Abstract
This review examines high-quality research evidence that synthesises the effects of extreme heat on human health in tropical Africa. Web of Science (WoS) was used to identify research articles on the effects extreme heat, humidity, Wet-bulb Globe Temperature (WBGT), apparent temperature, wind, Heat Index, Humidex, Universal Thermal Climate Index (UTCI), heatwave, high temperature and hot climate on human health, human comfort, heat stress, heat rashes, and heat-related morbidity and mortality. A total of 5, 735 articles were initially identified, which were reduced to 100 based on a set of inclusion and exclusion criteria. The review discovered that temperatures up to 60°C have been recorded in the region and that extreme heat has many adverse effects on human health, such as worsening mental health in low-income adults, increasing the likelihood of miscarriage, and adverse effects on well-being and safety, psychological behaviour, efficiency, and social comfort of outdoor workers who spend long hours performing manual labour. Extreme heat raises the risk of death from heat-related disease, necessitating preventative measures such as adaptation methods to mitigate the adverse effects on vulnerable populations during hot weather. This study highlights the social inequalities in heat exposure and adverse health outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most studies on heat-human health have focused on high income countries (HICs) compared to low- and middle-income countries (LMICs), for which few studies have been conducted, particularly in tropical Africa (Basu 2009; Green et al. 2019; Ebi et al. 2021; Kotharkar and Ghosh 2022). High temperatures can cause a rise in core body temperature and heart rate and lead to heat stress, heat stroke and, in extreme cases, death. Individuals with heart disease, obesity, or respiratory conditions are more vulnerable to heat stress (Donaldson et al. 2003; Kenney et al. 2014; Rahman and Adnan 2023). Among the effects of high temperatures on human health are heat exhaustion, dehydration, respiratory issues, cardiovascular strain, skin diseases, mental health issues, and electrolyte imbalance (Basu and Samet 2002; Gosling et al. 2009; Hajat and Kosatky 2010; Gabriel and Endlicher 2011; Hondula et al. 2012; Ma et al. 2014; Alcoforado et al. 2015; Son et al. 2016; Mora et al. 2017). High temperatures not only exacerbate existing heat-related health conditions, leading to organ failure and mortality, but also cause a range of harmful effects such as an increase in violent crimes (Sanz-Barbero et al. 2018), fatal road accidents (Wu et al. 2018), and stress on ambulance services (Dolney and Sheridan 2006; Cheng et al. 2016; Guo 2017). Rising temperatures also increase electricity and water demand (Hatvani-Kovacs et al. 2016), impacting infrastructure, water quality, open spaces, and overall liveability in urban areas (Klok and Kluck 2018).
The effects of heat on human health are further exacerbated by environmental, socioeconomic, demographic, physiological and behavioural factors. For instance, urban areas with high population density, limited green space, and extensive artificial impervious surfaces (AIS) can be warmer than surrounding areas (Myint et al. 2013; Chen et al. 2022a, b; Rajagopal et al. 2023). Economic constraints can limit access to cooling systems, adequate hydration, and healthcare services, e.g. inadequate access to air conditioning and other cooling methods can increase human vulnerability during extreme heat. Living in poorly ventilated homes can exacerbate the harmful effects of extreme heat (Thomson et al. 2019). Limited access to healthcare can hinder the treatment of heat-related illnesses; the effectiveness of public health interventions and heatwave warning systems plays a crucial role in exacerbating the harmful effects of extreme heat (Foster et al. 2020; Périard et al. 2021; Hess et al. 2023). Outdoor workers, such as those in construction, mining, and agriculture, are more exposed to high temperatures (Jay et al. 2021; He et al. 2023). Isolated individuals may lack assistance during heat waves (Kenny et al. 2020; Habibi et al. 2023). Older populations and young children are more sensitive to heat due to less effective thermoregulation (Tsuzuki 2023). A lack of awareness of heat risks can lead to inadequate preventive measures (Jessel et al. 2019). Cultural norms and practices, for instance, clothing choices, might affect how individuals respond to heat (Sovacool et al. 2021).
The occurrence of hot days in tropical Africa has been increasing since the 1980s because of increasing greenhouse gas (GHG) emissions, which continue to alter the region's summer temperatures (Mahlstein et al. 2011; Harrington et al. 2017; Herold et al. 2017; Ntoumos et al. 2022). Temperatures in tropical Africa are frequently near the upper limit of human comfort (Sherwood and Huber 2010). For example, in 2010, extreme temperature incidents of 47.6 °C and 48.2 °C were recorded in Faya-Largeau, Chad Republic, and Bilma, Niger Republic, respectively (World Meteorological Organization 2016). Furthermore, between 1989 and 2009, tropical Africa recorded 40 to 50 heat waves annually (Cook and Vizy 2012; Iyakaremye et al. 2021). The Nigerian Meteorological Agency (2021) recently reported extreme heatwave events of 50 °C in the Northern-eastern region of Nigeria. The Emergency event database (EM-DAT 2023) reports an incident with an extreme temperature of 60 °C in Nigeria which killed 60 people. (Table 1).
The effects of extreme heat on human health in LMICs are often exacerbated by socioeconomic and demographic characteristics of the population, for example, poverty, literacy, infants, and aged population (Oluwafemi et al. 2023; Nyadanu et al. 2023). The IPCC (2022) reported that LMICs had limited adaptive capacity to extreme heat due to scarce resources, fragile political institutions, and socio-cultural practices. More research on heat-human health in tropical Africa is needed (Omonijo et al. 2013; Agan 2017; Leal Filho et al. 2018; Niu et al. 2021) to identify the requirement for enhancing the resilience of the region to climate change-enhanced extreme heat events. Recent studies indicate that some HICs have observed a decline in the sensitivity of health outcomes to extreme heat, which implies an increase in adaptive capacity to extreme heat (Coates et al. 2014; Bobb et al. 2014; Sheridan and Allen 2018; Laranjeira et al. 2021). Unlike HICs, vulnerability to extreme heat in LMICs is on the rise due to their increase in sensitivity and low adaptive capacity to extreme heat (Hajat et al. 2010; Azhar et al. 2017; Green et al. 2019; Ncongwane et al. 2021; Chen et al. 2022a, b). This review aims to summarise the peer-reviewed literature on the relationship between extreme heat and human health in tropical Africa.
Material and methods
The regional focus of the review
Tropical regions lie between latitudes 23.5° north and south of the equator. Tropical Africa consists of 48 countries that make up five sub-regions: West Africa (16 countries), East Africa (9), Central Africa (10), part of Southern Africa (7), the Indian Ocean islands, and Madagascar (6). Figure 1 presents the sub-regions and member countries of tropical Africa. The Köppen-Geiger system classified the climate of tropical Africa as Type ‘A,’ characterised by constant, elevated temperatures and generally humid (Af) with high amounts of precipitation because of their closeness to the equator (Burkart et al. 2014). However, there is the emergence of drier climatic areas with declining rainfall towards latitude 23.5° north and south away from the equator due to the influence of the subtropical high-pressure system (Aw) and transition from type ‘A’ to type ‘B’ arid climates. Generally, regions at high altitudes have lower temperatures, typical of warm temperate-type ‘C’ climates (Kottek et al. 2006).
The weather and climate of tropical Africa varies with geographical location and is influenced by topography, proximity to large water bodies and movements of the Intertropical Convergence Zone (ITCZ; Odekunle et al. 2005; Oluwafemi et al. 2023). There are two major seasons in tropical Africa: rainy and dry seasons. The rainy season in Central and West Africa, e.g. Nigeria and Congo, start from April to October, with annual rainfall of 1,000—2,500 mm. The dry season lasts from November to March (Adeniyi and Oyekola 2017; Odekunle et al. 2005; Adegebo 2022). East Africa, e.g., Kenya and Ethiopia, is characterised by two rainy seasons—the long rainy season from March to May and the short rainy season from October to December, with an average rainfall of 500—1,500 mm. The dry season in this region occurs between the two rainy seasons and after the short rains (Camberlin and Philippon 2002; Cattani et al. 2018). Generally, the dry season is characterised by lower humidity, less cloud cover, and little or no rainfall. Tropical Africa generally experiences a warm climate, with temperatures ranging from 25°C to 30°C (Odekunle et al. 2005). However, there are temperature variations; for instance, highlands, e.g., Ethiopian highlands, have lower temperatures, below 20°C (Camberlin and Philippon 2002). Coastal regions have more consistent temperatures, influenced by oceanic currents, with an average monthly temperature of 31◦C and 32◦C in February and March and reaching their lowest temperature of 27◦C to 28◦C in July and August (Oluwafemi et al. 2023). The Sahelian Region at the northern fringes can experience more extreme temperatures over 40°C in March and April due to its proximity to the Sahara Desert (Agada and Yakubu 2022).
Search approach
Literature searches were performed in the Web of Science (WoS) to identify research articles on the association between extreme heat and human health in tropical Africa. The search terms were narrowed to peer-reviewed articles written in English. 5,735 publications were initially identified. Searches included all publications in the WoS database up to and including December 2023. Table 2 shows the keywords and search terms that were used to search “All fields” in the WoS database, which included health outcomes that are commonly referred to in heat health studies (e.g. human health, heat-related mortality) and several climatic and biometeorological climate variables that broadly cover the totality of the effect of weather and climate associated with extreme heat on temperature-related health by accounting for temperature, humidity, wind speed and radiation (e.g. high temperature, Wet Bulb Globe Temperature (WBGT), Universal Thermal Climate Index (UTCI); see Gosling et al. (2014) for definitions).
A preliminary scan of the articles identified after conducting the searches listed in Table 2 was undertaken to eliminate studies that examine non-human impacts, such as those on plants and animals. A manual check on the articles' titles, abstracts, and main text was undertaken for further screening using the inclusion criteria below:
-
1.
Studies carried out in any part of a country located between the tropics in tropical Africa, which focused on the effects on human health from increasing temperature, extreme heat, or heatwaves, and considered humidity, wind speed, solar radiation, or hot climate.
-
2.
Studies carried out in any part of a country located between the tropics in tropical Africa, which have considered the effects of heat as modifiers of deaths/infections from malaria, Trypanosomiasis, Schistosomiasis, and other infectious diseases.
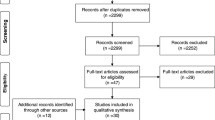
After removing duplicate entries and articles due to study area location and the 2 inclusion criteria, 100 articles met the requirement for this review as shown in Fig. 2.
Studies identified by the review
The number of studies on the effects of heat on human health, organised by country in tropical Africa, is shown in Table 3. Many studies have been conducted in Nigeria, Ghana, Kenya, Tanzania and Burkina Faso, Gambia, and South Africa. Only one or two studies have been published for many countries. There were no studies done in the following 17 tropical African countries: Niger, Chad, Mauritania, Ethiopia, Somalia, Eritrea, Togo, Ivory Coast, Liberia, Sierra Leone, Guinea Bissau, CAR, Zaire, Tanzania, Angola, Namibia, and Batswana. There have also been no studies conducted in African Countries that are partially in the tropics, such as Algeria (Tamanrasset Province), Egypt (Aswan Governorate), Libya (Al Kufra), and Western Sahara. 9(9%) studies are multi-country, encompassing a wide range of environments, socioeconomic and populations, 5(5%) of which were conducted in West Africa and 1(1%) in Central Africa. 1(1%) study was conducted in Kenya, Zambia, and Zimbabwe; Guinea, Gabon, the Democratic Republic of the Congo, South Sudan, and Uganda; and Kenya, Uganda, Rwanda, Burundi, Tanzania, Zambia, Malawi, and Mozambique. A multi-country study offers a more reliable understanding of tropical Africa's complex interactions between heat and human health.
The temporal resolution of studies and the length of time that they explored health impacts
The temporal resolution of the studies relates to whether the data was collected daily, weekly, monthly, seasonal, annually, and future projections. The length of the study relates to how long the studies investigate health impacts, i.e., how many days or years of data were used for the study.
Concerning the temporal resolution of the data, 15 (15%) of the studies project the future effects of heat on human health (Lorena et al. 2018; Ragatoa et al. 2018; Fotso-Nguemo et al. 2022). 25 (25%) studies used hourly, daily, monthly, and seasonal datasets, e.g. Azongo et al (2012) and Faye et al (2021) studied heat exposure on a daily scale. Brewster and Greenwood (1993) and Frimpong et al (2014) explored seasonal scale variations. 43 (43%) of the studies are based on annual and multi-annual scales. These were heat-health studies lasting years or decades. For example, studies by Etard et al (2004) and Fotso-Nguemo et al (2022) cover 11 and 39 years, respectively.
It may be argued that studies founded on annual and multi-annual scales, as opposed to daily, weekly, monthly, or seasonal studies offer a better extrapolation of the association between extreme heat and human health because it enables a more accurate assessment of the effects and changes over time. This depends on whether the study is a clinical trial assessing the immediate effects of excessive heat over a relatively short period or a cohort study exploring the long-term health effects of extreme heat to monitor the change over time. For instance, case-crossover studies are a type of observational research design commonly used in epidemiology and public health to investigate the association between an exposure such as heat exposure and an outcome such as a health outcome, these studies are beneficial for studying the acute effects of transient exposures on short-term outcomes.
Methods and technologies for data collection and analysis
Systematic data collection from weather stations is often used (Olatunde 2016; Azongo et al. 2012; Luque Fernández et al. 2009) while other studies use data from remote sensing, for example Wiru et al (2020), Mutai (2013), and Paz (2009) used satellite data from the National Climate Data Centre of the National Oceanic and Atmospheric Administration. Herold et al (2017). Balogun and Balogun (2014), Kwasi et al (2014), and Balogun and Daramola (2019) used a Shielded portable Lascar EL-USB-2 data logger for collecting observed temperature and relative humidity data. Some experiments utilised technological data observations concerning the data type, such as temperature and relative humidity, from a weather station or a Shielded portable Lascar EL-USB-2 data recorder (Adeniyi 2009; Frimpong et al. 2016; Balogun and Daramola 2019). Due to their cost, portability, and convenience, the use of Lascar USB temperature and humidity sensors with a calibrated Questemp heat stress monitor for daily, monthly of seasonal studies has increased in recent years (Balogun and Balogun 2014; Kwasi et al. 2014; Frimpong et al. 2016). Other research methods include questionnaires, surveys, and FGD (Ngwenya et al. 2018; Frimpong et al. 2020; Nunfam 2021). Nevertheless, some studies rely on hospital health data (Etard et al. 2004; Diboulo et al. 2012; Wiru et al. 2020).
13 (13%) of the articles cited in this review utilised reanalysis and climate models to simulate past, present, and future heat-human health relationships. 5 (5%) of studies explored future projections of heat stress, high temperature, relative humidity, heatwaves, and extreme heat on human health (Ermert et al. 2012; Sylla et al. 2018; Sarr et al. 2019; Gyilbag et al. 2021; Ragatoa et al. 2018). Reanalysis and climate models provide spatially gridded, historical and future climatic data, essential for studying long-term trends and potential future scenarios of heat impacts on human health across large spatial domains, aiding public health planning and climate change adaptation strategies. The output from these models often contains uncertainties due to assumptions and limitations in data and might not accurately capture local variations, leading to less precise assessments at local scales. 6 (6%) of the cited studies are at the regional scale, e.g. (Blom et al. 2022, Adeniyi and Oyekola 2017, Sylla et al. 2018, Batté et al. 2018; Ermert et al. 2012) covered West Africa, whereas Fotso-Nguemo et al. (2022) covered central Africa.
Several studies have used high resolution regional climate model simulations to estimate the effects of different greenhouse gas emissions scenarios on future health in tropical Africa. Some studies have used climate projections from the recent Coordinated Regional Climate Downscaling Experiment (CORDEX) program (Sarr et al. (2019), Ragatoa et al. (2018), Sylla et al. (2018), Gyilbag et al. 2021) and Adeniyi and Oyekola (2017)), for either Representative Concentration Pathway (RCP) greenhouse gas scenarios or global warming scenarios. Other studies have used the COSMO-CLM regional climate model, e.g. Ermert et al. (2012) and Fotso-Nguemo et al. (2022) considered a 1.5 °C global warming scenario. Diouf et al. (2013) used two, older, SRES emissions scenarios. No studies to date have considered the latest SSP (Shared Socioeconomic Pathways) scenarios and/or simulations from CMIP6 climate models (Coupled Model Intercomparison Project).
Over 47 (47%) of the identified studies employed descriptive and inferential statistics to analyse daily, monthly, and seasonal data from field surveys, FGD, questionnaires, and interviews (Alaigba et al. 2018; Ngwenya et al. 2018; Nunfam 2021). Annual and multi-annual studies such as 30 years, frequently employ time series, regression, and correlation designs to directly compare health data with biometeorological factors (Scott et al. 2017; Asamoah et al. 2018; Wiru et al. 2020).
Summary of the review findings
Table (Online resources 1) summarises studies on the effects of extreme heat on human health in tropical Africa. Even though most studies identified showed an increase in morbidity and mortality in the hot/rainy season compared to the cool season (e.g., Kynast-Wolf et al. 2006; Mutisya et al. 2010; Diboulo et al. 2012; Scott et al. 2017), studies in Bono village of Ghana revealed an increased risk of death at the lowest Apparent Temperature (18°C). Specifically, the highest relative mortality risk (RR = 1.61, 95% CI: 1.21–2.15, p-value < 0.001) was observed three days after exposure to an apparent temperature of 18 °C, indicating a substantial increase in the risk of death compared to other apparent temperatures studied such as the first quartile (23 °C), third quartile (26 °C), and the highest apparent temperature (31 °C) that showed no significant relationship with mortality (Wiru et al 2020). In Botswana, Alexander et al (2013) found that minimum temperatures were related to increase Diarrhea occurrence. A study by Rayco-solon et al (2004) revealed seasonality in death rates, with more deaths occurring during the "hungry" season (July – November), marked by the peak of agricultural work, depletion of food supply, and a rise in infectious diseases. Diboulo et al (2012) noted a substantial increase in deaths with heat intensification at lags of 0 – 1 days. A temperature rise of 1.0°C at lag 0—1 was associated with a 2.6% increase in mortality for all ages and 3.7% for children under five years, with people over 60 most vulnerable to extreme heat. Asamoah et al (2018) found a 42% rise in the likelihood of suffering a miscarriage with every degree rise in Wet Bulb Globe Temperature (WBGT), suggesting a connection between atmospheric heat exposure and adverse pregnancy outcomes in Accra. It was also discovered that an increase in Temperature to over 40°C during summer could affect the population who spend long hours in the heat, such as street vendors (Ngwenya et al. 2018).
Frimpong et al (2020) found that heat stress considerably influences farmers in Bawku East of Northern Ghana, with malaria and heat cramps identified among the recurring diseases. Nunfam et al (2019a) established a relationship (p < 0.05) between historical climate change threat awareness and work-related heat stress and the variance in educational accomplishment in the dissemination of coping approaches to work-related pressure from extreme temperatures. This agrees with the conclusions of Nunfam et al (2019b), who found a major variation in temperature-related morbidity with the type of mining activities among workforces in five mining spots in Western Ghana. Temperature and precipitation have altered the growth rates and survival of malaria pathogens. Several studies have demonstrated a decline in the spread of malaria in West Africa because of climate change-related increases in temperature and a decrease in precipitation (Ermert et al. 2012). In contrast, McGregor et al (1961), Lawoyin (2001), Reyburn et al (2011), and Ifatimehin and Ujoh (2014) observed a rise in morbidity or death during the rainy/hot season. Daniel (2015) reported a significant relationship between extreme temperature, rainfall, and heat rash.
Socioeconomic factors that contribute to population vulnerability to heat
Three (3%) of the articles identified in this review examined socioeconomic characteristics that contribute to increasing population vulnerability to heat. Grace et al (2012) considered the influence of education, home water supply, floor material, and livelihood zones to explore the association between surface temperatures, rainfall, and stunting in children under 5 years. Ibu and Bisong (2021) explored the urban bioclimatic discomfort index in Calabar, Nigeria, using socioeconomic and demographic parameters such as the urban heat island effect, age sensitivity, biophysical and sociocultural data, urban planning, and health. The study emphasises the need to integrate age and urban environmental factors in measuring vulnerability to heat discomfort in cities. Oluwafemi et al. (2023) considered the urban heat island, population density, age and health conditions such as elderly, young children, people with chronic diseases or disabilities, and low-income populations that have less capacity to adapt, as well as living conditions of people in informal settlements and areas with less vegetation. The study identified critical heat risk zones covering approximately 423 km2 in in densely populated areas.
Including demographic and socioeconomic factors is crucial in heat-human health studies because different age groups, health statuses, and socioeconomic classes have different sensitivities to heat, affecting their health differently. High population densities, especially in urban areas, exacerbate the urban heat island effect, which increases health risks. Socioeconomic status influences access to cooling resources, healthcare, and information on extreme heat, which is essential for mitigating heat-related health risks. Understanding these factors aids in developing targeted strategies to protect the most vulnerable populations from heat-related health issues.
Lag effects
The "lag period" refers to the time delay, often measured in days, between exposure to high temperatures and the observable health effects due to exposure. Lag periods vary between studies, e.g. 19 (19%) of the articles cited in this study observed a lag period of 0–28 days, 3 (3%) observed a lag period of 6–8 weeks, and 10 (10%) 1–10 months. 68 (68%) of the studies did not calculate a lag period. Faye et al. (2021) found that the relative mortality risk varied across different lags, e.g. the relative risk was below 1.0 at lag 0 days, indicating no immediate significant risk increase. However, a noticeable increase in relative risk was observed between lags 6 to 12 days, with the highest relative risk appearing at lags 8 and 9 days. The effect varied across different demographics, with significant associations among male mortality at lags 11 to 18 days and for female mortality at lags 7 to 14 days. Children aged 0 to 5 years showed significant risk at lags 8 to 14 days, and people aged 55 years or above were at a higher risk at lags 7 to 16 days. Interestingly, no significant association was observed for the age group of 6 to 54 years across different lags. This lag effect demonstrates the delayed impact of heat waves on mortality, highlighting the importance of considering varying time frames when assessing the health impacts of heat exposure in different demographic groups.
Various approaches have been used for estimating the lag period. The distributed lag nonlinear model (DLNM) is the most widely used, e.g. Nyadanu et al (2023), Bunker et al (2017), and Wiru et al (2020). The DLNM assesses the nonlinear association between heat exposure and mortality over different lag days, with a maximum lag of 25 days considered. This approach is useful for estimating heat waves' nonlinear and delayed effects on mortality. Nyadanu et al (2023) investigated the delayed effects of long-term heat stress on stillbirth rates in Ghana, using a DLNM to analyse the nonlinear exposure–response relationship and the time-structured lagged effects of heat stress. This approach is essential to understand the complex interplay between environmental factors like heat stress and adverse pregnancy outcomes. Egondi et al. (2012) employed a DLNM to understand the association between daily maximum temperature and Years of Life Lost. The study observes a J-shaped exposure–response curve, indicating a significant increase in YLL associated with cold temperatures. The study also explored the lag effect of temperature on YLL, showing that the impact of cold temperatures on YLL was observed mainly within the first five days after exposure. The study revealed no significant added impact of cold spells or heat waves on YLL beyond this lag effect. Bunker et al (2017) investigated the impact of heat exposure on non-communicable disease years of life lost (NCD-YLL) in rural Burkina Faso from 2000 to 2010. It uses a daily time series regression analysis with DLNMs. The key finding was that moderate to extreme heat exposure significantly increases premature deaths from NCDs. The most pronounced health effects were observed on the day of heat exposure, with a diminishing impact over the following four days. This lag effect demonstrates heat exposure's immediate and short-lived impacts on NCD-related mortality. Wiru et al (2020) used a DLNM to analyse the relationship between daily mean apparent temperature and all-cause mortality. The study found a nonlinear association, observing increased mortality risks at lower temperatures, especially from lag 2 to 4 days after exposure, with the highest risk occurring 3 days after exposure. This lag effect illustrates the delayed impact of temperature changes on mortality risks. The study also notes sex-specific differences in the temperature-mortality relationship.
Poisson regression is also often used to assess lag effects. Luque Fernández et al. (2009) used a Poisson autoregressive model to analyse the relationship between the weekly number of cholera cases and climatic variables. The study found a significant association between the increase in cholera cases and a rise in temperature 6 weeks prior, as well as an increase in rainfall 3 weeks before. Azongo et al (2012) used a time-series Poisson regression approach to analyse the short-term associations between mortality and mean daily temperature. They found a significant association at various lag days, indicating that temperature variations can have delayed effects on mortality.
Distribution of studies based on urban, rural, and informal settlements.
The review identified 34 studies (34%) focusing on urban areas. 21 studies (21%) were carried out in rural areas. The remaining 45 studies (45%) assessed the association between ambient temperature or heat waves and mortality in urban and rural areas. Table 4 summarises studies that have been conducted in urban and rural areas of tropical Africa. Some studies compared urban and rural populations based on their sensitivity to extreme heat (Nunfam et al. 2021; Jankowska et al. 2012; Alexander et al. 2013). Fewer studies were carried out in rural areas compared with urban, with the rural areas of West Africa having more studies relative to other regions. Together these studies revealed the harmful influence of heat on human health, behaviour, and productivity among farmers, labourers, and mining workers in rural communities (Nunfam 2021). While populations have diverse responses and coping mechanisms to heat exposure, these are inefficient in preventing heat-related morbidity and mortality at both the household and farm levels (Frimpong et al. 2020). Urban centres are known for their heat impacts on human health due to their propensity to create heat islands. The urban heat island (UHI), whereby temperatures in urban areas are higher than in the surrounding rural regions, exacerbates the influence of heat on human health (Sheridan and Allen 2015). Urbanisation is the leading cause of urban sprawl. Urban sprawl has led to the growth of informal settlements that house low-income populations in many Tropical African cities.
Informal settlements are an essential feature of tropical African cities, commonly identified as unplanned and densely-packed low-rise buildings with a high population (Yahia et al. 2018). The dwellers of informal settlements are more sensitive to the impact of extreme heat due to their low adaptive capacity, e.g. Lorena et al (2018) found an increase in non-communicable diseases in children, deteriorating mental health, and occupational hazard in adults of informal residences with low income due to extreme Temperature. The informal settlements are densely packed housing with poor building materials that lack access to public services and amenities, making their population particularly vulnerable to heat (Scott et al. 2017). The disparities in the designs of built-up expansion, vegetation and construction materials in cities can differentially affect the threat of heat-related morbidity and mortality. For instance, Egondi et al (2012) found that the extreme heat experienced in the neighbourhood of the informal settlements was more than the ambient temperature recorded in the nearest weather station by several oC. A study by Scott et al (2017) employed iButtons – an inexpensive device for measuring temperature and relative humidity, to investigate heat variations in an informal settlement in Nairobi. Both Scott et al (2017) and Egondi et al (2012) recognised that poor populations were at greater risk of extreme heat than wealthier populations, highlighting the social inequalities that exist in heat exposure and adverse health outcomes. There are, however, very few empirical studies on the vulnerability of human health to heat, particularly in the informal settlements of tropical Africa (Pasquini et al. 2020). Even though climate threat is projected for the African continent (Dosio 2017), studies in Zimbabwe have shown that informal settlements and urban outdoor workers are more vulnerable to extreme heat (Ngwenya et al. 2018). To this end, very little is known about the vulnerability to heat in tropical Africa.
Health outcomes
The primary health outcomes of the studies cited in this review are health risks associated with increased temperatures and heat stress (Joseph and Demot, 2021; Morakinyo et al. 2016; Van de Walle et al. 2022; Gratien Kiki et al. 2020; Mabuya and Scholes 2020; Sylla et al. 2018; Wright et al. 2022). For instance, Mushore et al. (2017) identified outdoor thermal discomfort in densely built-up areas, and Ndetto and Matzarakis (2013), Ndetto and Matzarakis (2017) and Sarr et al (2019) found heat stress and thermal discomfort to be the major health issues during the hot season leading to heat exhaustion, heatstroke, and overall discomfort affecting daily activities.
The review highlights the myriad of ways by which extreme heat affects human health, through different and varied health outcomes. Several studies report an increase in the incidence of diarrhoea, respiratory infections, malaria, and physiological stress associated with heatwaves, heat stress and extreme temperatures (Omonijo et al. (2011), Adeniyi and Oyekola (2017), Thandi et al. (2018), Njoku and Daramola (2019), and Adeboyejo et al. (2012)). Dukic et al. (2012) and Tunde et al. (2013) observed an increase in the prevalence of asthma, malaria, meningitis, and typhoid fever due to temperature, relative humidity, and air quality. Other studies have reported that increasing temperatures and relative humidity exacerbate heatstroke, heat stress, heat cramps, heat exhaustion, dehydration, kidney failures, acute meningitis, productivity loss, anxiety, increased risk of malaria and effects on social well-being among outdoor workers (Frimpong et al. (2014), Nunfam (2021), and Frimpong et al. (2020)).
The review also identifies several health outcomes, specifically relevant to children. Sylvia Blom et al (2022) found increased chronic and acute malnutrition in children due to extreme heat exposure. Scorgie et al (2023) found an increased risk of heat-related health issues such as heat exhaustion, dehydration, and potential impacts on foetal health. Nyadanu et al (2023) identified an increased risk of stillbirth associated with exposure to long-term heat stress. Bonell et al (2023) suggests that reducing maternal exposure to heat stress and strain will likely reduce foetal strain, potentially decreasing adverse birth outcomes.
Some studies have shown how extreme heat disproportionally affects the elderly and female population, e.g. Faye et al (2021) found that heat waves lasting three or more consecutive days increase the risk of death, with the elderly over 55 years and females being more affected.
Priorities for reducing the health impacts from extreme heat
There is a need for a more detailed analysis of cause-specific mortality to understand better and address regional seasonal mortality patterns in tropical Africa (Ndetto and Matzarakis 2013; Ndetto and Matzarakis 2017; Lawoyin 2001; Kynast-Wolf et al. 2005; Mutisya et al. 2010; Diboulo et al. 2012; Azongo et al. 2012; Mrema et al. 2012; Scott et al. 2017; Wiru et al. 2020).
Several studies emphasise the importance of integrating tree planting and urban greening in building and urban design and materials to enhance thermal comfort and ventilation to enhance thermal comfort and reduce health risks associated with extreme temperatures, particularly in regions where heat stress has a major impact on human health and productivity (Omonijo et al. (2013), Morakinyo et al. (2014), Njoku and Daramola (2019), Mushore et al. (2017), Mabuya and Scholes (2020) and Van de Walle et al. (2022)). Wright et al (2022) emphasise the need to develop climate-proof housing and improve access to essential services to support resilient coping mechanisms, particularly in rural areas, during heatwaves. Ndetto and Matzarakis (2013) prioritise adapting urban planning and architectural design to mitigate heat stress, including optimising street orientation, and building heights to enhance thermal comfort in urban areas.
Moreover, several studies have underscored the importance of implementing effective adaptation measures (Egondi et al. (2012), Dukic et al. (2012), Adeboyejo et al. (2012) and, Adeniyi and Oyekola (2017), Sarr et al. (2019)). These include enhancing public awareness, improving public health infrastructure, developing health action plans, enhancing disease surveillance and response systems, increasing community awareness, preparedness and education on health risks associated with climate change, and targeting children.
This review also finds that further research is needed to quantify better the impact of warming on socioeconomic activities and health, to inform more targeted and efficient adaptation strategies, which is crucial for mitigating the adverse effects of heatwaves and extreme temperatures on human health. Sylvia Blom et al (2022) suggested implementing healthcare and nutrition program strategies to reduce the impact of rising temperatures on child nutrition. Adeniyi and Oyekola's (2017) argue that improving regional climate modelling is a priority for better prediction of heat waves. Tunde et al. (2013) recommend public awareness and education about climate variability and its effects on health through broadcasting weather reports and educating people on the impacts of anthropogenic activities on the climate.
Additionally, practical measures using mosquito nets, clearing stagnant water, and avoiding residing near riverbeds are suggested to reduce the risk outcomes from future heatwaves. Future priorities for minimising these risks involve implementing heat stress management strategies, enhancing workplace heat stress policies, and improving awareness and training about heat-related health risks among outdoor workers (Ngwenya et al. 2018; Nunfam 2021). Future priorities for reducing these health risks include developing effective heat wave early warning systems and public health strategies tailored to the needs of the most vulnerable groups, such as the elderly, children, and female population, to enhance preparedness and response to heat waves and mitigating their impact on human health (Faye et al. 2021).
Adapting to extreme heat should take account of evidence from this review that extreme heat can affect female populations more (Faye et al. 2021). Scorgie et al (2023) emphasise the importance of developing culturally appropriate adaptation strategies to reduce heat risks for pregnant women. These strategies should consider local gender dynamics to empower women, enhance their autonomy, and improve community support during hot seasons. Nyadanu et al (2023) emphasise the need for public health and climate governance strategies to reduce maternal exposure to heat stress, particularly in rural areas, to lower the risk of stillbirth. These strategies may include developing heat stress warning systems, improving maternal healthcare services, and enhancing awareness and education about the risks of heat exposure during pregnancy. Bonell et al (2023) prioritises further research to explore the association between heat stress and pregnancy outcomes in various settings and populations, aiming to develop effective interventions.
Opportunities for improving study methodologies
The majority of studies cited in the review obtained the climate data from traditional weather stations (Trærup et al. 2011; Reyburn et al. 2011; Adeniyi 2009; Eludoyin 2014; Dukic et al. 2012), which means the estimates of climate are not necessarily identical to the conditions experienced by the population. This is because people experience thermal discomfort indoors as well as outdoors, in distinct locations which may be a significant distance from the outdoor weather station. Our review has highlighted the importance of understanding thermal stress in informal settlements, yet temperatures are rarely monitored in these settings. Moreover, many urban areas of tropical Africa lack dense in-situ monitoring networks that can provide air temperature data at high spatial resolution.
Advances in technology offer an opportunity to address some of the methodological gaps discussed above. It is possible to measure climatic conditions more closely to the populations being affected, even at the individual person level. For example, few studies have used wearable devices such as iButtons that collect data on air temperature, humidity, and UV radiation (Scott et al. 2017; Mabuya and Scholes 2020; Van de Walle et al. 2022) or EasyLog-USB and Lascar USB temperature and humidity sensors (Kwasi et al. 2014; Balogun and Balogun 2014; Frimpong et al. 2016; Kiki et al. 2020). Moreover, recent technological advancements have led to the development of intelligent sensors like microneedles, skin patches, tattoos, and stretchable electronics. These devices can monitor various physiological parameters, including sweat rate, sodium levels in sweat, skin temperature, and heart rate (Paulo Silva Cunha 2018) and facilitate the creation of Internet of Things (IoT) networks to measure environmental conditions (Chapman 2015).
Remotely sensed data from satellite observations provide greater spatial coverage of land surface temperatures than what can be achieved with traditional weather station data. However, only 2% of the articles cited in this review used freely accessible satellite thermal imagery to map land surface temperature (Ifatimehin and Ujoh 2014; Scott et al. 2017; Mushore et al. 2017; and Van de Walle et al. 2022). Thermal bands of satellite imagery such as Landsat, MODIS, and Sentinels, provide datasets with spatial resolution from 10 m to 1 km, enabling potentially high resolution thermal mapping in urban areas. Although Landsat 5–9 imagery has good spatial resolution (100 m), the image is acquired at 10.00 am, which is unsuitable for heat-human health studies because maximum temperatures occur later in the day and minimum temperatures earlier. Although satellites can provide high resolution temperature data, they provide estimates of land surface temperature, which is not the same as air temperature, and a conversion is necessary (Anderson et al. 2021; Wang et al. 2022; Khan et al. 2022).
Conclusions
The evidence gathered from 100 articles in this review revealed that dehydration, discomfort, and heat-related morbidity and death increased during high temperatures or heat waves. The harmful effects of extreme heat on human health in tropical Africa include declining mental health in adults of low-income residents (Lorena et al. 2018), an increase in miscarriage risk with each degree of temperature rise (Asamoah et al. 2018), and effects on the safety and well-being, psychological behaviour, productivity, and social comfort of outdoor workers who spend long hours performing manual labour (Nunfam et al. 2019a, b; Nunfam 2021). The findings of this study are consistent with previous findings that higher temperatures increase the incidence of morbidity. According to Liu et al (2021b), renal disease rose by 10% for every 1°C increase. Heat and mental health research evaluations show that morbidity rose by 0.9% to 22% for every 1°C increase (Liu et al. 2021a). According to Phung et al (2016), the risk of cardiovascular hospitalisation increased by 0.7%. According to Fatima et al (2021), occupational illnesses and injuries increase by 1% for every 1°C increase in temperature. Regarding morbidity or mortality, Faurie et al (2022) reported over 100% increases in case numbers. Given that more than 90% of urban population growth is anticipated in Asia and Africa (UN-Habitat 2014), urbanisation and increases in the artificial impervious surface are anticipated to impact the thermal environment due to the destruction of vegetation cover and the expansion of informal settlements. Almost 55% of Sub-Saharan Africa, according to UN-Habitat (2014), resides in informal settlements, which are more vulnerable to heat-related morbidity and mortality due to their dense population and poor living conditions. Heat-related health impacts are of concern in tropical Africa, which is already facing substantial heat stress due to the climate and environmental change exacerbated by anthropogenic activities and increasing greenhouse gas levels.
The impact of extreme heat on human health in tropical Africa is worsened by the population's relative poor socioeconomic and demographic status and the environmental quality. Green spaces are an essential contributor to human well-being. Studies have found that people dwelling in areas with less vegetation cover are more vulnerable to heat-related morbidity and mortality (Schinasi et al. 2018). Informal settlements are characterised by poor physical infrastructure and little vegetation cover, which influences the UHI effect and increases night-time temperatures. Nighttime cooling is essential for people to get a good night's sleep and recuperate from the day's heat. There is a strong association between amplified night-time heat and inadequate sleep; the consequence is more prevalent among the lower-income and ageing population (Obradovich et al. 2017). Most of the studies cited in this review reported increased heat-related morbidity and mortality during the dry/hot season and the heat/rainy season relative to the dry/cold season. For example, the prevalence of infectious diseases, such as malaria and diarrhoea, increased mortality in coastal towns of tropical Africa during the hot/wet season (Greenwood 1993; Ifatimehin and Ujoh 2014). The common reasons for excess mortality in these seasons are extreme heat and hygienic environments. The increased rain usually overstretches the sewage and drainage systems, leading to stagnant water and a wet environment.
Moreover, stagnant water and a damp environment offer numerous disease agents decent breeding and surviving grounds. In addition, the heat/rainy season, characterised by planting and growing crops, often coincides with the time of least food supply and poor nutritional status of the population (Rayco-solon et al. 2004). The dry/hot season is the transition period between Harmattan and the heat/rainy season in tropical African cities that border the Sahara Desert. The dry/hot season exhibits excess mortality due to extreme heat, increasing the time spent outdoors to try and cool down. The poor population that cannot afford air conditioning spends more time outside, making them vulnerable to disease pathogens (Pasquini et al. 2020). Moreover, their dwelling is usually overcrowded and poorly ventilated, leading to indoor air pollution, a significant cause of mortality peaks in informal settlements. There is a further increased risk of airborne disease and meningitis due to the Harmattan dust from the Sahara Desert during the dry/hot season. A common observation in most identified studies in tropical Africa was the age dependency of morbidity seasonality. Older people are at a higher risk of dying during the hot/dry season (Daniel 2015; Scott et al. 2017), while children below 9 years are most vulnerable to death in the heat/rainy season (Kynast-Wolf et al. 2006). Human sensitivity and ability to adapt to extreme heat's effects depend on the population's demographic and socioeconomic status. Generally, there is a link between the human dwelling environment, the socioeconomic characteristics, and the adverse effects of extreme heat.
References
Adegebo BO (2022) Urban thermal perception and self-reported health effects in Ibadan, southwest Nigeria. Int J Biometeorol 66(2):331–343. https://doi.org/10.1007/s00484-021-02168-z
Adeniyi MO (2009) Determination of heat stress in the tropical urban area of Ibadan, Southwestern Nigeria. Int J Nat Appl Sci 5:235–243
Adeniyi MO, Oyekola SO (2017) Assessment of heat and cold wave events over West Africa using three regional climate models. Ann Geophys 60(3):A0322–A0322. https://doi.org/10.4401/ag-7039
Agada LE, Yakubu MS (2022) Heat wave and its impact in northeastern Nigeria: A case study of Yobe State Nigeria. FUDMA J Sci 6(1):232–239. https://doi.org/10.33003/fjs-2022-0601-893
Agan PN (2017) Heat Waves Research and Impacts on Human Health: The Need for Studies in Nigeria. J Earth Sci Clim Change 8:418–427. https://doi.org/10.4172/2157-7617.1000418
Alaigba DB, Fabiyi OO, Akinnawo OS (2018) GIS in the assessment of the impact of microclimatic variables on human comfort in Akure. Niger South Afr J Geomatics 7(1):64–74. https://doi.org/10.4314/sajg.v7i1.5
Alcoforado MJ, Marques D, Garcia RA, Canário P, de Fátima NM, Nogueira H, Cravosa A (2015) Weather and climate versus mortality in Lisbon (Portugal) since the 19th Century. Appl Geogr 57:133–141. https://doi.org/10.1016/j.apgeog.2014.12.017
Alexander KA, Carzolio M, Goodin D, Vance E (2013) Climate change is likely to worsen the public health threat of diarrheal disease in Botswana. Int J Environ Res Public Health 10(4):1202–1230. https://doi.org/10.3390/ijerph10041202
Anderson V, Leung AC, Mehdipoor H, Jänicke B, Milošević D, Oliveira A, Manavvi S, Kabano P, Yuliya D, Aguilar APN, Joshua JK, Gustavo G, Vinicius de França CF, Sheila TN, Zurita-Milla R (2021) Technological opportunities for sensing of the health effects of weather and climate change: a state-of-the-art-review. Int J Biometeorol 65:779–803. https://doi.org/10.1007/s00484-020-02063-z
Arisco NJ, Sewe MO, Bärnighausen T, Sié A, Zabre P, Bunker A (2023) The effect of extreme temperature and precipitation on cause-specific deaths in rural Burkina Faso: a longitudinal study. Lancet Planet Health 7(6):e478–e489
Asamoah B, Kjellstrom T, Östergren PO (2018) Is ambient heat exposure levels associated with miscarriage or stillbirths in hot regions? A cross-sectional study using survey data from the Ghana Maternal Health Survey 2007. Int J Biometeorol 62(3):319–330. https://doi.org/10.1007/s00484-017-1402-5
Azhar G, Saha S, Ganguly P, Mavalankar D, Madrigano J (2017) Heat wave vulnerability mapping for India. Int J Environ Res Public Health 14(4):357. https://doi.org/10.3390/ijerph14040357
Azongo DK, Awine T, Wak G, Binka FN, Rexford OA (2012) A time series analysis of weather variables and all-cause mortality in the Kasena-Nankana Districts of Northern Ghana, 1995–2010. Glob Health Action 5(1):19073. https://doi.org/10.3402/gha.v5i0.19073
Balogun IA, Balogun AA (2014) Urban heat island and bioclimatological conditions in a hot-humid tropical city: the example of Akure, Nigeria. Die Erde–J Geograph Soc Berlin 14(5):3–15
Balogun IA, Daramola MT (2019) The outdoor thermal comfort assessment of different urban configurations within Akure City. Nigeria Urban Climate 29:100489. https://doi.org/10.1016/j.uclim.2019.100489
Basu R (2009) High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health 8(1):40. https://doi.org/10.1186/1476-069X-8-40
Basu R, Samet JM (2002) Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev 24(2):190–202. https://doi.org/10.1093/epirev/mxf007
Batté L, Ardilouze C, Déqué M (2018) Forecasting West African heat waves at sub seasonal and seasonal time scales. Mon Weather Rev 146(3):889–907. https://doi.org/10.1175/MWR-D-17-0211.1
Blom S, Ortiz-Bobea A, Hoddinott J (2022) Heat exposure and child nutrition: Evidence from West Africa. J Environ Econ Manag 115:102698. https://doi.org/10.1016/j.jeem.2022.102698
Bobb JF, Peng RD, Bell ML, Dominici F (2014) Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect 122(8):811–816. https://doi.org/10.1289/ehp.1307392
Bonell A, Sonko B, Badjie J, Samateh T, Saidy T, Sosseh F, Haines A (2022) Environmental heat stress on maternal physiology and fetal blood flow in pregnant subsistence farmers in The Gambia, West Africa: an observational cohort study. Lancet Planet Health 6(12):968–976
Bonell A, Vicedo-Cabrera A, Murray K, et al (2023) Assessing the impact of heat stress on growth faltering in the first 1000 days of life in rural Gambia. https://doi.org/10.21203/rs.3.rs-2358038/v1.
Brewster D, Greenwood B (1993) Seasonal variation of paediatric diseases in The Gambia. West Afr Annal Trop Paediatr 13(3):133–146. https://doi.org/10.1080/02724936.1993.11747637
Bühler JL, Shrikhande S, Kapwata T, Cissé G, Liang Y, Pedder H, Wright CY (2022) The association between apparent temperature and hospital admissions for cardiovascular disease in Limpopo Province, South Africa. Int J Environ Res Public Health 20(1):116. https://doi.org/10.3390/ijerph20010116
Bunker A, Sewe MO, Sié A, Rocklöv J, Sauerborn R (2017) Excess burden of non-communicable disease years of life lost from heat in rural Burkina Faso: a time series analysis of the years 2000–2010. BMJ Open, 7(11). https://doi.org/10.1136/bmjopen-2017-018068
Burkart K, Khan MM, Schneider A et al (2014) The effects of season and meteorology on human mortality in tropical climates: a systematic review. Trans R Soc Trop Med Hyg 108(7):393–401. https://doi.org/10.1093/trstmh/tru055
Camberlin P, Philippon N (2002) The East African March–May rainy season: Associated atmospheric dynamics and predictability over the 1968–97 period. J Clim 15(9):1002–1019. https://doi.org/10.1175/1520-0442(2002)015%3C1002:TEAMMR%3E2.0.CO;2
Cattani E, Merino A, Guijarro JA, Levizzani V (2018) East Africa rainfall trends and variability 1983–2015 using three long-term satellite products. Remote Sens 10(6):931. https://doi.org/10.3390/rs10060931
Chang CL, Shipley M, Marmot M, Poulter N (2004) Lower ambient temperature was associated with an increased risk of hospitalization for stroke and acute myocardial infarction in young women. J Clin Epidemiol 57(7):749–757. https://doi.org/10.1016/j.jclinepi.2003.10.016
Chapman L (2015) Urban meteorological networks: an urban climatologist panacea. In 9th International Conference on Urban Climate (IAUC & AMS), open plenary speech. pp 20–24
Chen TL, Lin H, Chiu YH (2022a) Heat vulnerability and extreme heat risk at the metropolitan scale: A case study of Taipei metropolitan area. Taiwan Urban Climate 41(7):101054. https://doi.org/10.1016/j.uclim.2021.101054
Chen L, Wang X, Cai X, Yang C, Lu X (2022b) Combined effects of artificial surface and urban blue-green space on land surface temperature in 28 major cities in China. Remote Sens 14(3):448. https://doi.org/10.3390/rs14030448
Cheng J, Xu Z, Zhao D, Xie M, Zhang H, Wang S, Su H (2016) The burden of extreme heat and heatwave on emergency ambulance dispatches: A time-series study in Huainan, China. Sci Total Environ 571:27–33. https://doi.org/10.1016/j.scitotenv.2016.07.103
Coates L, Haynes K, O’brien J, McAneney J, De Oliveira FD (2014) Exploring 167 years of vulnerability: An examination of extreme heat events in Australia 1844–2010. Environ Sci Policy 42:33–44. https://doi.org/10.1016/j.envsci.2014.05.003
Daniel OA (2015) Urban extreme weather: a challenge for a healthy Living environment in Akure, Ondo State. Niger Clim 3(4):775–791. https://doi.org/10.3390/cli3040775
Dapi LN, Rocklöv J, Nguefack-Tsague G, Tetanye E, Kjellstrom T (2010) Heat impact on schoolchildren in Cameroon, Africa: potential health threat from climate change. Glob Health Action 3(1):56–69. https://doi.org/10.3402/gha.v3i0.5610
Diboulo E, Sie A, Rocklöv J, Niamba L, Ye M, Bagagnan C, Sauerborn R (2012) Weather and mortality: a 10-year retrospective analysis of the Nouna Health and Demographic Surveillance System. Burkina Faso Global Health Action 5(1):19–31. https://doi.org/10.3402/gha.v5i0.19078
Diouf I, Deme A, Ndione JA, Gaye AT, Rodríguez-Fonseca B, Cissé M (2013) Climate and health: observation and modelling of malaria in the Ferlo (Senegal). CR Biol 336(5–6):253–260. https://doi.org/10.1016/j.crvi.2013.04.001
Dolney TJ, Sheridan SC (2006) The relationship between extreme heat and ambulance response calls for the city of Toronto, Ontario. Canada Environmental Research 101(1):94–103. https://doi.org/10.1016/j.envres.2005.08.008
Donaldson GC, Keatinge WR, Saunders RD (2003) Cardiovascular responses to heat stress and their adverse consequences in healthy and vulnerable human populations. Int J Hyperth 19(3):225–235. https://doi.org/10.1080/0265673021000058357
Dosio A (2017) Projection of temperature and heat waves for Africa with an ensemble of CORDEX Regional Climate Models. Clim Dyn 49(1–2):493–519. https://doi.org/10.1007/s00382-016-3355-5
Dukić V, Hayden M, Forgor AA, Hopson T, Akweongo P, Hodgson A, Pandya R (2012) The role of weather in meningitis outbreaks in Navrongo, Ghana: a generalized additive modeling approach. J Agric Biol Environ Stat 17:442–460. https://doi.org/10.1007/s13253-012-0095-9
Ebi KL, Vanos J, Baldwin JW, Bell JE, Hondula DM, Errett NA, Berry P (2021) Extreme weather and climate change: population health and health system implications. Annu Rev Public Health 42(1):293. https://doi.org/10.1146/annurev-publhealth-012420-105026
Efeoma M, Uduku O (2014) Assessing thermal comfort and energy efficiency in tropical African offices using the adaptive approach. Struct Surv 32(5):396–412. https://doi.org/10.1108/SS-03-2014-0015
Egondi T, Kyobutungi C, Kovats S, Muindi K, Ettarh R, Rocklöv J (2012) Time-series analysis of weather and mortality patterns in Nairobi’s informal settlements. Glob Health Action 5(1):19065. https://doi.org/10.3402/gha.v5i0.19065
Eludoyin OM (2014) A perspective of the diurnal aspect of thermal comfort in Nigeria. Atmos Climate Sci 4:696–709. https://doi.org/10.4236/acs.2014.44063
Eludoyin OM (2015) Assessment of daytime physiologic comfort, its perception and coping strategies among people in tertiary institutions in Nigeria. Weather Clim Extremes 10:70–84. https://doi.org/10.1016/j.wace.2015.06.006
EM-DAT (2023) The OFDA/CRED international disaster database. Université Catholique de Louvain, Brussels, Belgium. Available at http://www.emdat.be. Accessed 20 Feb 2023
Enete IC, Awuh ME, Ikekpeazu FO (2013) Assessment of Urban Heat Island situation in Douala Metropolis, Cameroon. J Geograph Earth Sci 2(1):55–57
Ermert V, Fink AH, Morse AP, Paeth H (2012) The impact of regional climate change on malaria risk due to greenhouse forcing and land-use changes in tropical Africa. Environ Health Perspect 120(1):77–84. https://doi.org/10.1289/ehp.1103681
Etard JF, Le Hesran JY, Diallo A, Diallo JP, Ndiaye JL, Delaunay V (2004) Childhood mortality and probable causes of death using verbal autopsy in Niakhar, Senegal, 1989–2000. Int J Epidemiol 33(6):1286–1292. https://doi.org/10.1093/ije/dyh259
Fatima SH, Rothmore P, Giles LC, Varghese BM (2021) Extreme heat and occupational injuries in different climate zones: A systematic review and meta-analysis of epidemiological evidence. Environ Int 148:106384. https://doi.org/10.1016/j.envint.2021.106384
Faurie C, Varghese BM, Liu J, Bi P (2022) Association between high temperature and heatwaves with heat-related illnesses: A systematic review and meta-analysis. Sci Total Environ, 158332. https://doi.org/10.1016/j.scitotenv.2022.158332.
Faye M, Dème A, Diongue AK, Diouf I (2021) Impact of different heat wave definitions on daily mortality in Bandafassi. Senegal Plos One 16(4):0249199. https://doi.org/10.1371/journal.pone.0249199
Foster J, Hodder SG, Lloyd AB, Havenith G (2020) Individual responses to heat stress: implications for hyperthermia and physical work capacity. Front Physiol 11:541483. https://doi.org/10.3389/fphys.2020.541483
Fotso-Nguemo TC, Vondou DA, Diallo I et al (2022) Potential impact of 1.5, 2 and 3°C global warming levels on heat and discomfort indices changes over Central Africa. Sci Total Environ 804:150099. https://doi.org/10.1016/j.scitotenv.2021.150099
Frimpong K, Oosthuizen J, Van Etten EJ (2014) Recent trends in temperature and relative humidity in Bawku East. Northern Ghana. https://doi.org/10.5539/jgg.v6n2p69
Frimpong K, Van Etten E, Oosthuizen J (2016) Barriers of adaptation to heat stress in Northeast Ghana. Int J Clim Change: Impact Responses 8(2):53–65. https://doi.org/10.18848/1835-7156/CGP
Frimpong K, Odonkor ST, Kuranchie FA, Nunfam VF (2020) Evaluation of heat stress impacts and adaptations: perspectives from smallholder rural farmers in Bawku East of Northern Ghana. Heliyon 6(4):03679. https://doi.org/10.1016/j.heliyon.2020.e03679
Gabriel KM, Endlicher WR (2011) Urban and rural mortality rates during heat waves in Berlin and Brandenburg. Germany Environ Pollut 159(8–9):2044–2050. https://doi.org/10.1016/j.envpol.2011.01.016
Gosling SN, Lowe JA, McGregor GR, Pelling M, Malamud BD (2009) Associations between elevated atmospheric temperature and human mortality: a critical review of the literature. Clim Change 92:299–341. https://doi.org/10.1007/s10584-008-9441-x
Gosling SN, Bryce EK, Dixon PG, Gabriel KM, Gosling EY, Hanes JM, Wanka ER (2014) A glossary for biometeorology. Int J Biometeorol 58:277–308
Grace K, Davenport F, Funk C, Lerner AM (2012) Child malnutrition and climate in Sub-Saharan Africa: An analysis of recent trends in Kenya. Appl Geogr 35(1–2):405–413. https://doi.org/10.1016/j.apgeog.2012.06.017
Green H, Bailey J, Schwarz VJ, Ebi K, Benmarhnia T (2019) Impact of heat on mortality and morbidity in low and middle income countries: a review of the epidemiological evidence and considerations for future research. Environ Res 171:80–91. https://doi.org/10.1016/j.envres.2019.01.010
Guo Y (2017) Hourly associations between heat and ambulance calls. Environ Pollut 220:1424–1428. https://doi.org/10.1016/j.envpol.2016.10.091
Gyilbag A, Amou M, Tulcan RX, Zhang L, Demelash T, Xu Y (2021) Characteristics of Enhanced Heatwaves over Tanzania and Scenario Projection in the 21st Century. Atmosphere 12(8):1026. https://doi.org/10.3390/atmos12081026
Hajat S, Kosatky T (2010) Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Commun Health 64(9):753–760. https://doi.org/10.1136/jech.2009.087999
Hajat S, O’Connor M, Kosatsky T (2010) Health effects of hot weather: from awareness of risk factors to effective health protection. The Lancet 375(9717):856–863. https://doi.org/10.1016/S0140-6736(09)61711-6
Hammer GP, Some F, Muller O, Kynast-Wolf G, Kouyate B, Becher H (2006) Pattern of cause-specific childhood mortality in a malaria endemic area of Burkina Faso. Malar J 5:47. https://doi.org/10.1186/1475-2875-5-47
Harrington LJ, Frame DJ, Hawkins E, Joshi M (2017) Seasonal cycles enhance disparities between low-and high-income countries in exposure to monthly temperature emergence with future warming. Environ Res Lett 12(11):114039. https://doi.org/10.1088/1748-9326/aa95ae
Hatvani-Kovacs G, Belusko M, Pockett J, Boland J (2016) Assessment of heatwave impacts. Procedia Eng 169:316–323
He BJ, Xiong K, Dong X (2023) Urban Heat Adaptation and a Smart Decision Support Framework. Smart Buildings and Technologies for Sustainable Cities in China. Singapore, Springer Nature Singapore, pp 65–84
Herold N, Alexander L, Green D, Donat M (2017) Greater increases in temperature extremes in low versus high income countries. Environ Res Lett 12(3):034007. https://doi.org/10.1088/1748-9326/aa5c43
Hess JJ, Errett NA, McGregor G, Busch Isaksen T, Wettstein ZS, Wheat SK, Ebi KL (2023) Public Health Preparedness for Extreme Heat Events. Annu Rev Public Health 44:301–321. https://doi.org/10.1146/annurev-publhealth071421-025508
Hondula DM, Davis RE, Leisten MJ, Saha MV, Veazey LM, Wegner CR (2012) Fine-scale spatial variability of heat-related mortality in Philadelphia County, USA, from 1983–2008: a case-series analysis. Environ Health 11(1):1–11. https://doi.org/10.1186/1476-069X-11-16
Ifatimehin OO, Ujoh F (2014) Application of Remotely sensed Data for Modeling Malaria Infection in Lokoja, Nigeria. Int J Trop Dis Health 4(6):634–644
Ikeda T, Kapwata T, Behera SK, Minakawa N, Hashizume M, Sweijd N, Wright CY (2019) Climatic factors in relation to diarrhoea hospital admissions in rural Limpopo. South Afr Atmos 10(9):522. https://doi.org/10.3390/atmos10090522
Iyakaremye V, Zeng G, Yang X, Zhang G, Ullah I, Gahigi A, Ayugi B (2021) Increased high-temperature extremes and associated population exposure in Africa by the mid-21st century. Sci Total Environ 790:148162
Jaffar S, Leach A, Greenwood A et al (1997) Changes in the pattern of infant and childhood mortality in Upper River Division, The Gambia, from 1989 to 1993. Trop Med Int Health 2:28–37. https://doi.org/10.1046/j.1365-3156.1997.d01-131.x
Jankowska MM, Lopez-Carr D, Funk C, Husak GJ, Chafe ZA (2012) Climate change and human health: Spatial modeling of water availability, malnutrition, and livelihoods in Mali, Africa. Appl Geogr 33:4–15. https://doi.org/10.1016/j.apgeog.2011.08.009
Jay O, Capon A, Berry P, Broderick C, de Dear R, Havenith G, Ebi KL (2021) Reducing the health effects of hot weather and heat extremes: from personal cooling strategies to green cities. Lancet 398(10301):709–724. https://doi.org/10.1016/s0140-6736(21)01209-5
Jessel S, Sawyer S, Hernández D (2019) Energy, poverty, and health in climate change: a comprehensive review of an emerging literature. Front Publ Health 7:357. https://doi.org/10.3389/fpubh.2019.00357
Kapwata T, Gebreslasie MT, Mathee A, Wright CY (2018a) Current and potential future seasonal trends of indoor dwelling temperature and likely health risks in rural Southern Africa. Int J Environ Res Public Health 15(5):952. https://doi.org/10.3390/ijerph15050952
Kapwata T, Language B, Piketh S, Wright CY (2018b) Variation of indoor particulate matter concentrations and association with indoor/outdoor temperature: a case study in rural Limpopo. South Afr Atmosphere 9(4):124. https://doi.org/10.3390/atmos9040124
Kapwata T, Wright CY, Du Preez DJ, Kunene Z, Mathee A, Ikeda T, Blesic S (2021) Exploring rural hospital admissions for diarrhoeal disease, malaria, pneumonia, and asthma in relation to temperature, rainfall and air pollution using wavelet transform analysis. Sci Total Environ 791:148307
Kenney WL, Craighead DH, Alexander LM (2014) Heat waves, aging, and human cardiovascular health. Med Sci Sports Exerc 46(10):1891. https://doi.org/10.1249/MSS.0000000000000325
Kenny GP, Notley SR, Flouris AD, Grundstein A (2020) Climate change and heat exposure: impact on health in occupational and general populations. A Clinical and Evidence-Based Guide, Exertional Heat Illness, pp 225–261
Khan F, Das B, Mishra RK (2022) An automated land surface temperature modelling tool box designed using spatial technique for ArcGIS. Earth Sci Inf 15(1):725–733. https://doi.org/10.1007/s12145-021-00722-2
Kiki G, Kouchadé C, Houngan A, Zannou-Tchoko SJ, André P (2020) Evaluation of thermal comfort in an office building in the humid tropical climate of Benin. Build Environ 185:107277. https://doi.org/10.1016/j.buildenv.2020.107277
Klok EL, Kluck JJ (2018) Reasons to adapt to urban heat (in the Netherlands). Urban Climate 23:342–351. https://doi.org/10.1016/j.uclim.2016.10.005
Kotharkar R, Ghosh A (2022) Progress in extreme heat management and warning systems: A systematic review of heat-health action plans (1995–2020). Sustain Cities Soc 76(4):103487. https://doi.org/10.1016/j.scs.2021.103487
Kottek M, Grieser J, Beck C, Rudolf B, Rubel F (2006) World Map of the Köppen-Geiger climate classification updated. Meteorol Z 15:259–263. https://doi.org/10.1127/0941-2948/2006/0130
Kunene Z, Kapwata T, Mathee A, Sweijd N, Minakawa N, Naidoo N, Wright CY (2023) Exploring the Association between Ambient Temperature and Daily Hospital Admissions for Diarrhea in Mopani District, Limpopo Province South Africa. Healthcare 11(9):1251. https://doi.org/10.3390/healthcare11091251
Kwasi F, Oosthuizen J, Etten EV (2014) The extent of heat on health and sustainable farming in ghana–bawku east. Sustain Agric Res 3(5):20–37. https://doi.org/10.22004/ag.econ.230515
Kynast-Wolf G, Hammer G, Müller O, Kouyaté B, Becher H (2006) Season of death and birth predict patterns of mortality in Burkina Faso. Int J Epidemiol 35:427–435. https://doi.org/10.1093/ije/dyi150
Kynast-Wolf G, Preuß M, Sié A, Kouyaté B, Becher H (2010) Seasonal patterns of cardiovascular disease mortality of adults in Burkina Faso, West Africa. Trop Med Int Health 15:1082–1089. https://doi.org/10.1111/j.1365-3156.2010.02586.x
Laranjeira K, Göttsche F, Birkmann J, Garschagen M (2021) Heat vulnerability and adaptive capacities: Findings of a household survey in Ludwigsburg, BW. German Clim Change 166(1):1–19. https://doi.org/10.1007/s10584-021-03103-2
Lawoyin TO (2001) Risk factors for infant mortality in a rural community in Nigeria. J Royal Soc Prom Health 121(2):114–118. https://doi.org/10.1177/146642400112100213
Leal Filho W, Icaza LE, Neht A, Klavins M, Morgan EA (2018) Coping with the impacts of urban heat islands. A literature-based study on understanding urban heat vulnerability and the need for resilience in cities in a global climate change context. J Clean Prod 171(8):1140–1149. https://doi.org/10.1016/j.jclepro.2017.10.086
Liu J, Varghese BM, Hansen A, Borg MA et al (2021a) Hot weather as a risk factor for kidney disease outcomes: A systematic review and meta-analysis of epidemiological evidence. Sci Total Environ 801:149806. https://doi.org/10.1016/j.scitotenv.2021.149806
Liu J, Varghese BM, Hansen A, Xiang J, Zhang Y et al (2021b) Is there an association between hot weather and poor mental health outcomes? A systematic review and meta-analysis. Environ Int 153:106533. https://doi.org/10.1016/j.envint.2021.106533
Longo-Mbenza B, Phanzu-Mbete LB, M’Buyamba-Kabangu JR et al (1999) Hematocrit and stroke in black Africans under tropical climate and meteorological influence. Annales De Médecine Interne 150(3):171–177
Lorena P, Lisa A, Jessica L, Christie G, Chris J (2018) Emerging climate change related public health challenges: the potential impacts of temperature rise on health outcomes in Dar es Salaam. Tanzania, Urban Africa Risk Knowledge Briefing, UN Habitat
Luque Fernández MÁ, Bauernfeind A, Jiménez JD et al (2009) Influence of temperature and rainfall on the evolution of cholera epidemics in Lusaka, Zambia, 2003–2006: analysis of a time series. Trans R Soc Trop Med Hyg 103(2):137–143. https://doi.org/10.1016/j.trstmh.2008.07.017
Ma W, Chen R, Kan H (2014) Temperature-related mortality in 17 large Chinese cities: how heat and cold affect mortality in China. Environ Res 134:127–133. https://doi.org/10.1016/j.envres.2014.07.007
Mabuya B, Scholes M (2020) The three little houses: A comparative study of indoor and ambient temperatures in three low-cost housing types in Gauteng and Mpumalanga, South Africa. Int J Environ Res Publ Health 17(10):3524. https://doi.org/10.3390/ijerph17103524
Mahlstein I, Knutti R, Solomon S, Portmann RW (2011) Early onset of significant local warming in low latitude countries. Environ Res Lett 6(3):034009. https://doi.org/10.1088/1748-9326/6/3/034009
Manyuchi AE, Vogel C, Wright CY, Erasmus B (2022) The self-reported human health effects associated with heat exposure in Agincourt sub-district of South Africa. Humanit Soc Sci Commun, 9(1).https://doi.org/10.1057/s41599-022-01063-1
Maposa D, Seimela AM, Sigauke C, Cochran JJ (2021) Modelling temperature extremes in the Limpopo province: Bivariate time-varying threshold excess approach. Nat Hazards 107:2227–2246. https://doi.org/10.1007/s11069-021-04608-w
Martineau P, Behera SK, Nonaka M, Jayanthi R, Ikeda T, Minakawa N, Mabunda QE (2022) Predicting malaria outbreaks from sea surface temperature variability up to 9 months ahead in Limpopo, South Africa, using machine learning. Front Public Health 10:962377. https://doi.org/10.3389/fpubh.2022.962377
McGregor IA, Billewicz WZ, Thomson AM (1961) Growth and Mortality in Children in an African Village. BMJ 2:1661–1666. https://doi.org/10.1136/bmj.2.5268.1661
Mora C, Counsell CW, Bielecki CR, Louis LV (2017) Twenty-seven ways a heat wave can kill you: deadly heat in the era of climate change. Circ: Cardiovas Qual Outcomes 10(11):1–3. https://doi.org/10.1161/CIRCOUTCOMES.117.004233
Morakinyo TE, Adegun OB, Balogun AA (2016) The effect of vegetation on indoor and outdoor thermal comfort conditions: Evidence from a microscale study of two similar urban buildings in Akure. Niger Indoor Built Environ 25(4):603–617. https://doi.org/10.1177/1420326X14562455
Mrema S, Shamte A, Selemani M, Masanja H (2012) The influence of weather on mortality in rural Tanzania: a time-series analysis 1999–2010. Glob Health Action 5(1):19068. https://doi.org/10.3402/gha.v5i0.19068
Mutanga O, Mushore TD, Odindi J, Dube T (2018) Outdoor thermal discomfort analysis in Harare, Zimbabwe in Southern Africa. South Afr Geograph J Suid-Afrikaanse Geografiese Tydskrif 100(2):162–179. https://doi.org/10.1080/03736245.2017.1339630
Mutisya M, Orindi B, Emina J, Zulu E, Ye Y (2010) Is mortality among under-five children in Nairobi slums seasonal? Tropical Med Int Health 15:132–139. https://doi.org/10.1111/j.1365-3156.2009.02419.x
Myint SW, Wentz EA, Brazel AJ, Quattrochi DA (2013) The impact of distinct anthropogenic and vegetation features on urban warming. Landscape Ecol 28:959–978. https://doi.org/10.1007/s10980-013-9868-y
Ncongwane KP, Botai JO, Sivakumar V, Botai CM (2021) A literature review of the impacts of heat stress on human health across Africa. Sustainability 13(9):5312. https://doi.org/10.3390/su13095312
Ndetto EL, Matzarakis A (2013) Basic analysis of climate and urban bioclimate of Dar es Salaam. Tanzania Theoretical Appl Climatol 114(1):213–226. https://doi.org/10.1007/s00704-012-0828-2
Ndetto EL, Matzarakis A (2017) Assessment of human thermal perception in the hot-humid climate of Dar es Salaam, Tanzania. Int J Biometeorol 61:69–85. https://doi.org/10.1007/s00484-016-1192-1
Ng S, Cowling BJ (2014) Association between temperature, humidity, and ebolavirus disease outbreaks in Africa, 1976 to 2014. Eurosurveillance 19(35):20892
Ngwenya B, Oosthuizen J, Cross M, Frimpong K (2018) Emerging heat-related climate change influences; a public health challenge to health care practitioners and policy makers: insight from Bulawayo, Zimbabwe. Int J Dis Risk Reduct 27:596–601. https://doi.org/10.1016/j.ijdrr.2017.10.012
Nigerian Meteorological Agency (2021) In Salami A, Fenta AA (2022) Spatio-temporal evaluation of open access precipitation products with rain gauge observations in Nigeria. Arab J Geosci 15(24):1785. https://doi.org/10.1007/s12517-022-11071-9
Niu Y, Li Z, Gao Y et al (2021) A Systematic Review of the Development and Validation of the Heat Vulnerability Index: Major Factors, Methods, and Spatial Units. Curr Clim Change Rep 7(3):87–97. https://doi.org/10.1007/s40641-021-00173-3
Njoku CA, Daramola MT (2019) Human outdoor thermal comfort assessment in a tropical region: a case study. Earth Syst Environ 3:29–42. https://doi.org/10.1007/s41748-019-00090-4
Ntoumos A, Hadjinicolaou P, Zittis G, Proestos Y, Lelieveld J (2022) Projected Air Temperature Extremes and Maximum Heat Conditions over the Middle East-North Africa (MENA) Region. Earth Syst Environ 6(2):343–359. https://doi.org/10.1007/s41748-022-00297-y
Nunfam VF (2021) Mixed methods study into social impacts of work-related heat stress on Ghanaian mining workers: A pragmatic research approach. Heliyon 7(5):06918. https://doi.org/10.1016/j.heliyon.2021.e06918
Nunfam VF, Oosthuizen J, Van Etten A-A, EJ, Frimpong K, (2019a) Perceptions of climate change and occupational heat stress risks and adaptation strategies of mining workers in Ghana. Sci Total Environ 657:365–378. https://doi.org/10.1016/j.scitotenv.2018.11.480
Nunfam VF, Van Etten EJ, Oosthuizen J, Adusei-Asante K, Frimpong K (2019b) Climate change and occupational heat stress risks and adaptation strategies of mining workers. Perspectives of supervisors and other stakeholders in Ghana. Environ Res 16(9):147–155. https://doi.org/10.1016/j.envres.2018.11.004
Nunfam VF, Afrifa-Yamoah E, Adusei-Asante, et al (2021) Construct validity and invariance assessment of the social impacts of occupational heat stress scale (SIOHSS) among Ghanaian mining workers. Sci Total Environ 771:144911. https://doi.org/10.1016/j.scitotenv.2020.144911
Nyadanu SD, Tessema GA, Mullins B, Kumi-Boateng B, Ofosu AA, Pereira G (2023) Prenatal exposure to long-term heat stress and stillbirth in Ghana: A within-space time-series analysis. Environ Res 222:115385. https://doi.org/10.1016/j.envres.2023.115385
Obe OB, Morakinyo TE, Mills G (2023) Assessing heat risk in a sub-saharan African humid city, Lagos, Nigeria, using numerical modelling and open-source geospatial socio-demographic datasets. City Environ Interact 20:100128. https://doi.org/10.1016/j.cacint.2023.100128
Obradovich N, Migliorini R, Mednick SC, Fowler JH (2017) Nighttime temperature and human sleep loss in a changing climate. Sci Adv 3(5):1601555. https://doi.org/10.1126/sciadv.1601555
Odekunle TO, Balogun EE, Ogunkoya OO (2005) On the prediction of rainfall onset and retreat dates in Nigeria. Theoret Appl Climatol 81:101–112. https://doi.org/10.1007/s00704-004-0108-x
Olatunde AF (2016) The Intensity and Extent of Thermal Discomfort in Lokoja. Nigeria Int J Soc Sci 10(4):17–31
Oloukoi G, Bob U, Jaggernath J (2014) Perception and trends of associated health risks with seasonal climate variation in Oke-Ogun region, Nigeria. Health Place 25:47–55. https://doi.org/10.1016/j.healthplace.2013.09.009
Omonijo AG (2017) Assessing seasonal variations in urban thermal comfort and potential health risks using Physiologically Equivalent Temperature: A case of Ibadan, Nigeria. Urban Climate 21:87–105. https://doi.org/10.1016/j.uclim.2017.05.006
Omonijo AG, Adeofun CO, Oguntoke O, Matzarakis A (2013) Relevance of thermal environment to human health: a case study of Ondo State. Nigeria Theor Appl Climatol 113(1):205–212. https://doi.org/10.1007/s00704-012-0777-9
Pasquini L, van Aardenne L, Godsmark CN, Lee J, Jack C (2020) Emerging climate change-related public health challenges in Africa: A case study of the heat-health vulnerability of informal settlement residents in Dar es Salaam. Tanzania Sci Total Environ 747(3):141355. https://doi.org/10.1016/j.scitotenv.2020.141355
Paz S (2009) Impact of temperature variability on cholera incidence in southeastern Africa, 1971–2006. EcoHealth 6(3):340–345. https://doi.org/10.1007/s10393-009-0264-7
Périard JD, Eijsvogels TM, Daanen HA (2021) Exercise under heat stress: thermoregulation, hydration, performance implications, and mitigation strategies. Physiol Rev. https://doi.org/10.1152/physrev.00038.2020
Phung D, Thai PK, Guo Y, Morawska L, Rutherford S, Chu C (2016) Ambient temperature and risk of cardiovascular hospitalization: An updated systematic review and meta-analysis. Sci Total Environ 550:1084–1102. https://doi.org/10.1016/j.scitotenv.2016.01.154
Ragatoa DS, Ogunjobi KO, Okhimamhe AA, Klutse NAB, Lamptey BL (2018) A predictive study of heat wave characteristics and their spatio-temporal trends in climatic zones of Nigeria. Model Earth Syst Environ 4(3):1125–1151. https://doi.org/10.1007/s40808-018-0480-7
Rahman MNA, Adnan AA (2023) A Review on Heat Stress Issues Among Workers at Automotive Service Centre. J Adv Res Appl Sci Eng Technol 32(3):334–341. https://doi.org/10.37934/araset.32.3.334341
Rajagopal P, Priya RS, Senthil R (2023) A review of recent developments in the impact of environmental measures on urban heat island. Sustain Cities Soc 88:104279. https://doi.org/10.1016/j.scs.2022.104279
Rayco-Solon P, Moore SE, Fulford AJ, Prentice AM (2004) Fifty-year mortality trends in three rural African villages. Trop Med Int Health 9:1151–1160. https://doi.org/10.1111/j.1365-3156.2004.01325.x
Reyburn R, Kim DR, Emch M et al (2011) Climate variability and the outbreaks of cholera in Zanzibar, East Africa: a time series analysis. Am J Trop Med Hyg 84(6):862. https://doi.org/10.4269/ajtmh.2011.10-0277
Sankoh OA, Kynast-Wolf G, Kouyaté B, Becher H (2003) Patterns of adult and old-age mortality in rural Burkina Faso. J Public Health 25:372–376. https://doi.org/10.1093/pubmed/fdg080
Sanz-Barbero B, Linares C, Vives-Cases C, González JL, López-Ossorio JJ, Díaz J (2018) Heat wave and the risk of intimate partner violence. Sci Total Environ 644:413–419. https://doi.org/10.1016/j.scitotenv.2018.06.368
Sarr AB, Diba I, Basse J, Sabaly HN, Camara M (2019) Future evolution of surface temperature extremes and the potential impacts on the human health in Senegal. Afr J Environ Sci Technol 13(12):482–510. https://doi.org/10.5897/AJEST2019.2757
Schinasi LH, Benmarhnia T, De Roos AJ (2018) Modification of the association between high ambient temperature and health by urban microclimate indicators: A systematic review and meta-analysis. Environ Res 161(4):168–180. https://doi.org/10.1016/j.envres.2017.11.004
Scorgie F, Lusambili A, Luchters S, Khaemba P, Filippi V, Nakstad B, Chersich MF (2023) “Mothers get really exhausted!” The lived experience of pregnancy in extreme heat: Qualitative findings from Kilifi. Kenya Soc Sci Med 335:116223. https://doi.org/10.1016/j.socscimed.2023.116223
Scott AA, Misiani H, Okoth J, Jordan A, Gohlke J, Ouma G, Waugh DW (2017) Temperature and heat in informal settlements in Nairobi. PLoS ONE 12:11. https://doi.org/10.1371/journal.pone.0187300
Sheridan SC, Allen MJ (2015) Changes in the frequency and intensity of extreme temperature events and human health concerns. Curr Clim Change Rep 1(3):155–162. https://doi.org/10.1007/s40641-015-0017-3
Sheridan SC, Allen MJ (2018) Temporal trends in human vulnerability to excessive heat. Environ Res Lett 13(4):043001. https://doi.org/10.1088/1748-9326/aab214
Sherwood SC, Huber M (2010) An adaptability limit to climate change due to heat stress. Proc Natl Acad Sci 107(21):9552–9555. https://doi.org/10.1073/pnas.0913352107
Son JY, Lane KJ, Lee JT, Bell ML (2016) Urban vegetation and heat-related mortality in Seoul, Korea. Environ Res 151:728–733. https://doi.org/10.1016/j.envres.2016.09.001
Sovacool BK, Demski C, Noel L (2021) Beyond climate, culture, and comfort in European preferences for low-carbon heat. Glob Environ Chang 66:102200. https://doi.org/10.1016/j.gloenvcha.2020.102200
Sylla MB, Faye A, Giorgi F, Diedhiou A, Kunstmann H (2018) Projected heat stress under 1.5 C and 2 C global warming scenarios creates unprecedented discomfort for humans in West Africa. Earth’s Future 6(7):1029–1044. https://doi.org/10.1029/2018EF000873
Thiam S, Diène AN, Sy I, Winkler MS, Schindler C, Ndione JA, Faye O, Vounatsou P, Utzinger J, Cissé G (2017) Association between childhood diarrhoeal incidence and climatic factors in urban and rural settings in the health district of Mbour, Senegal. Int J Environ Res Publ Health 14(9):1049. https://doi.org/10.3390/ijerph14091049
Thompson AA, Matamale L, Kharidza SD (2012) Impact of climate change on children’s health in Limpopo Province, South Africa. Int J Environ Res Public Health 9(3):831–854. https://doi.org/10.3390/ijerph9030831
Thomson H, Simcock N, Bouzarovski S, Petrova S (2019) Energy poverty and indoor cooling: An overlooked issue in Europe. Energy Build 196:21–29. https://doi.org/10.1016/j.enbuild.2019.05.014
Trærup SL, Ortiz RA, Markandya A (2011) The costs of climate change: a study of cholera in Tanzania. Int J Environ Res Public Health 8(12):4386–4405. https://doi.org/10.3390/ijerph8124386
Tsuzuki K (2023) Effects of heat exposure on the thermoregulatory responses of young children. J Therm Biol 113:103507. https://doi.org/10.1016/j.jtherbio.2023.103507
Tunde AM, Adeleke EA, Adeniyi EE (2013) Impact of climate variability on human health in Ilorin. Niger Environ Nat Resourc Res 3(1):127. https://doi.org/10.5539/enrr.v3n1p127
UN-Habitat (2014) The State of African Cities. United Nations Human Settlements Programme, Nairobi, Kenya. United Nations (2014) Urbanization and sustainable development: towards a new United Nations Urban Agenda. Meeting document (CEB/2014/HLCP-28/CRP.5) of the High Level Committee on Programmes Twenty-Eight Session UN HQs (New York) (CR-6). https://habnet.unhabitat.org/sites/default/files/oo/urbanization-andsustainable-development.pdf
Upla DJI, Bisong DDN (2021) Urban Bio Climatic Discomfort Index Of Residents In Calabar Metropolis Cross River State Being Tetffund Research Grant Study Under Taken. Urban Bio Clim Discomfort Index Residents Calabar Metropolis Cross River State Being Tetffund Res Grant Stud Under Taken 91(1):12–12. https://doi.org/10.47119/Ijrp1009111220212647
Van de Walle J, Brousse O, Arnalsteen L, Brimicombe C, Byarugaba D, Demuzere M, Van Lipzig NPM (2022) Lack of vegetation exacerbates exposure to dangerous heat in dense settlements in a tropical African city. Environ Res Lett 17(2):024004. https://doi.org/10.1088/1748-9326/ac47c3
Wang R, Voogt J, Ren C (2022) Spatial-temporal variations of surface urban heat island: An application of local climate zone into large Chinese cities. Build Environ 222(11):109378. https://doi.org/10.1016/j.buildenv.2022.109378
Wiru K, Oppong FB, Agyei O, Zandoh C, Nettey OE, Adda R, Asante KP (2020) The influence of apparent temperature on mortality in the Kintampo Health and Demographic Surveillance area in the Middle Belt of Ghana: a retrospective time-series analysis. J Environ Public Health. https://doi.org/10.1155/2020/5980313
World Meteorological Organization (2016) Statement on the status of the global climate in 2015. Available at: http://public.wmo.int/en/%0Amedia/press-release/provisionalwmo-statement-status-of-global-climate-2016. Accessed 17 Oct 2019
Wright CY, Street RA, Cele N, Kunene Z, Balakrishna Y, Albers PN, Mathee A (2017a) Indoor temperatures in patient waiting rooms in eight rural primary health care centers in northern South Africa and the related potential risks to human health and wellbeing. Int J Environ Res Public Health 14(1):43. https://doi.org/10.3390/ijerph14010043
Wright CY, Albers PN, Mathee A, Kunene Z, D’Este C, Swaminathan A, Lucas RM (2017b) Sun protection to improve vaccine effectiveness in children in a high ambient ultraviolet radiation and rural environment: an intervention study. BMC Public Health 17:1–8. https://doi.org/10.1186/s12889-016-3966-0
Wright CY, Wernecke B, Kapwata T, Kunene Z, Mathee A, Vande Hey J, Theron L (2022) Perceptions of thermal comfort and coping mechanisms related to indoor and outdoor temperatures among participants living in rural villages in Limpopo province, South Africa. South African Journal of Psychology, 52(4), 449–459. https://orcid.org/0000-0001-9608-818X.
Wu CY, Zaitchik BF, Gohlke JM (2018) Heat waves and fatal traffic crashes in the continental United States. Accident Anal Prevent 119:195–201. https://doi.org/10.1016/j.aap.2018.07.025
Yahia MW, Johansson E, Thorsson S, Lindberg F, Rasmussen MI (2018) Effect of urban design on microclimate and thermal comfort outdoors in warm-humid Dar es Salaam. Tanzania Int J Biometeorol 62(3):373–385. https://doi.org/10.1007/s00484-017-1380-7
Ye Y, Zulu E, Mutisya M, Orindi B, Emina J, Kyobutungi C (2009) Seasonal pattern of pneumonia mortality among under-five children in Nairobi’s informal settlements. Am J Trop Med Hyg 81:770–775. https://doi.org/10.4269/ajtmh.2009.09-0070
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kunda, J.J., Gosling, S.N. & Foody, G.M. The effects of extreme heat on human health in tropical Africa. Int J Biometeorol 68, 1015–1033 (2024). https://doi.org/10.1007/s00484-024-02650-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-024-02650-4