Abstract
Background
Continuous kidney replacement therapy (CKRT) is a mainstay of therapy for management of severe acute kidney injury (AKI) in critically ill pediatric patients. There is limited data on the risk of chronic kidney disease (CKD) after discharge in this population.
Methods
This is a single-center, retrospective cohort study of all pediatric patients ages 0–17 years who received CKRT from 2013 to 2017. The study excluded patients with pre-existing CKD, those who died prior to discharge, and those who had insufficient follow-up data. Patients were followed after hospital discharge and electronic health record data was collected and analyzed to assess for incidence of and risk factors for kidney sequelae.
Results
A total of 42 patients were followed at a median time of 27 months (IQR 17.2, 39.8). Of these, 26.2% had evidence of CKD and 19% were at risk for CKD. Lower eGFR at hospital discharge was associated with increased odds of kidney sequelae (aOR 0.985; 95% CI 0.972, 0.996). Ages 0– < 1 and 12–17 were not significantly different (aOR 0.235, 95% CI 0.024, 1.718) and had the highest incidence of kidney sequelae (50% and 77%, respectively). Ages 1–5 and 6–11 had a decreased odds of kidney sequelae compared to the 12–17 year age group (aOR 0.098; 95% CI 0.009, 0.703 and aOR 0.035; 95% CI 0.001, 0.39, respectively). Only 54.8% of patients (n = 23) were seen in the nephrology clinic after discharge.
Conclusions
Patients who receive CKRT for AKI have a significant risk of CKD, while follow-up with a pediatric nephrologist in these high-risk patients is sub-optimal.
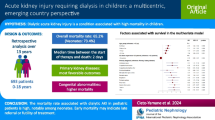
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information





Similar content being viewed by others

Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Analyses were performed using R version 4.1.0 within RStudio version 1.4.1717. R Core Team (2021). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/.
References
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, AWARE Investigators (2016) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20. https://doi.org/10.1056/NEJMoa1611391
Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, Chishti AS, Woroniecki R, Mammen C, Swanson JR, Sridhar S, Wong CS, Kupferman JC, Griffin RL, Askenazi DJ, Neonatal kidney collaborative (NKC) (2017) incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health 1:184–194. https://doi.org/10.1016/S2352-4642(17)30069-X
Madsen NL, Goldstein SL, Frøslev T, Christiansen CF, Olsen M (2017) Cardiac surgery in patients with congenital heart disease is associated with acute kidney injury and the risk of chronic kidney disease. Kidney Int 92:751–756. https://doi.org/10.1016/j.kint.2017.02.021
Uber AM, Sutherland SM (2020) Acute kidney injury in hospitalized children: consequences and outcomes. Pediatr Nephrol 35:213–220. https://doi.org/10.1007/s00467-018-4128-7
Sawhney S, Marks A, Fluck N, Levin A, McLernon D, Prescott G, Black C (2017) Post-discharge kidney function is associated with subsequent ten-year renal progression risk among survivors of acute kidney injury. Kidney Int 92:440–452. https://doi.org/10.1016/j.kint.2017.02.019
Hessey E, Morissette G, Lacroix J, Perreault S, Samuel S, Dorais M, Phan V, Jouvet P, Lafrance JP, LeLorier J, Palijan A, Pizzi M, Roy L, Zappitelli M (2018) Healthcare utilization after acute kidney injury in the pediatric intensive care unit. Clin J Am Soc Nephrol 13:685–692. https://doi.org/10.2215/CJN.09350817
Stads S, Fortrie G, van Bommel J, Zietse R, Betjes MG (2013) Impaired kidney function at hospital discharge and long-term renal and overall survival in patients who received CRRT. Clin J Am Soc Nephrol 8:1284–1291. https://doi.org/10.2215/CJN.06650712
Menon S, Kirkendall ES, Nguyen H, Goldstein SL (2014) Acute kidney injury associated with high nephrotoxic medication exposure leads to chronic kidney disease after 6 months. J Pediatr 165:522–527. https://doi.org/10.1016/j.jpeds.2014.04.058
Mammen C, Al Abbas A, Skippen P, Nadel H, Levine D, Collet JP, Matsell D (2012) Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am J Kidney Dis 59:523–530. https://doi.org/10.1053/j.ajkd.2011.10.048
Askenazi DJ, Feig DI, Graham NM, Hui-Stickle S, Goldstein SL (2006) 3–5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int 69:184–189. https://doi.org/10.1038/sj.ki.5000032
Greenberg JH, Zappitelli M, Devarajan P, Thiessen-Philbrook HR, Krawczeski C, Li S, Garg AX, Coca S, Parikh CR, TRIBE-AKI Consortium (2016) Kidney outcomes 5 years after pediatric cardiac surgery: the TRIBE-AKI study. JAMA Pediatr 170:1071–1078. https://doi.org/10.1001/jamapediatrics.2016.1532
Sutherland SM, Goldstein SL, Alexander SR (2014) The prospective pediatric continuous renal replacement therapy (ppCRRT) registry: a critical appraisal. Pediatr Nephrol 29:2069–2076. https://doi.org/10.1007/s00467-013-2594-5
Chawla LS, Amdur RL, Amodeo S, Kimmel PL, Palant CE (2011) The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int 79:1361–1369. https://doi.org/10.1038/ki.2011.42
Holmes J, Roberts G, May K, Tyerman K, Geen J, Williams JD, Phillips AO, Welsh AKI Steering Group (2017) The incidence of pediatric acute kidney injury is increased when identified by a change in a creatinine-based electronic alert. Kidney Int 92:432–439. https://doi.org/10.1016/j.kint.2017.03.009
Schwartz GJ, Work DF (2009) Measurement and estimation of GFR in children and adolescents. Clin J Am Soc Nephrol 4:1832–1843. https://doi.org/10.2215/CJN.01640309
Zappitelli M, Parikh CR, Akcan-Arikan A, Washburn KK, Moffett BS, Goldstein SL (2008) Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin J Am Soc Nephrol 3:948–954. https://doi.org/10.2215/CJN.05431207
Lo LJ, Go AS, Chertow GM, McCulloch CE, Fan D, Ordoñez JD, Hsu CY (2009) Dialysis-requiring acute renal failure increases the risk of progressive chronic kidney disease. Kidney Int 7:893–899. https://doi.org/10.1038/ki.2009.289
Basu B, Mahapatra TK, Roy B, Schaefer F (2016) Efficacy and outcomes of continuous peritoneal dialysis versus daily intermittent hemodialysis in pediatric acute kidney injury. Pediatr Nephrol 3:1681–1689. https://doi.org/10.1007/s00467-016-3412-7
Author information
Authors and Affiliations
Contributions
Conceptualization: JF, DN; methodology: JF, DN; data curation: MK, DN; investigation: JF; formal analysis and validation: JA; writing — original draft preparation: JF; writing — review and editing: JF, DN, MB, MK, JA; supervision: DN.
Corresponding author
Ethics declarations
Ethics approval
This study was approved as exempt status by the Ann & Robert H. Lurie Children’s Hospital of Chicago Institutional Review Board (IRB 2019–2746) due to the research study posing minimal risk to study participants and involving only information collection and analysis of identifiable health information when that use is regulated under the HIPAA Privacy Rule for the purposes of “health care operations” or “research.” The study was conducted in accordance with the Declaration of Helsinki.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Frisby-Zedan, J., Barhight, M.F., Keswani, M. et al. Long-term kidney outcomes in children following continuous kidney replacement therapy. Pediatr Nephrol 38, 565–572 (2023). https://doi.org/10.1007/s00467-022-05579-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05579-1