk ratios (RRR) of Period 2 over Period 1 were all less than one and gradually decreased from 0.86 (95% CI, 0.72–1.03) to 0.64 (95% CI, 0.33–1.22), and the differences in attributable risk percent increased from 13.2 to 25.3%. The reduction in the risk of heatwave-related deaths decreased by 3.4% (RRp1 1.068, 95% CI, 1.024–1.112 versus RRp2 1.034, 95% CI, 0.986–1.082) and 10% (RRp1 1.16, 95% CI, 1.10–1.22 versus RRp2 1.06, 95% CI, 1.002–1.119) for all groups of people. The study indicated a decrease in heat-related mortality following the operation of HARS in Victoria under extreme heat and high-intensity heatwaves conditions. Further studies could investigate the extent of changes in mortality among populations of differing socio-economic groups during the operation of the heat-health alert system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The burden of disease and deaths attributable to extreme heat is increasing across different geographical scales because of climate change (Ebi et al. 2021; Zhao et al. 2021).
In the past three decades, populations across America, Australia, New Zealand, and Europe have been severely affected by the more frequent heatwaves expected to be attributed to anthropogenic climate change (Lemonsu et al. 2015; Chapman et al. 2017; Kotharkar and Ghosh 2022). In Australia, recent studies suggest that extreme heat is associated with an increase in the risk of ambulance demand, hospital admissions, and deaths, particularly among populations > 65 years and children under 5 years (Watson et al. 2020; Campbell et al. 2021; Franklin et al. 2023; Wondmagegn et al. 2021). These impacts have been observed in both the urban (Cheng et al. 2018; Guo et al. 2017; Hansen et al. 2008; Loughnan et al. 2010b) and rural areas (Loughnan et al. 2010a), strengthening the argument that Australian populations are vulnerable to extreme heat events regardless of the location. Regarding temporal changes in heat-related health effects, the study by Gasparini et al. (2015) assessed the changes mortality in Sydney and Melbourne city due to the low statistical power when comparing the effects between the two periods 1988–1998 and 1999–2009.
In response to rapidly rising number of extreme heat events, national and state governments have developed and operated heat-health warning systems (HHWS). These have been proven successful in reducing heat-related mortality in most high income nations, especially in some European countries (Martinez et al. 2022), the United States (Bobb Jennifer et al. 2014), and the United Kingdom (Lo et al. 2022). The effectiveness of the HHWS in improving health outcomes varies significantly by temporal changes in the temperature-response relationship, and health outcome among populations over time (Kotharkar and Ghosh 2022). For example, heat alerts may not necessarily decrease the risk of mortality, but could encourage individuals (especially those with fluid and electrolyte disorders) to seek medical care, suggesting increasing hospital admissions(Weinberger et al. 2021). Others have also found a high degree of heterogeneities about the effectiveness of HHWS in reducing mortalities among different regions(Díaz et al. 2019).
Assessment of the HHWS over time will provide information on their efficacy as a public health intervention tool during extreme weather events. Australia has seen an increase in frequency and severity of extreme heat events increasing over the last 100 years (Coates et al. 2014) and their associated health consequences such as fatalities and morbidities (Zhang et al. 2020; Coates et al. 2022). These record-breaking heat events have been observed in multiple cities in Australia making it an important public health concern (Beggs et al. 2021; Bi et al. 2011; Pezza et al. 2012). Although HHWS have been developed and operated in most jurisdictions in Australia in the last decade (Williams et al. 2019), no study has attempted to examine their effectiveness.
The Victorian Department of Health established a heat-health alert and response system (HARS) in 2009–2010 and reviewed its implementation in 2012–2013 (Williams et al. 2019). The HARS uses the forecast temperature to issue heat-health alerts for the specific district once the temperature exceeds the threshold which heat-related illness and mortality. This threshold is the 95th percentile 3 day moving average derived from 30 years of temperature data. This study aims to examine the temperature-related mortality over time including the HHWS intervention in Victoria, Australia over the 1992–2009 (prior-HARS) and 2010–2019 (post-HARS) time periods.
Methods
Research locations
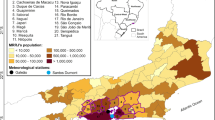
This study was conducted in the state of Victoria in South-Eastern Australia. Victoria is the second-smallest State by land area of 227,44 km2, but it is the most densely populated state in Australia (28 per km2) with a total population of more than 6.5 million (Australian Bureau of Statistics 2021a). The state has 9 geographical districts including 96 cities and counties (Fig. 1). The climate of this state ranges from semi-arid temperature with hot summers in the northwest, to temperate and cool along the coastal areas (Beck et al. 2018). The temperatures in summer range between 14 and 25.3 °C (December-February). According to Loughnan et al. (2010a), extreme heat is considered one of the most significant health hazards facing Victoria, and it causes exacerbation of pre-existing conditions in the population and may result in increased propensity of heat-related mortality among vulnerable populations especially the elderly (> 65 years). For example, 374 and 167 excess deaths were recorded during the bushfire-induced heatwaves in 2009 and 2014 in Victoria (Victoria Government 2020).
Weather forecast districts and corresponding heat health temperature thresholds. (Source: Extreme Heat Sub-plan for Victoria (2017))
Data
Daily count of all-cause death data for Victoria residents during January 1996-December 2015 (inclusive) were obtained from the Australian Bureau of Statistics (ABS). This mortality data covers nearly 78.5% of Victorian population living in central part of the State. The data includes the number of deaths for all causes for the State of Victoria by date of death, sex, and age groups (0–15, 16–64, 65–74, 75–84, and 85+).
Data on temperatures were obtained from the Bureau of Meteorology for the Melbourne Airport weather station (144.844788,-37.663712) which locates in the city of Melbourne in the southern part of the central forecast district area of Victoria, where 5.1 million of 6.5 million Victorian residents reside. The data includes daily maximum and minimum temperatures from 1st Jan 1992 to 15th December 2019. To evaluate the temporal change in heat-related mortality in relation to the HARS operational date, we used the average temperature which was calculated from the maximum temperature of one day and the minimum temperature for the following day (Extreme Heat Sub-plan for Victoria 2017). The Victorian Health Department is using this calculation method using the forecast temperatures for HARS (Extreme Heat Sub-plan for Victoria 2017).
The heat-health plan for Victoria (HHP-V) (Victoria Government 2020), which has been developed since 2009–2010, guides how the State Department of Health and Human Services works together with local government and health and human services sectors to promote public health and wellbeing before and during periods of extreme heat (3 days of 95th percentile temperatures). The HHP-V has three main objectives: (i) protect the health of Victorians from heat-related harm; (ii) communicate the actions of the department to prepare for and respond to extreme heat; (iii) outline preparedness and response activities for local government and the health and human services sectors to reduce the impact of extreme heat on Victorians (Victoria Government 2020). The key element of the HHP-V is the HARS which has been developed to notify the stakeholders (local councils, departmental program areas, hospitals, and health and community service providers) that the average temperature is predicted to reach and exceed heat-health thresholds. The thresholds are identified by a range of evidence and information and vary across Victoria to recognize the higher temperatures experienced in its northern parts. A heat health temperature threshold has been established for each of the nine weather forecast districts (Fig. 1). The average temperature for any given day is calculated as the mean of the forecast daily maximum temperature and the forecast overnight minimum temperature (which is the daily minimum for the following day). When the forecast average temperatures are predicted to reach or exceed the heat health temperature threshold of 30–34℃ depending on specific weather forecast district, the State government department would issue a heat health alert for that district. Among the most common actions taken by the department during extreme heat days includes media notification/release, messaging (via digital platforms and via radio, television), monitoring of health system demands, involvement of local community organization to increase heat-health information dissemination, ensures the availability of adequate cool spaces/water, and monitoring of weather systems (Victoria Government 2020).
Statistical analysis
We examined the relationship between the temperature and mortality counts using quasi-Poisson regression and the distributed lag non-linear model (DLNM ) framework (Gasparrini 2014). This method is warranted as it captures the non-linear and delayed effects (lagged association) which are the typical characteristics of heat-health response, using basis functions (Martínez-Solanas and Basagaña 2019). Since the HARS was established and operated in 2009–2010, we conducted data analysis separately for two periods, period 1 (1992–2009) and period 2 (2010–2019).
The exposure-response association was regressed using a quadratic B-spline with 3 internal knots placed at the 10th, 75th, and 90th percentiles of temperature distribution (Ngandu et al. 2015). The potential confounding effect of seasonality was controlled by including a natural cubic B-spline of the day of the year with equally spaced knots and 8 degrees of freedom per year. An interaction between this spline function and the variable of the year was specified to relax the assumption of a constant seasonal trend. We controlled the effects of long-term trends and the week’s days by incorporating a linear term for a year and the variable for a day of the week into the model. The lag-response association was modelled using a natural cubic B-spline with an intercept and three internal knots placed at equally spaced values in the log scale. The lag period was extended up to 21 days including possible long delays in the effects of the temperature (Martínez-Solanas and Basagaña 2019; Davis et al. 2023). The overall cumulative effects of temperature for all lags were then plotted to visually examine the difference in the temperature-mortality association between the two periods.
To compare the temperature-mortality association between the two periods, we estimated the relative risk (RR) and an attributable fraction (AF) for the temperatures above 30oC, which was the lowest temperature threshold used for the HARS, relative to the reference temperature at 22.5oC that was identified from the previous study (Gasparrini et al. 2015). The relative risk ratio (RRR) and differences in AF between the two periods were then estimated. Since the HHP-V heavily weights heatwave effects, we also compared the main effects of heatwave events between two periods. The heatwaves were defined for three levels, including 3 consecutive days at 97th, 98th, and 99th percentiles which are in line with the heatwave definitions by the HHP-V (Victoria Government 2020; Tong et al. 2015). The main effects of heatwaves were calculated using the models using the same cross-basis function of the average temperature described above. The details on how to quantify the main effects of heatwaves were described elsewhere (Gasparrini and Armstrong 2011). The comparison of the effects between the two periods was analyzed by sex and age groups (16–74, 75+). The analyses on two heatwave periods ( period 1:1992–2009, and period 2:2010–2019) were restricted to the summer only (December to February), a major season where heat-related deaths normally occur in Australia (Coates et al. 2014).
We conducted several sensitivity analyses to examine the robustness of our findings. First, we determine how significant of a break point the implementation of the current HARS periods. We applied the same study design, and arbitrarily defined HARS at different periods of implementation: (i) 1992–2005 as period 1– prior-HARS, and (ii) 2006–2019 as period 2– post-HARS implementation at lag 21 days. Second, we examined whether changes in temperature-mortality relationships were not underestimated between period 1 (1992–2009), and period 2 (2010–2019) by expanding the analyses at three different shorter lag periods (i.e. lag 4 days, lag 7 days, lag 14 days), since adverse health effects of heatwave normally last for few days. In both analyses, heatwaves were defined for three levels, including 3 consecutive days at the 97th, 98th, and 99th percentiles (Benmarhnia et al. 2016a). All analyses were performed with R (version 4.1.2) and Stata (version 17).
Results
Descriptive statistics
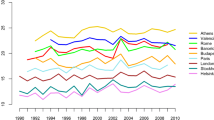
The descriptive statistics of the study population and temperatures by period are shown in Table 1. The total number of deaths that occurred between 1992 and 2019 was 978,690 with a mean of 96 (SD, 15) deaths per day. The average number of daily deaths (ANDD) was higher in period 2 (105 ± 14 versus 91 ± 13), reflecting an increase in the total population (an increase of 2,138,661 inhabitants during the study period) (Australian Bureau of statistics 2019). While the ANDD was stable for the age group of 16–74, it was higher in period 2 for the older people at 75-year-old and above (72 ± 11 versus 56 ± 11). In terms of sex, the daily counts of mortality were equally higher in period two for both males and females. The temporal decrease in the mortality rate over time in period 1 (-0.11/1,000,000 persons/ year) was approximately similar to that observed in period2 (-0.1/1,000,000 persons/year). Both the means of daily average maximum and minimum temperatures were higher in period 2 (7.9 °C versus 8.3 °C and 19.9 °C versus 20.6 °C) (Table 2). This is also seen in the temporal pattern of the average daily temperature between two periods shown in Fig. 2.
Change in the temporal pattern of the temperature-mortality association in the two periods
The pattern of the relationship between average temperature and the risk of death in the two periods is shown in the overall cumulative exposure-response curve in Fig. 3. For both periods, the curves had a J-shape, reflecting a rapid increase in risk of mortality as average daily temperaturees increased. The risk of deaths associated with cold temperatures was reduced substantially, especially the effect of extreme cold at a temperature less than the 5th percentile (8.2oC) disappeared in period 2 while this effect was found significant in period 1. For the effect of higher temperatures, the slope of the risk of mortality curve was reduced in period 2 in comparison with period 1 although the confidence intervals for the higher temperatures in the two periods overlapped. The threshold of the elevated temperature-mortality was observed at 29oC which was significantly higher than the threshold observed in period 1 (27oC). It is noteworthy that the thresholds of both periods were lower than the minimum threshold (30oC) used for the activation of HARS in Victoria.
The comparison of relative risk and attributable fraction were calculated for the average temperatures from 30oC up to the maximum relative to the reference temperature at 22.5oC (Table 1). The risk of deaths statistically increased monotonically by the increase in the temperature for period 1; whereas this linear effect was not statistically significant observed for period 2 (all 95% CI of RRs included the unity) (Table 2). The relative risk ratios (RRR) were all less than one and gradually decreased from 0.86 (95% CI, 0.72–1.03) to 0.64 (95% CI, 0.33–1.22), however the RRRs were not statistically significant, reflecting the overlapped 95% CI presented in Fig. 3. The differences in attributable risk percent increased from 13.2 to 25.3% as shown in Table 2.
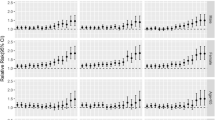
Figure 4 presents the main effects of heatwaves for two periods. The main effect of the heatwave was calculated as the risk ratio between the median temperatures during the heatwave duration and the 75th percentile of the temperature outside the heatwave durations. The heatwave defined at the 97th percentile did not cause significant health effects for almost all the groups (except males). Heatwaves defined at the 98th and 99th percentiles, reductions in the risk of heatwave-related deaths were observed for all groups except males from period 1 to period 2. The risks of death for the general population decreased by 3.4% (RRp1 1.068, 95% CI, 1.024–1.112 versus RRp2 1.034, 95% CI, 0.986–1.082) and 10% (RRp1 1.16, 95% CI, 1.10–1.22 versus RRp2 1.06, 95% CI, 1.002–1.119) for all groups of people. It is noteworthy that the risks declined from statistically significance (at the 98th percentile: RRp1 1.059, 95% CI, 1.0-1.12; at the 99th percentile: RRp1 1.13, 95% CI, 1.05–1.20) in the period 1 to non-significance in period 2 (at the 98th percentile: RRp2 0.95, 95% CI, 0.88–1.02; at the 99th percentile: RRp2 0.95, 95% CI, 0.86–1.23) among female groups, and this was also observed among elderly (75+) at the 99th threshold heatwave (RRp1 1.09, 95% CI, 1.02–1.16 versus RRp2 1.03, 95% CI, 0.96–1.10). The reductions were also observed in the people aged from 16- to 74-year-olds (at the 98th percentile: RRp1 1.18, 95% CI, 1.08–1.27 versus RRp2 1.15, 95% CI, 1.04–1.26; at the 99th percentile: RRp1 1.37, 95% CI, 1.24–1.49 versus RRp2 1.25, 95% CI, 1.11–1.39).
Sensitivity analysis
The adjusted cumulative temperature-mortality relationship and the differences in attributable risk percent for the selected arbitrary two study periods in the sensitivity analysis are shown in Supp. Figure 1, and Supp. Table 1, respectively. We compared these two arbitrary periods (1992–2005 and 2006–2019) which were unrelated to the actual HARS implementation periods. We did not find evidence of a decreasing risk of mortality following the implementation of the latter period. As shown in Supp. Figure 1, the slope of the risk of mortality curve rather increased in period 2 in comparison with period 1 during high temperatures, when compared to actual implementation periods. Similarly, the relative risk ratios (RRR) of heat-related deaths were all greater than 1 and sharply increased from 1.19 (95% CI, 0.76–1.88) to 2.07 (95% CI, (0.84–5.12), the RRRs were found to be statistically significant at 95% CI (Table 3). The Supp. Figure 2 and Supp. Tables 2–4, shows the sensitivity analysis of the effect of different lag structures (lag 4 days, lag 7 days, and lag 14 days) on cumulative temperature-mortality relationships in period 1 (1992–2009) and period 2 (2010–2019). We observed that the reduction in heat-associated death increases with increasing lag days following post-HARS activation (2010–2019).
Discussion
This study examined the association between extreme temperatures and mortality in Victoria, Australia in two periods (1992–2009 and 2010–2019). The heat-health alert and response system (HARS) were established and operated in 2009–2010. The results of the study provide the implication for the efficacy of the HARS since we compared the pattern and absolute effects of temperatures between two periods. These results are robust to sensitivity analysis as the risk of mortality curve did not increase in period 2 (arbitrary period 2006–2019) in comparison with period 1 (arbitrary period 1992–2005) during high temperatures, compared to actual implementation periods. Overall, we observed the reductions in risk of deaths associated with the extreme temperatures in period 2 compared with period (1) The reductions were higher corresponding to the higher threshold of the temperatures. In addition to the decrease in the heat-related risk of death, the effect of extreme cold in the summer period disappeared in period (2) However, despite the obvious reduction pattern in heat-related mortality, the risk ratios between the two periods were not statistically significant. We interpreted the risk ratios without accounting for statistical significance because we considered p-value alone as not an objective measure and did not provide enough information about hypothesis testing (Baghi et al. 2007; Hayat 2010). For example, similar studies have also concluded the effectiveness of heat action plans in reducing heat-related mortality without considering statistical significance (Díaz et al. 2019; Ebi et al. 2004).
The findings of this current study increase the evidence on the benefits of the heat-health action plan, which includes the HARS as a key component, in reducing heat-related mortalities across countries worldwide. A significant reduction in heat-related mortality was observed in the cities in Italy (Schifano et al. 2012), Montreal in Canada (Benmarhnia et al. 2016b), and Paris in France (De’Donato et al. 2015). Although there is no study comprehensively evaluating the efficacy of heat-health action plans and HARS in Australia, the previous studies looked at the public perception and responses toward heat health warnings in regional areas. The study by William et al. (2018) indicated that the heat-health warnings had been well received and understood, however the behavior change was varied by regional populations in Australia. Thus, this study encourages reinforcing existing protective behavior rather than promoting change (Williams et al. 2019). The findings also found that women had higher perceptions of a heat-related health risks than men. This is an interesting point and well reflected by the significant reduction of heat-related mortality among women observed in our study in comparison with other groups, although it may reflect the propensity of cardiovascular diseases in males in this population. It may also reflect the sexual dimorphism in ratio of occupations involving outdoor work (Fatima et al. 2021). Another study by the Williams et al. (2021) estimated that the potential cost savings from reduced morbidity offset the estimated heat-health warnings implementation costs by at least two-fold (Williams et al. 2021). Both studies encouraged the effectiveness of the systems should be further evaluated.
For example, evaluating HARS according to pre- and post-implementation in the case of this study may capture confounding factors that are likely to change over time such as increasing cognizance of heat-health education, air conditioning prevalence rate, and modern housing systems. In addition, behavioral change toward adaptations (e.g., taking annual leave during the summer season), and an inherent decrease in heat sensitivity because of acclimatization may not be linked with HARS implementation(Weinberger et al. 2021; Boeckmann and Rohn 2014). On the other hand, an increase in migration may increase the risk of heat-related outcomes as new migrants may lack acclimatization or have limited knowledge of accessing emergency healthcare services during extreme heat events(Hansen et al. 2014). Also, improvement in socioeconomic conditions may be predictors that can decrease the risk of heat-related deaths(Ng et al. 2016). Evidence shows that Victoria has shown an improvement in the unemployment rate (5%), and increased number of home ownership (36.1%) in 2021 compared to 2006 where they were 5.4%, and 34%, respectively (Australian Bureau of Statistics 2006, 2021b). Having recognized these potential confounding factors, we can then understand the true effectiveness of HARS in Victoria by comparing days of activation of the heat alerts versus days without heat alerts (Weinberger et al. 2021).
In terms of other potential mechanisms of the heat-health action plan for reducing heat-related health risks, the evidence from the previous studies suggests that the plans could reduce risks through surveillance and monitoring of effects (Elliot et al. 2014; Perry et al. 2011; Josseran et al. 2009), mobilizing of community resources (Hasan et al. 2021). The influence of the plans may change over time and vary by location, thus they should be developed to meet the local needs and based on the latest evidence of health risks as well as the effectively existing preventive measures which could be readily implemented by the local public health officials and community (Jay et al. 2021). Our study provides updated evidence on the temperature threshold as well as the temporal changes in mortality in relation to the operation of the heat-health action plan and alert system at the State level of the Victoria suggests positive benefits from use of the action plan. We found important evidence on the efficacy of the heat-health alert system in reducing heat-related mortality among women and vulnerable groups such older people. Our sensitivity analysis confirms that heat-associated death reduces few weeks after the activation of the heat-health action plan and alert system. This suggest that the implementation period effectively reduces risk of death and could be helpful in future risk communication.
The lower threshold temperature observed in this study warrants further research to determine the updated optimum temperature thresholds used for the specific locations in the alert system. Similar to previous studies, this current study encounters the limitation in evaluating whether the reduction in heat-related mortality is due to the heat-health alert system itself or a growing understanding of the risk of high heat exposure in the community and the implementation of mitigation factors in the community. These may include factors such as improved housing conditions (air conditioning, design), and increasing greenspaces in better designed newer suburban areas.
This study has some limitations. First, our study used the average temperature registered from a single monitoring station in the central area, so the exposure of temperature might be misclassified in rural areas that are far from the central area. However, the proportion of the rural populations is small (approximately 12%), thus the potential bias in overall estimates is expected to be small. Second, we were unable to obtain the mortality data by districts and regions but aggregated data for the whole of Victoria, so the evaluation was not conducted against the temperature thresholds which vary by the region. There are significant differences in average daily temperature with increases seen in areas more continental areas, away from the coast. Alternatively, we examined the temporal change of mortality in relation to the temperature before and after the implementation of the heat-health alert system at the state level. A future study should examine the effectiveness of the heat-health alert system at a higher resolution level since the heat-health alerts are issued for specific local governments once the temperature thresholds of the relevant districts have exceeded the threshold. Third, the design of our study does not allow us to assess the causality because we did not have a control group and data on heat-health adaptation in the household- and individual-level (e.g., increase in the prevalence of mitigation factors such as air conditioning over time). A more sophisticated study design, such as difference-in-difference, can address the effect of underlying time-dependent trends in the health outcomes unrelated to the heat-health intervention. The populations overall understanding of the risk of heat as part of a changing environment has also changed during this time and the contribution of this (as opposed to the HHWS alone) is unclear.
Conclusion
The study indicated a decrease in mortality attributed to high ambient temperatures and heatwaves after the operation of the heat-health alert and response system (HARS) in Victoria. The decrease was observed more with high intensity of heatwaves. The temperature thresholds are likely to change over time, so further studies should be conducted to investigate this change to adapt the heat-health alert system and enhance the public health actions in reducing the heat-related health risk in a timely fashion.
References
Australian Bureau of Statistics (2021b) Victoria 2021 Census All persons QuickStats. Australian Bureau of Statistics. https://www.abs.gov.au/census/find-census-data/quickstats/2021/2. Accessed 05/01/2024
Australian Bureau of Statistics (2021a) Population: Census. Australian Bureau of Statistics. https://www.abs.gov.au/statistics/people/population/population-census/2021. Accessed 24/08/2022
Australian Bureau of statistics (2019) Data by region. https://dbr.abs.gov.au/. Accessed 06/02/2019
Australian Bureau of Statistics (2006) Victoria 2006 Census All persons QuickStats. Australian Bureau of Statistics. https://abs.gov.au/census/find-census-data/quickstats/2006/2#:~:text=In%20the%202006%20Census%20in,median%20household%20income%20was%20%241%2C022. Accessed 05/01/2024
Baghi H, Noorbaloochi S, Moore JB (2007) Statistical and nonstatistical significance: implications for Health Care Researchers. Qual Manage Healthc 16 (2)
Beck HE, Zimmermann NE, McVicar TR, Vergopolan N, Berg A, Wood EF (2018) Present and future Köppen-Geiger climate classification maps at 1-km resolution. Sci Data 5(1):180214. https://doi.org/10.1038/sdata.2018.214
Beggs PJ, Zhang Y, McGushin A, Trueck S, Linnenluecke MK, Bambrick H, Berry HL, Jay O, Rychetnik L, Hanigan IC (2021) The 2021 report of the MJA–Lancet countdown on health and climate change: Australia increasingly out on a limb. Med J Aust 215(9):390–392 e322
Benmarhnia T, Bailey Z, Kaiser D, Auger N, King N, Kaufman Jay S (2016a) A difference-in-differences Approach to assess the Effect of a Heat Action Plan on Heat-related mortality, and differences in effectiveness according to sex, Age, and socioeconomic status (Montreal, Quebec). Environ Health Perspect 124(11):1694–1699. https://doi.org/10.1289/EHP203
Benmarhnia T, Bailey Z, Kaiser D, Auger N, King N, Kaufman JS (2016b) A difference-in-differences approach to assess the effect of a heat action plan on heat-related mortality, and differences in effectiveness according to sex, age, and socioeconomic status (Montreal, Quebec). Environ Health Perspect 124(11):1694–1699
Bi P, Williams S, Loughnan M, Lloyd G, Hansen A, Kjellstrom T, Dear K, Saniotis A (2011) The effects of extreme heat on human mortality and morbidity in Australia: implications for public health. Asia Pac J Public Health 23(2suppl):27S–36S
Bobb Jennifer F, Peng Roger D, Bell Michelle L, Dominici F (2014) Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect 122(8):811–816. https://doi.org/10.1289/ehp.1307392
Boeckmann M, Rohn I (2014) Is planned adaptation to heat reducing heat-related mortality and illness? A systematic review. BMC Public Health 14(1):1112. https://doi.org/10.1186/1471-2458-14-1112
Campbell SL, Remenyi T, Williamson GJ, Rollins D, White CJ, Johnston FH (2021) Ambulance dispatches and heatwaves in Tasmania, Australia: a case-crossover analysis. Environ Res 202:111655. https://doi.org/10.1016/j.envres.2021.111655
Chapman S, Watson JE, Salazar A, Thatcher M, McAlpine CA (2017) The impact of urbanization and climate change on urban temperatures: a systematic review. Landscape Ecol 32(10):1921–1935
Cheng J, Xu Z, Bambrick H, Su H, Tong S, Hu W (2018) Heatwave and elderly mortality: an evaluation of death burden and health costs considering short-term mortality displacement. Environ Int 115:334–342. https://doi.org/10.1016/j.envint.2018.03.041
Coates L, Haynes K, O’Brien J, McAneney J, de Oliveira FD (2014) Exploring 167 years of vulnerability: an examination of extreme heat events in Australia 1844–2010. Environ Sci Policy 42:33–44. https://doi.org/10.1016/j.envsci.2014.05.003
Coates L, van Leeuwen J, Browning S, Gissing A, Bratchell J, Avci A (2022) Heatwave fatalities in Australia, 2001–2018: an analysis of coronial records. Int J Disaster Risk Reduct 67:102671. https://doi.org/10.1016/j.ijdrr.2021.102671
Davis RE, Roney PC, Pane MM, Johnson MC, Leigh HV, Basener W, Curran AL, DeMarcy B, Jang J, Schroeder C, DeGuzman PB, Novicoff WM (2023) Climate and human mortality in Virginia, 2005–2020. Sci Total Environ 894:164825. https://doi.org/10.1016/j.scitotenv.2023.164825
De’Donato FK, Leone M, Scortichini M, De Sario M, Katsouyanni K, Lanki T, Basagaña X, Ballester F, Åström C, Paldy A (2015) Changes in the effect of heat on mortality in the last 20 years in nine European cities. Results from the PHASE project. Int J Environ Res Public Health 12(12):15567–15583
Díaz J, Sáez M, Carmona R, Mirón IJ, Barceló MA, Luna MY, Linares C (2019) Mortality attributable to high temperatures over the 2021–2050 and 2051–2100 time horizons in Spain: adaptation and economic estimate. Environ Res 172:475–485. https://doi.org/10.1016/j.envres.2019.02.041
Ebi KL, Teisberg TJ, Kalkstein LS, Robinson L, Weiher RF (2004) Heat Watch/Warning systems Save lives: estimated costs and benefits for Philadelphia 1995–98. Bull Am Meteorol Soc 85(8):1067–1074. https://doi.org/10.1175/BAMS-85-8-1067
Ebi KL, Capon A, Berry P, Broderick C, de Dear R, Havenith G, Honda Y, Kovats RS, Ma W, Malik A, Morris NB, Nybo L, Seneviratne SI, Vanos J, Jay O (2021) Hot weather and heat extremes: health risks. Lancet 398(10301):698–708. https://doi.org/10.1016/S0140-6736(21)01208-3
Elliot AJ, Bone A, Morbey R, Hughes HE, Harcourt S, Smith S, Loveridge P, Green HK, Pebody R, Andrews N (2014) Using real-time syndromic surveillance to assess the health impact of the 2013 heatwave in England. Environ Res 135:31–36
Extreme Heat Sub-plan for Victoria (2017) State Emergency Response Plan Extreme Heat Sub-plan Edition 2. Victorian Government, Victoria, Australia
Fatima SH, Rothmore P, Giles LC, Varghese BM, Bi P (2021) Extreme heat and occupational injuries in different climate zones: a systematic review and meta-analysis of epidemiological evidence. Environ Int 148:106384. https://doi.org/10.1016/j.envint.2021.106384
Franklin RC, Mason HM, King JC, Peden AE, Nairn J, Miller L, Watt K, FitzGerald G (2023) Heatwaves and mortality in Queensland 2010–2019: implications for a homogenous state-wide approach. Int J Biometeorol 67(3):503–515. https://doi.org/10.1007/s00484-023-02430-6
Gasparrini A (2014) Modeling exposure–lag–response associations with distributed lag non-linear models. Stat Med 33(5):881–899
Gasparrini A, Armstrong B (2011) The impact of heat waves on mortality. Epidemiol (Cambridge Mass) 22(1):68
Gasparrini A, Guo Y, Hashizume M, Kinney PL, Petkova EP, Lavigne E, Zanobetti A, Schwartz JD, Tobias A, Leone M (2015) Temporal variation in heat–mortality associations: a multicountry study. Environ Health Perspect 123(11):1200–1207
Guo Y, Gasparrini A, Armstrong BG, Tawatsupa B, Tobias A, Lavigne E, Coelho MSZS, Pan X, Kim H, Hashizume M (2017) Heat wave and mortality: a multicountry, multicommunity study. Environ Health Perspect 125(8):087006
Hansen A, Bi P, Nitschke M, Ryan P, Pisaniello D, Tucker G (2008) The Effect of Heat Waves on Mental Health in a temperate Australian City. Environ Health Perspect 116(10):1369–1375. https://doi.org/10.1289/ehp.11339
Hansen A, Nitschke M, Saniotis A, Benson J, Tan Y, Smyth V, Wilson L, Han G-S, Mwanri L, Bi P (2014) Extreme heat and cultural and linguistic minorities in Australia: perceptions of stakeholders. BMC Public Health 14(1):550. https://doi.org/10.1186/1471-2458-14-550
Hasan F, Marsia S, Patel K, Agrawal P, Razzak JA (2021) Effective Community-based interventions for the Prevention and Management of Heat-related illnesses: a scoping review. Int J Environ Res Public Health 18(16). https://doi.org/10.3390/ijerph18168362
Hayat MJ (2010) Understanding statistical significance. Nurs Res 59 (3)
Jay O, Capon A, Berry P, Broderick C, de Dear R, Havenith G, Honda Y, Kovats RS, Ma W, Malik A (2021) Reducing the health effects of hot weather and heat extremes: from personal cooling strategies to green cities. Lancet 398(10301):709–724
Josseran L, Caillère N, Brun-Ney D, Rottner J, Filleul L, Brucker G, Astagneau P (2009) Syndromic surveillance and heat wave morbidity: a pilot study based on emergency departments in France. BMC Med Inf Decis Mak 9(1):1–9
Kotharkar R, Ghosh A (2022) Progress in extreme heat management and warning systems: a systematic review of heat-health action plans (1995–2020). Sustainable Cities Soc 76:103487
Lemonsu A, Viguié V, Daniel M, Masson V (2015) Vulnerability to heat waves: impact of urban expansion scenarios on urban heat island and heat stress in Paris (France). Urban Clim 14:586–605 doi org/101016/j ucli m 10
Lo YTE, Mitchell DM, Thompson R, O’Connell E, Gasparrini A (2022) Estimating heat-related mortality in near real time for national heatwave plans. Environ Res Lett 17(2):024017. https://doi.org/10.1088/1748-9326/ac4cf4
Loughnan M, Nicholls N, Tapper N (2010a) Mortality–temperature thresholds for ten major population centres in rural Victoria, Australia. Health Place 16(6):1287–1290. https://doi.org/10.1016/j.healthplace.2010.08.008
Loughnan ME, Nicholls N, Tapper NJ (2010b) When the heat is on: threshold temperatures for AMI admissions to hospital in Melbourne Australia. Appl Geogr 30(1):63–69
Martinez GS, Kendrovski V, Salazar MA, de’Donato F, Boeckmann M (2022) Heat-health action planning in the WHO European Region: Status and policy implications. Environ Res 214:113709. https://doi.org/10.1016/j.envres.2022.113709
Martínez-Solanas È, Basagaña X (2019) Temporal changes in temperature-related mortality in Spain and effect of the implementation of a Heat Health Prevention Plan. Environ Res 169:102–113
Ng CFS, Boeckmann M, Ueda K, Zeeb H, Nitta H, Watanabe C, Honda Y (2016) Heat-related mortality: effect modification and adaptation in Japan from 1972 to 2010. Glob Environ Change 39:234–243. https://doi.org/10.1016/j.gloenvcha.2016.05.006
Ngandu T, Lehtisalo J, Solomon A, Levälahti E, Ahtiluoto S, Antikainen R, Bäckman L, Hänninen T, Jula A, Laatikainen T (2015) A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet 385(9984):2255–2263
Perry AG, Korenberg MJ, Hall GG, Moore KM (2011) Modeling and syndromic surveillance for estimating weather-induced heat-related illness. Journal of environmental and public health 2011
Pezza AB, Van Rensch P, Cai W (2012) Severe heat waves in Southern Australia: synoptic climatology and large scale connections. Clim Dyn 38(1):209–224
Schifano P, Leone M, De Sario M, de’Donato F, Bargagli AM, D’Ippoliti D, Marino C, Michelozzi P (2012) Changes in the effects of heat on mortality among the elderly from 1998–2010: results from a multicenter time series study in Italy. Environ Health 11(1):1–9
Tong S, FitzGerald G, Wang X-Y, Aitken P, Tippett V, Chen D, Wang X, Guo Y (2015) Exploration of the health risk-based definition for heatwave: a multi-city study. Environ Res 142:696–702. https://doi.org/10.1016/j.envres.2015.09.009
Victoria Government (2020) Heat health plane for Victoria
Watson KE, Gardiner KM, Singleton JA (2020) The impact of extreme heat events on hospital admissions to the Royal Hobart Hospital. J Public Health 42(2):333–339
Weinberger KR, Wu X, Sun S, Spangler KR, Nori-Sarma A, Schwartz J, Requia W, Sabath BM, Braun D, Zanobetti A, Dominici F, Wellenius GA (2021) Heat warnings, mortality, and hospital admissions among older adults in the United States. Environ Int 157:106834. https://doi.org/10.1016/j.envint.2021.106834
Williams S, Hanson-Easey S, Nitschke M, Howell S, Nairn J, Beattie C, Wynwood G, Bi P (2019) Heat-health warnings in regional Australia: examining public perceptions and responses. Environ Hazards 18(4):287–310
Williams S, Nitschke M, Wondmagegn BY, Tong M, Xiang J, Hansen A, Nairn J, Karnon J, Bi P (2021) Evaluating cost benefits from a heat health warning system in Adelaide, South Australia. Australian and New Zealand Journal of Public Health
Wondmagegn BY, Xiang J, Dear K, Williams S, Hansen A, Pisaniello D, Nitschke M, Nairn J, Scalley B, Varghese BM, Xiao A, Jian L, Tong M, Bambrick H, Karnon J, Bi P (2021) Impact of heatwave intensity using excess heat factor on emergency department presentations and related healthcare costs in Adelaide, South Australia. Sci Total Environ 781:146815. https://doi.org/10.1016/j.scitotenv.2021.146815
Zhang Y, Beggs PJ, McGushin A, Bambrick H, Trueck S, Hanigan IC, Morgan GG, Berry HL, Linnenluecke MK, Johnston FH (2020) The 2020 special report of the MJA–Lancet countdown on health and climate change: lessons learnt from Australia’s Black Summer. Med J Aust 213(11):490–492 e410
Zhao Q, Guo Y, Ye T, Gasparrini A, Tong S, Overcenco A, Urban A, Schneider A, Entezari A, Vicedo-Cabrera AM, Zanobetti A, Analitis A, Zeka A, Tobias A, Nunes B, Alahmad B, Armstrong B, Forsberg B, Pan S-C, Íñiguez C, Ameling C, De la Cruz Valencia C, Åström C, Houthuijs D, Dung DV, Royé D, Indermitte E, Lavigne E, Mayvaneh F, Acquaotta F, de’Donato F, Di Ruscio F, Sera F, Carrasco-Escobar G, Kan H, Orru H, Kim H, Holobaca I-H, Kyselý J, Madureira J, Schwartz J, Jaakkola JJK, Katsouyanni K, Hurtado Diaz M, Ragettli MS, Hashizume M, Pascal M, de Sousa Zanotti Stagliorio Coélho M, Valdés Ortega N, Ryti N, Scovronick N, Michelozzi P, Matus Correa P, Goodman P, Nascimento Saldiva PH, Abrutzky R, Osorio S, Rao S, Fratianni S, Dang TN, Colistro V, Huber V, Lee W, Seposo X, Honda Y, Guo YL, Bell ML, Li S (2021) Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet Health 5(7):e415–e425. https://doi.org/10.1016/S2542-5196(21)00081-4
Acknowledgements
A/Prof Osborne and Dr Phung are investigators on the NHMRC grant “Healthy Environments and Lives (HEAL) - National Research Network on Human Health and Environmental Change”. Patrick Amoatey is the recipient of a UQ international HDR scholarship.
Funding
No funding was received for conducting this study.
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Not Applicable.
Conflict of interest
The authors declare no known competing conflict of interest that might influence the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Osborne, N.J., Amoatey, P., Selvey, L. et al. Temporal changes in temperature-related mortality in relation to the establishment of the heat-health alert system in Victoria, Australia. Int J Biometeorol (2024). https://doi.org/10.1007/s00484-024-02691-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00484-024-02691-9