Abstract
Growth retardation is a major feature of chronic kidney disease (CKD) of onset in infants or children and is associated with increased morbidity and mortality. Several factors have been shown to play a causal role in the growth impairment of CKD. All these factors interfere with growth by disturbing the normal physiology of the growth plate of long bones. To facilitate the understanding of the pathogenesis of growth impairment in CKD, this review discusses cellular and molecular alterations of the growth plate during uremia, including structural and dynamic changes of chondrocytes, alterations in their process of maturation and hypertrophy, and disturbances in the growth hormone signaling pathway.



Similar content being viewed by others
References
Benyi E, Sävendahl L (2017) The physiology of childhood growth: hormonal regulation. Horm Res Paediatr 88:6–14
Karlberg J (1989) A biologically-oriented mathematical model (ICP) for human growth. Acta Paediatr Scand Suppl 350:70–94
Mehta A, Hindmarsh PC, Stanhope RG, Turton JP, Cole TJ, Preece MA, Dattani MT (2005) The role of growth hormone in determining birth size and early postnatal growth, using congenital growth hormone deficiency (GHD) as a model. Clin Endocrinol 63:223–231
Hindmarsh PC, Smith PJ, Brook CGD, Matthews DR (1987) The relationship between height velocity and growth hormone secretion in short prepubertal children. Clin Endocrinol 27:581–591
Granados A, Gebremariam A, Lee JM (2015) Relationship between timing of peak height velocity and pubertal staging in boys and girls. J Clin Res Pediatr Endocrinol 7:235–237
Abbassi V (1998) Growth and normal puberty. Pediatrics 102:507–511
Roselló-Díez A, Joyner AL (2015) Regulation of long bone growth in vertebrates; it is time to catch-up. Endocr Rev 36:646–680
Kronenberg H (2003) Developmental regulation of the growth plate. Nature 423:332–336
Abad V, Meyers JL, Weise M, Gafni RI, Barnes KM, Nilsson O, Bacher JD, Baron J (2002) The role of the resting zone in growth plate chondrogenesis. Endocrinology 143:1851–1857
Buckwalter JA, Mower D, Ungar R, Schaeffer J, Ginsberg B (1986) Morphometric analysis of chondrocyte hypertrophy. J Bone Joint Surg Am 68:243–255
Hunziker EB (1994) Mechanism of longitudinal bone growth and its regulation by growth plate chondrocytes. Microsc Res Tech 28:505–519
Hunziker EB, Schenk RK (1989) Physiological mechanisms adopted by chondrocytes in regulating longitudinal bone growth in rats. J Physiol 414:55–71
Wilsman NJ, Farnum CE, Leiferman EM, Fry M, Barreto C (1996) Differential growth by growth plates as a function of multiple parameters of chondrocytic kinetics. J Orthop Res 14:927–936
Breur GJ, VanEnkevort BA, Farnum CE, Wilsman NJ (1991) Linear relationship between the volume of hypertrophic chondrocytes and the rate of longitudinal bone growth in growth plates. J Orthop Res 9:348–359
Kember N (1993) Cell kinetics and the control of bone growth. Acta Paediatr 391:61–65
Van Der Eerden BCJ, Karperien M, Wit JM (2003) Systemic and local regulation of the growth plate. Endocr Rev 24:782–801
Wajnrajch MP, Gertner JM, Harbison MD, Chua SC Jr, Leibel RL (1996) Nonsense mutation in the human growth hormone-releasing hormone receptor causes growth failure analogous to the little (lit) mouse. Nat Genet 12:88–90
Wagner JK, Eble A, Hindmarsh PC, Mullis PE (1998) Prevalence of human GH-1 gene alterations in patients with isolated growth hormone deficiency. Pediatr Res 43:105–110
Franke D, Winkel S, Gellermann J, Querfeld U, Pape L, Ehrich JH, Haffner D, Pavičić L, Zivičnjak MI (2013) Growth and maturation improvement in children on renal replacement therapy over the past 20 years. Pediatr Nephrol 28:2043–2051
Harambat J, Bonthuis M, van Stralen KJ, Ariceta G, Battelino N, Bjerre A, Jahnukainen T, Leroy V, Reusz G, Sandes AR, Sinha MD, Groothoff JW, Combe C, Jager KJ, Verrina E, Schaefer F, Registry ESPN/ERA-EDTA (2014) Adult height in patients with advanced CKD requiring renal replacement therapy during childhood. Clin J Am Soc Nephrol 9:92–99
Furth SL, Stablein D, Fine RN, Powe NR, Fivush BA (2002) Adverse clinical outcomes associated with short stature at dialysis initiation: a report of the North American Pediatric Renal Transplant Cooperative Study. Pediatrics 109:909–913
Schaefer F, Seidel C, Binding A, Gasser T, Largo RH, Prader A, Schärer K (1990) Pubertal growth in chronic renal failure. Pediatr Res 28:5–10
Harambat J, Cochat P (2009) Growth after renal transplantation. Pediatr Nephrol 24:1297–1306
Rees L, Jones H (2013) Nutrition and growth in children with chronic kidney disease. Pediatr Nephrol 28:527–536
Fine RN (2010) Etiology and treatment of growth retardation in children with chronic kidney disease and end-stage renal disease: a historical perspective. Pediatr Nephrol 25:725–732
Mehls O, Ritz E, Krempien B, Gilli G, Link K, Willich E, Schärer K (1975) Slipped epiphyses in renal osteodystrophy. Arch Dis Child 50:545–554
Claramunt D, Gil-Peña H, Fuente R, García-López E, Loredo V, Hernández-Frías O, Ordoñez FA, Rodríguez-Suárez J, Santos F (2015) Chronic kidney disease induced by adenine: a suitable model of growth retardation in uremia. Am J Physiol Renal Physiol 309:F57–F62
Claramunt D, Gil-Peña H, Fuente R, Hernández-Frías O, Santos F (2015) Animal models of pediatric chronic kidney disease. Is adenine intake an appropriate model? Nefrologia 35:517–522
Mehls O, Ritz E, Gilli G, Schmidt-Gayk H, Krempien B, Kourist B, Wesch H, Prager P (1977) Skeletal changes and growth in experimental uremia. Nephron 18:288–300
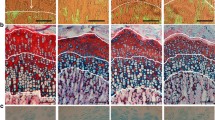
Cobo A, Carbajo E, Santos F, García E, López JM (1996) Morphometry of uremic rat growth plate. Miner Electrolyte Metab 22:192–195
Cobo A, López JM, Carbajo E, Santos F, Alvarez J, Fernández M, Weruaga A (1999) Growth plate cartilage formation and resorption are differentially depressed in growth retarded uremic rats. J Am Soc Nephrol 10:971–979
Fernández-Fuente M, Santos F, Carbajo-Pérez E, Rodríguez J, Weruaga A, Amil B, Molinos I, García E (2004) Growth plate height of uremic rats is influenced by severity and duration of renal failure. Pediatr Nephrol 19:187–192
Alvarez J, Balbín M, Fernández M, López JM (2001) Collagen metabolism is markedly altered in the hypertrophic cartilage of growth plates from rats with growth impairment secondary to chronic renal failure. J Bone Miner Res 16:511–524
Sanchez CP, Salusky IB, Kuizon BD, Abdella P, Jüppner H, Goodman WG (1998) Growth of long bones in renal failure: roles of hyperparathyroidism, growth hormone and calcitriol. Kidney Int 54:1879–1887
Sanchez CP, He YZ (2004) Growth hormone therapy in calcium-loaded rats with renal failure. Endocrinology 145:3375–3385
Sanchez CP, zhu HY (2003) Effects of thyroparathyroidectomy, exogenous calcium, and short-term calcitriol therapy on the growth plate in renal failure. J Am Soc Nephrol 14:148–158
Santos F, Carbajo-Pérez E, Rodríguez J, Fernández-Fuente M, Molinos I, Amil B, García E (2005) Alterations of the growth plate in chronic renal failure. Pediatr Nephrol 20:330–334
Bush PG, Pritchard M, Loqman MY, Damron TA, Hall AC (2010) A key role for membrane transporter NKCC1 in mediating chondrocyte volume increase in the mammalian growth plate. J Bone Miner Res 25:1594–1603
Claramunt D, Gil-Peña H, Fuente R, García-López E, Frías OH, Ordoñez FA, Rodríguez-Suárez J, Santos F (2017) Effects of growth hormone treatment on growth plate, bone and mineral metabolism of young rats with uremia induced by adenine. Pediatr Res 82:888
Mehls O, Irzynjec T, Ritz E, Eden S, Kovàcs G, Klaus G, Floege J, Mall G (1993) Effects of rhGH and rhIGF-1 on renal growth and morphology. Kidney Int 44:1251–1258
Haffner D, Schaefer F, Nissel R, , Wühl E, Tönshoff B, Mehls O; German Study Group for Growth Hormone Treatment in Chronic Renal Failure (2000) Effect of growth hormone treatment on the adult height of children with chronic renal failure. N Engl J Med 343:923–930
Amil B, Fernández-Fuente M, Santos F, Rodríguez J, Díaz-Tejón L, García E, Carbajo E (2003) Efecto de la hormona de crecimiento y del calcitriol sobre la placa de crecimiento de ratas urémicas. Nefrología Suppl 2:23–26
Hunziker EB, Wagner J, Zapf J (1994) Differential effects of insulin-like growth factor I and growth hormone on developmental stages of rat growth plate chondrocytes in vivo. J Clin Invest 93:1078–1086
Darnell JE (1997) STATs and gene regulation. Science 277:1630–1635
Woelfle J, Chia DJ, Rotwein P (2003) Mechanisms of growth hormone (GH) action: identification of conserved Stat5 binding sites that mediate GH-induced insulin-like growth factor-I gene activation. J Biol Chem 278:51261–51266
Woelfle J, Billiard J, Rotwein P (2003) Acute control of insulin-like growth factor-I gene transcription by growth hormone through Stat5b. J Biol Chem 278:22696–22702
Kofoed EM, Hwa V, Little B, Woods KA, Buckway CK, Tsubaki J, Pratt KL, Bezrodnik L, Jasper H, Tepper A, Heinrich JJ, Rosenfeld RG (2003) Growth hormone insensitivity associated with a STAT5b mutation. N Engl J Med 349:1139–1147
Yasukawa H, Sasaki A, Yoshimura A (2000) Negative regulation of cytokine singaling pathways. Annu Rev Immunol 2:143–164
Edmondson SR, Baker NL, Oh J, Kovacs G, Werther GA, Mehls O (2000) Growth hormone receptor abundance in tibial growth plates of uremic rats: GH/IGF-I treatment. Kidney Int 58:62–70
Hanna JD, Santos F, Foreman JW, Chan JC, Han VK (1995) Insulin-like growth factor-I gene expression in the tibial epiphyseal growth plate of growth hormone-treated uremic rats. Kidney Int 47:1374–1382
Schaefer F, Chen Y, Tsao T, Nouri P, Rabkin R (2001) Impaired JAK-STAT signal transduction contributes to growth hormone resistance in chronic uremia. J Clin Invest 108:467–475
Troib A, Landau D, Kachko L, Rabkin R, Segev Y (2013) Epiphyseal growth plate growth hormone receptor signaling is decreased in chronic kidney disease-related growth retardation. Kidney Int 84:940–949
Woelfle J, Rotwein P (2004) In vivo regulation of growth hormone-stimulated gene transcription by STAT5b. Am J Physiol Endocrinol Metab 286:E393–E401
Sun DF, Zheng Z, Tummala P, Oh J, Schaefer F, Rabkin R (2004) Chronic uremia attenuates growth hormone – induced signal transduction in skeletal muscle. J Am Soc Nephrol 15:2630–2636
Rabkin R, Sun DF, Chen Y, Tan J, Schaefer F (2005) Growth hormone resistance in uremia, a role for impaired JAK/STAT signaling. Pediatr Nephrol 20:313–318
Yoshimura A, Nishinakamura H, Matsumura Y, Hanada T (2005) Negative regulation of cytokine signaling and immune responses by SOCS proteins. Arthritis Res Ther 7:100–110
Wiezel D, Assadi MH, Landau D, Troib A, Kachko L, Rabkin R, Segev Y (2014) Impaired renal growth hormone JAK/STAT5 signaling in chronic kidney disease. Nephrol Dial Transplant 29:791–799
Tönshoff B, Kiepe D, Ciarmatori S (2005) Growth hormone/insulin-like growth factor system in children with chronic renal failure. Pediatr Nephrol 20:279–289
Acknowledgments
This work was supported by the National Plan I+D+I 2013-2016 Instituto de Salud Carlos III (PI15/02122), European Regional Development Funds 2013-2016 (ERDF, Grupín 14-020), and by the Foundation of the University of Oviedo (FUO).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Multiple choice answers: 1a, 2b, 3d, 4d, 5c
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fernández-Iglesias, Á., López, J.M. & Santos, F. Growth plate alterations in chronic kidney disease. Pediatr Nephrol 35, 367–374 (2020). https://doi.org/10.1007/s00467-018-4160-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-4160-7