Abstract
Background
Malignant Distal Biliary Obstruction (MBDO) is a common event occurring along the natural history of both pancreatic cancer and cholangiocarcinoma. Epidemiological and biological features make MBDO one of the key elements of the clinical management of patients suffering for of pancreatic cancer or cholangiocarcinoma. The development of dedicated biliary lumen-apposing metal stents (LAMS) is changing the clinical work up of patients with MBDO. i-EUS is an Italian network of clinicians and scientists with a special interest in biliopancreatic endoscopy, EUS in particular.
Methods
The scientific methodology was chosen in line with international guidance and in a fashion similar to those applied by broader scientific associations. PICO questions were elaborated and subsequently voted by a broad panel of experts within a simplified Delphi process.
Results and conclusions
The manuscripts describes the results of a consensus conference organized by i-EUS with the aim of providing an evidence based-guidance for the appropriate use of the techniques in patients with MBDO.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Malignant Distal Biliary Obstruction (MBDO) is a common event occurring along the natural history of both pancreatic cancer and cholangiocarcinoma. Pancreatic cancer is a leading cause of death in particular in western countries, is global burden, and is rising over time, having doubled in the last two decades [1]. Cholangiocarcinoma is a rare and heterogeneous disease; its incidence and mortality rates have increased globally (0.3–6 cases per 100,000 inhabitants yearly in Western countries, and > 6 cases in some East Asian regions) over the past 20 years [2]. In addition to a similar epidemiological trend, pancreatic cancer and cholangiocarcinoma share aggressive biological features and high mortality rates.
Epidemiological and biological features make MBDO one of the key elements of the clinical management of patients suffering for pancreatic cancer or cholangiocarcinoma. Biliary drainage is determinant for the administration of oncological therapy and has a direct effect on patients’ quality of life [3]. The current gold standard technique to achieve biliary drainage is the transpapillary route by retrograde cholangiopancreatography (ERCP), with an alternative in Percutaneous Bile duct drainage (PTBD) in case of failure.
The development of dedicated biliary lumen-apposing metal stents (LAMS) is changing the clinical work-up of patients with MBDO. The use of LAMS simplifies the establishment of a choledochoduodenal anastomosis by Endoscopic Ultrasonography (EUS); its promising results convey the potential for a greater clinical application [3].
i-EUS is an Italian network of clinicians and scientists with a special interest in biliopancreatic endoscopy, EUS in particular. In the current phase of initial dissemination of application of EUS to the management of MBDO, i-EUS thought to organize a consensus conference with the aim of providing an evidence-based guidance for the appropriate use of the techniques that are being developed. In particular, the experts reviewed the current evidence on four main aspects of the clinical management of MBDO, to answer the following questions: (i) which are the indications to biliary drainage? (ii) which is the best approach to EUS-guided biliary drainage? (iii) how to manage specific challenges? (iv) how to take care of and follow up patients?
Methods
The scientific methodology was chosen in line with international guidance and in a fashion similar to those applied by broader scientific associations [4], with pre-defined changes for the method to be applicable to the current set.
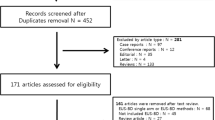
The process involved identification of a number of key questions pertinent to the subject matter. The expert panel drafted questions according to the PICO format (P—patient, problem or population, I—intervention, C—comparison, control or comparator, O—outcome). i-EUS identified 20 experts divided in 4 work groups who defined the PICO questions and discussed in three virtual meetings for approval. This was followed by a systematic literature review process, for statement definition and grading of the evidence. Search terms and results can be found in the supplementary information. The level of evidence was graded according to the Oxford Centre for Evidence-Based Medicine (OCEBM) system (Table 1) and the strength of the recommendations was categorized as either ‘weak’ or ‘strong’ (Table 2) [4]. The higher the quality of the evidence, the more likely a strong recommendation was made. If no clear evidence was available, recommendations were based on the expert opinion of the panel members. A simplified Delphi process followed: statements and evidences were presented in a dedicated, in-person plenary session (Palermo, Italy, May 2023), where results were discussed by a total of 61 experts (gastroenterologists/endoscopists, radiologists, surgeons). Experts were then called to vote for approval of final statements; a pre-defined cut off of 80% of consensus was considered valid for statement approval. The consensus reached for each PICO question is reported in Table 3.
WHICH ARE THE INDICATIONS TO BILIARY DRAINAGE?
CLINICAL QUESTION #1
Can Endoscopic ultrasound biliary drainage (EUS-BD) be considered as first option for biliary drainage of malignant distal biliary obstruction?
Statement #1
i-EUS group suggests EUS choledocho-duodenostomy (EUS-CDS) as an alternative to ERCP as first attempt for biliary drainage in patients with unresectable distal malignant biliary obstruction.
(Level of evidence: 2, grade of recommendation: strong)
Summary of evidence
ERCP is currently considered the first-line approach to obtain adequate biliary drainage. EUS-BD has been developed in the last two decades to perform a direct communication between the biliary tree and the gastroduodenal lumen when ERCP fails or is not feasible. EUS-BD could be performed with different techniques, the two more relevant are CDS connecting the common bile duct and the duodenal lumen, and hepaticogastrostomy (HGS) connecting the left intrahepatic segments and the gastric lumen. Both CDS and HGS have demonstrated high technical feasibility, clinical success, and safety after failed ERCP.
Four Randomized Controlled Trials (RCT) have evaluated the efficacy and safety of EUS-BD as a primary treatment in patients with distal malignant biliary obstruction (DMBO) compared to ERCP [5,6,7,8]. EUS-BD was performed via CDS in all but one the studies where HGS was used in 50% of patients allocated in the EUS-BD arm [6].
In three RCT [6,7,8], only patients with unresectable DMBO were included, whereas in the study by Bang et al., a minority of resectable patients were also included [5]. In the first three RCTs, EUS-BD was performed using a self-expandable metal stent (SEMS). Differently, in the RCT by Teoh et al., hot-LAMS were used. All the four RCT showed similar results between EUS-BD and ERCP in terms of technical and clinical success and safety. In the last study by Teoh et al. technical success was higher in the EUS-BD group (96.2% vs 76.3%, p < 0.001) but it should be noted that technical failure in the ERCP group was related to duodenal obstruction in 7 patients [8]. Comparable efficacy and safety of EUS-BD and ERCP were confirmed in different meta-analysis [9, 10]. In a more recent RCT, EUS-CDS with (hot) LAMS demonstrated to be noninferior to ERCP in terms of technical success (90.4% vs 83.1%) with comparable stent dysfunction rate at 1 year (9.6% vs 9.9%), safety (adverse events rate of 12.3% vs 12.7%), and initial clinical success (84.9% vs 85.9%) [11].
CLINICAL QUESTION #2
Is biliary drainage indicated in patients with resectable malignant distal biliary obstruction?
Statement #2a
i-EUS group recommends against routine preoperative biliary drainage in patients with resectable malignant distal biliary obstruction.
(Level of evidence: 1, grade of recommendation: strong)
Statement #2b
i-EUS group recommends preoperative biliary drainage in patients with cholangitis, severe jaundice, in those planned for neoadjuvant therapy, and when a delay in surgery is anticipate.
(Level of evidence: 1, grade of recommendation: strong)
Summary of evidence
Persistent cholestasis due to distal malignant biliary obstruction (DMBO) is associated with post-surgical complications, including anastomotic leaks and poor wound healing. On this basis, preoperative biliary drainage (PBD) has been used to reduce surgical morbidity and mortality in patients with jaundice undergoing pancreaticoduodenectomy for DMBO. However, conflicting data about the usefulness of PBD have been reported. In 2010, a multicenter RCT provided additional data on this topic [12]. A total of 202 patients with resectable pancreatic head cancer were randomized to early surgery within 1 week without PBD or to ERCP with PBD and delayed surgery 4–6 weeks later. The rate of cumulative post-surgical serious complication was significantly higher in the PBD group (mostly due to the PDB procedure, as cholangitis or stent occlusion) compared to the early surgery group (39% vs. 74%, p < 0.001) with a relative risk of complications after early surgery of 0.54 (95% CI 0.41–0.71). Mortality and length of hospital stay did not differ significantly between the two groups.
Multiple meta-analyses, including retrospective and prospective studies and RCTs, assessed the potential benefit of PBD in patients with distal MDBO. None of them found differences in terms of mortality. In terms of morbidity, only one meta-analysis [13] reported a lower rate of serious adverse events in patients who underwent PBD, whereas other meta-analyses found similar [14, 15] or higher [16, 17] morbidity in patients with PBD vs those without PBD, with regard to infection and cholangitis rates. Consequently, European guidelines did not recommend PBD in all patients with MDBO [18].
However, specific settings of patients requiring PBD were identified, such as acute cholangitis and severe jaundice (with or without symptoms). Indeed, acute cholangitis represents an urgent condition requiring prompt intervention, and severe jaundice was associated with a higher risk of postoperative complications. For this reason, bilirubin levels > 15 mg/dl are considered an indication for PBD, especially when a delay in surgery is anticipated.
Moreover, PBD is required in patients with obstructive jaundice planned to receive neoadjuvant chemotherapy and could be indicated to improve alterations in coagulation and fibrinolysis related to jaundice.
CLINICAL QUESTION #3
How biliary drainage should be performed in non-surgical candidate patients with malignant distal biliary obstruction when ERCP fails?
Statement #3
i-EUS group recommends EUS-guided choledochoduodenostomy (EUS-CDS) over PTBD after failed ERCP in malignant unresectable MBDO.
(Level of evidence: 2, grade of recommendation: strong)
Summary of evidence
Difficult biliary cannulation during ERCP (which accounts for up to 10%) is associated with a higher risk of ERCP-related complications [5]. PTBD has historically been considered a rescue strategy in case of ERCP failure, despite it is burdened by significant morbidity and complications. Many recent retrospective and prospective studies demonstrated the efficacy (technical and clinical success of 90–98%), and safety (AE rate of 5–23%) of EUS-BD performed with LAMS as a second option after failed ERCP [6, 7].
According to the growing evidence, Asian and European guidelines recommended EUS-BD as the procedure of choice for biliary drainage in patients with failed ERCP [8, 9] when local expertise is available. These recommendations are supported by available evidence coming from 28 retrospective and 8 prospective studies, 4 randomized controlled trials (RCTs), and 8 meta-analyses, which compared EUS-BD and PTBD in patients with MBDO reporting similar technical and clinical success rates for EUS-BD versus percutaneous or surgical treatment, with lower rate of AE and reintervention, even resulting in better cost-effectiveness (Supplementary Table 3). It should be noted that the examined population is not homogeneous throughout studies because it is not always specified if only patients with unresectable diseases were included and, in addition, in most of the studies the subgroup of EUS-BD is characterized by one or more of the different techniques available.
Another option in case of ERCP failure, especially when expertise for EUS-guided techniques is not available or dilation of biliary system is not enough to safely perform it, can be represented by repeating ERCP on a different timing (interval ERCP). This option should be considered mainly if a precut has been performed at the index procedure. Available studies, including benign and malignant indications, examined the benefit of interval ERCP reporting a successful cannulation rate ranging between 68 and 87%, with an AE rate comparable to index ERCP [10, 12, 13]. Also, percutaneous rendezvous technique remains a potential option with a successful cannulation rate of approximately 90% [14].
CLINICAL QUESTION #4
Which type of sedation should be preferred for EUS-BD in malignant distal biliary obstruction?
Statement #4
i-EUS group suggests performing EUS-BD under deep sedation or general anesthesia; the choice between these two options should be based on patient clinical condition and anaesthesiologist preference.
(Level of evidence: 4, grade of recommendation: weak)
Summary of evidence
No studies comparing different sedation/anesthesia strategies for EUS-BD in patients with MBDO have been published. In available studies, EUS-BD (including choledochoduodenostomy and hepaticogastrostomy) has been performed either under conscious sedation, deep sedation, and general anesthesia, with the latter appearing to be the most used [6, 19]. A recent Italian survey on LAMS clinical practice confirmed this variability in sedation preference: general anesthesia was used in 38.8% of the centers involved (14/36), deep sedation in 30.5% (11/36), and conscious sedation in 8.3% (3/36) [20]. This issue has been raised also by the ESGE Technical Review on Therapeutic EUS, which stated that although many centers perform therapeutic EUS exclusively in patients under general anesthesia, other centers use conscious or deep sedation without compromising safety outcomes [21]. Likewise, ERCP biliary drainage can be performed under conscious or deep sedation or general anesthesia, and the choice of type of sedation/anesthesia is often based on local resources and institutional preferences [22]. However, a Dutch study showed that one-third to one-half of patients experienced pain and discomfort during and immediately after ERCP when the procedure is performed under conscious sedation [23]. Similarly, it is likely that conscious sedation can be a burden for the patient undergoing EUS-BD and, therefore, as with ERCP, other forms of deeper sedation should be preferred.
WHICH IS THE BEST APPROACH TO EUS-GUIDED BILIARY DRAINAGE?
CLINICAL QUESTION #5
What’s the best method of EUS-guided biliary drainage in terms of technical and clinical success, safety and long-term patency among patients with malignant distal biliary obstruction after ERCP failure?
Statement #5
i-EUS recommends EUS-choledocoduodenostomy for the treatment of MBDO after ERCP failure. EUS-guided gallbladder drainage (EUS-GBD) and EUS-guided hepaticogastrostomy (EUS-HGS) should be considered in case of unapproachable EUS-CDS.
(Level of evidence 2; Grade of recommendation: strong)
Summary of evidence
EUS-guided BD has been an effective alternative method to PTBD after ERCP failure for DMBO. EUS-guided biliary drainage may include different approaches, as choledocoduodenostomy (CDS), hepaticogastrostomy (HGS), antegrade stenting, rendezvous or even gallbladder drainage, but strong outcomes comparisons are still lacking in the literature in the setting of patients with MBDO after ERCP failure. Recently, a network meta-analysis including 5 RCTs (217 patients) evaluated those methods for BD of MBDO after ERCP failure in terms of technical success, clinical success, and postprocedure adverse events. In this study, EUS-BD included EUS-CDS and EUS-HGS, which showed no significant differences when compared each other (EUS-HGS vs EUS-CDS: clinical success RR 1.01, 95% CI 0.87–1.17; technical success RR 1.01, 95% CI 0.93–1.09; adverse event rate RR 0.85, 95% CI 0.39–1.82) [24]. Our literature search analyzed 28 studies. The majority of studies were retrospective (n = 18, 62%, Table 1), while other studies included four trials (Supplementary Table 5) [25,26,27,28] and six prospective studies (Table 3). Fifteen studies were multi-center (53.6%). However, there was no direct efficacy and safety comparison among EUS-BD procedures, even if eight studies included two or more different EUS-guided BD procedures. Pooled technical and clinical success of EUS-BD was over 95% when considering all of the approaches, with a low heterogeneity among studies even if not statistically significant (TS, I2 = 5.03%, p = 0.379; CS, I2 = 25.38%, p = 0.083). Pooled technical success for EUS-CDS and EUS-HGS was, respectively, 95.5% and 94.7%, while clinical success was 96.5% and 90.9%, respectively. Furthermore, EUS-GBD after ERCP failure was used when EUS-CDS was unapproachable among the included studies, showing a pooled technical and clinical success of 97.7% and 92.4%, respectively. In this setting of patients, EUS-guided rendezvous (EUS-RV) was used in two studies (n = 15 patients) showing 100% of clinical and technical success, while the EUS-guided antegrade (EUS-AG) approach was used for 40 patients (two studies) with a technical success of 97.4% (n = 38) and 100% (n = 2), but clinical success (100%, 2 out of 2 patients) was reported only in one study. Moreover, EUS-CDS showed better safety compared to EUS-HGS and EUS-GBD (CDS 10.3% vs HGS 16.8% vs GBD 15.5%). However, some study also showed data on patency, with overall mean patency rate of 69.4% (± 24.98) during the period of follow-up.
CLINICAL QUESTION #6
Could EUS-GBD be considered as a rescue strategy in patients with malignant distal biliary obstruction and patent cystic duct when other EUS-BD approaches are not feasible?
Statement #6
i-EUS group states that EUS-guided gallbladder drainage (EUS-GBD) may be considered a rescue strategy for biliary drainage in unresectable patients with MBDO and patent cystic duct when other EUS-BD approaches are not feasible.
(Level of evidence 3; Grade of recommendation: weak)
Summary of evidence
To date, EUS-guided drainages are a valuable alternative in case of failure of ERCP in patients affected by DMBO, usually when are considered unfit for surgery. Although EUS-BD has a high technical success rate and an acceptable risk profile, EUS-BD can fail or may be technically unfeasible for multiple reasons, such as in case of a CBD < 15 mm or altered anatomy. EUS-guided gallbladder drainage (EUS-GBD) is a feasible rescue therapy when ERCP and EUS-BD are unsuccessful or not feasible, which can occur in up to 7% of patients with DMBO. In 2016, Imai et al. reported a series of 12 cases with malignant biliary obstruction who underwent EUS‑GBD after failed ERCP and EUS‑BD [29]. The rational is that the bile produced by the liver, through the cystic duct passed usually goes in the gallbladder and then is again excreted in the bile duct. Therefore, when a DMBO is present, the gallbladder can represent a possible gate for drainage. However, in order to perform an EUS-GBD as rescue treatment, the patency of the cystic duct is often not easy to be assessed and should be carefully evaluated at CT-scan and during EUS examination. To date, 3 case reports and 5 retrospective studies are available with at least 116 patients (see Table 1). In 6 studies, the authors used LAMS for EUS-GBD, while in the remaining, 2 studies SEMS were used.
A recent meta-analysis reported a pooled technical success of 100%, pooled clinical success of 85% and a pooled rate of adverse events of 13%, being stent dysfunction the most common complication [30]. The pooled rate of stent dysfunction was 9%, mainly due to food impaction in the stent complicated by recurrent cholecystitis and to the entrapment of the cystic duct by growing tumor [30]. Three studies report the mean percentage of decrease in bilirubin levels at 14 days with EUS-GBD, which ranges from 62 to 66.5% [5, 9, 10]. In most of the cases, patients were considered unresectable, while only in few cases, a subsequent surgery was performed. Therefore, as evidence are sparse regarding this procedure in the setting of EUS-GBD as a bridge-to-surgery, we suggest to reserve this type of drainage in the setting of unresectable diseases.
CLINICAL QUESTION #7
In patients with malignant distal biliary obstruction undergoing EUS-guided choledochoduodenostomy (EUS-CDS), is there any advantage in the use of either LAMS or SEMS?
Statement #7a
iEUS recommends the use of either self-expandable metal stents (SEMS) or lumen-apposing metal stents (LAMS) for EUS-guided choledochoduodenostomy (EUS-CDS).
(Level of evidence 3; Grade of recommendation: strong)
Statement #7b
iEUS suggests that of electrocautery enhanced LAMS might be preferred in patients with dilated (≥ 15 mm) common bile duct since a slight reduction in pooled incidence of adverse events was observed.
(Level of evidence 3; Grade of recommendation: weak)
Summary of evidence
In terms of comparison of the different stent types for EUS-CDS, a systematic review conducted in 2021 [31] identified 31 studies including 820 patients who underwent EUS-CDS with either SEMS (25 studies; 509 patients) or LAMS (6 studies; 311 patients). The authors did not identify significant difference in terms of technical success rate (92.7% vs. 94.8%), clinical success rate (91.7% vs 93.6%), adverse event rate (18.3% vs. 17.1%), and reintervention rate (13.9% vs. 10.9%).
One retrospective study [32] compared the outcomes of 20 patients who underwent EUS-CDS with SEMS to 37 patients who underwent EUS-CDS with LAMS. The authors reported similar rates of technical success (100% in both groups), clinical success (95% vs. 100%), adverse event (20% vs. 13.5%), and reintervention rate (35% vs. 16.2%). Finally, overall survival was similar in the two groups.
A systematic review updated at the end of April 2023 identified thirty-eight original studies including 1277 patients who underwent EUS-CDS for distal MBO (Supplementary Table 6). The above-mentioned retrospective comparative study on SEMS vs. LAMS, 26 (7 RCTs, 9 prospective and 10 retrospective) studies using SEMS and 12 (1 prospective, 11 retrospective) studies using LAMS. Finally, 570 patients underwent EUS-CDS with SEMS, while 707 with LAMS. Pooled outcomes of EUS-CDS assessed with random effect model are summarized in (Supplementary Table 7).
Overall, the quality of available literature on the comparison between LAMS or SEMS use for EUS-CDS was low or even very-low. No randomized controlled trial designed to compare EUS-CDS with LAMS or SEMS.
CLINICAL QUESTION #8
In patients with distal malignant distal biliary obstruction undergoing EUS-guided choledochoduodenostomy (EUS-CDS), the use of 6 mm LAMS allows advantages over ≥ 8 mm LAMS?
Statement #8
I-EUS does not suggest the use of 6 × 8 mm over 8 × 8 mm LAMS since no advantages has been demonstrated; 6 × 8 mm LAMS could be used in case of small CBD diameter.
(Level of evidence 4; Grade of recommendation: weak)
Summary of evidence
There are several different LAMS systems available at this time with different lengths and diameters.
The major data of the EUS-CDS studies present in literature concern the Hot-Axios system (Boston Scientific, Massachusetts, USA).
In particular, 4 studies report data regarding 6–8 vs 8–8 mm stents. Jacques et al. reported that, on univariate analysis, the use of 6 × 8 mm LAMS (OR 6.67; P = 0.04) was related to an increased technical success [33].
In a prospective study, the same authors enrolled 70 patients and recommend to use a 6–8 mm stent based on their long experience with this stent size, without direct comparison of the impact of stent size on procedural outcomes [34].
In the largest multicentric study present in literature including 256 patients, no statistically significant difference was observed between 6 and 8 mm and 8–8 mm stents in terms of technical success, clinical success, and stent patency (p = 0.661) [19].
However, On et al. [35] in a multicentric retrospective study including 120 patients reported that the overall technical success was similar between patients who had a 6–8 mm and an 8–8 mm stent, but adverse events (OR, 3.71; 95% CI, 1.35–10.19; p = 0.008) and reintervention rates (OR, 6.17; 95% CI, 1.22–31.22; p = 0.019) were higher in those who had a 6-8 mm stent.
CLINICAL QUESTION #9
In patients with malignant distal biliary obstruction undergoing EUS-guided choledochoduodenostomy (EUS-CDS) with LAMS (any size) the use of co-axial double pig-tail plastic stents (DPPS) allows any advantage?
Statement #9
There is no evidence to suggest in favor or against double pig-tail plastic stents (DPPS) placement through the LAMS in patients undergoing EUS-guided choledochoduodenostomy (EUS-CDS). i-EUS states that DPPS placement could be considered in selected cases.
(Level of evidence 4; Grade of recommendation: weak)
Summary of evidence
LAMS obstruction could occur after EUS-CDS by food impaction from 6,7% to 31,8% of cases [19].
Placement of a double pig-tail stent (DPS) into a LAMS for EUS-CDS may be theoretical beneficial in preventing stent occlusion by maintaining patency of the lumen of the LAMS, anchoring the EC-LAMS to prevent migration, and orientating the LAMS in a vertical direction to augment coaxial biliary drainage [35].
In such clinical scenario, it can be considered to place a prophylactic DPPS through the internal lumen of the LAMS at the time of initial deployment.
El Chafic et al. [36] reported the first routine use of the double stent placement technique after placement of a 10–10 mm stent. In their cohort of 67 patients, 50 patients received double stent placement (DPS in 46 patients and Fully Covered SEMSs in 4 patients). Among 40 patients with follow-up of > 4 weeks, a significant reduction in biliary reintervention rates was observed in patients with double stent placement (5% vs 50%, p = 0 0.02).
In the multicenter retrospective study of On et al. [35], 32 patients placed DPPS into the LAMS. In this group of patients compared with patients who had only a LAMS were observed lower biliary reintervention (0% vs 12.2%, p = 0.03).
Non-statistically difference was encountered in the rate of cholangitis (6.3% vs 12.2%, p = 0.3).
Garcia-Sumalla et al. [37] published the first study assessing the hypothetical benefit of a DPS through a LAMS in EUS-CDS. In this retrospective study, 29 patients were included (22 LAMS alone vs 17 LAMS plus DPS). No differences between the groups in terms of clinical success (77.3 vs 87.5%, p = 0.67), adverse events (AEs, 13.6 vs 11.8%, p = 0.99), recurrent biliary obstruction (13.6 vs 23.5%, p = 0.67), or survival rate (p = 0.67) were encountered. The only difference was the procedural time: the LAMS alone group had a shorter length of procedure in comparison of the DPS group (50 min vs 66 min, p = 0.102). The authors conclude that a DPS inserted through a LAMS for EUS-CDS seems not to offer enough benefits over a LAMS alone, and it is a time-consuming approach. These results do not support this approach being used routinely.
CLINICAL QUESTION #10
In patients undergoing EUS-guided hepaticogastrostomy (EUS-HGS) for malignant distal biliary obstruction, the use of dedicated stents (partially covered stents with uncovered distal portion, covered proximal portion, anti-migration flange/flap) allows any advantage over the use of other stents (fully covered SEMS, uncovered SEMS with a fully covered SEMS inside, DPPS)?
Statement #10
i-EUS suggests the use of dedicated stents in patients undergoing EUS-guided hepaticogastrostomy (EUS-HGS) for MBDO.
(Level of evidence 5, Grade of recommendation: open)
Summary of evidence
EUS-HGS is characterized by a high technical complexity, that requires high technical skills both in ERCP and in interventional endoscopy, and not negligible rate of adverse events, often severe and requiring additional modalities (e.g., interventional radiology or surgery). Moreover, for a long time, no dedicated devices were available, with the employment mainly of plastic stents (PS), partially and fully covered self-expandable metal stents (SEMS). In the last years, different type of stent has been designed for this procedure, to make this procedure safer and to overcome the limitations of the previously available devices.
These stents are SEMS with a longer portion fully covered and uncovered extremity for the intra-hepatic side, and provided of variable anti-migrating systems both on the intra-hepatic side and the intra-gastric one [25, 38]. Therefore, these devices could potentially reduce the risk of both proximal and distal stent migration, biliary leakage, and intra-hepatic bile duct obstruction. There are no studies which directly compared the use of dedicated stents to non-dedicated ones. Standing to available literature, EUS-HGS outcomes varied widely among studies: technical success varies from 65 to 100%, clinical success from 76 to 100%, and overall, from 0 to 35% [25, 38,39,40].
To date the use of dedicated stents was reported in 20 studies on EUS-HGS, mainly mixed with non-dedicated stents and only in few cases considered alone. Standing to largest studies considering dedicated stents alone, technical success varies from 90.2 to 100%, clinical success from 83 to 100%, and adverse events from 9 to 25%. Interestingly, when considering the type of complications, transient fever, abscess, and sepsis were the most common adverse events, while no cases of biliary leakage were reported and only two cases of stent migration were described. One of the most severe adverse events after EUS-HGS is the occurrence of stent migration with consequent bile leak into the abdominal cavity. Dedicated stents have been specifically designed to avoid, or at least reduce, the risk of proximal migration, thanks to the presence of an uncovered portion that fixes the stent to the liver parenchyma. On the other hand, to reduce the risk of distal migration, choosing a stent length that guarantees a 2–3 cm margin into the gastric cavity is commonly suggested. While no data are available on the outcomes of EUS-HGS performed with different stent lengths, a recent meta-analysis demonstrated that dedicated stents significantly reduce the incidence of AEs after EUS-HGS (odd ratio 0.62) [41].
Although ESGE guidelines recommend either partially or fully covered SEMS [42], several expert opinions advised for the use of dedicated stents to reduce adverse events, especially stent migration.
HOW TO MANAGE SPECIFIC CHALLENGES?
CLINICAL QUESTION #11
In the setting of malignant gastric outlet obstruction, should EUS-gastroenterostomy (EUS-GE) be preferred over enteral stenting?
Statement #11
i-EUS suggests to prefer EUS-gastroenterostomy (EUS-GE) over Enteral Stenting in patients with malignant Gastric Outlet Obstruction
(Level of evidence 3, Grade of recommendation: weak).
Summary of evidence
Malignant gastric outlet obstruction (GOO) is common in pancreatobiliary and gastroduodenal malignancies, occurring in about 20% of patients [43]. Malignant GOO is thus associated with biliary obstruction (BO) in 40 to 92% of patients [44]. The goal of treatment is to palliate obstructive symptoms and to improve poor performance status that can delay chemotherapy treatment.
In the last decades, enteral stenting (ES) has been preferred over surgical gastroenterostomy as a treatment of GOO, given its noninvasive nature, high technical, clinical success, and safety profile. However, the main drawback of ES is represented by high recurrence rate reaching 56% at 6 months due to stent dysfunction related to ingrowth and overgrowth [45].
EUS-guided gastroenterostomy (EUS-GE) has recently emerged as a valuable alternative to enteral stenting, facilitating the effective reestablishment of the gastrointestinal transit while avoiding recurrences over time. Cohort comparative studies have demonstrated higher clinical success (ranging from 83.3 to 100% vs.67.3–87.7%) and lower recurrence rate (ranging from 1 to 8.8% vs. 26 to 33.3%) of EUS-GE over enteral stenting [11, 21, 46,47,48,49]. Technical success is reported to be the same or slightly inferior for EUS-GE but statistical significance was not reached.
Longer patency of EUS-GE with LAMS compared to ES seems to be related to the avoidance of the tumor tract reflecting a lower need for reintervention and a positive impact on the quality of life of the patient.
Also safety profile seems to be acceptable for EUS-GE with comparable adverse event rate with ES (7.1–16.7% vs. 10.3 vs. 40.2%) that however has been decreasing over time probably reflecting an improvement of the technique together with learning curve progression.
Results have been confirmed by two meta-analysis that reported higher clinical success, fewer severe adverse events, and lower GOO recurrence for EUS-GE [50, 51].
In the published series emerges that EUS-GE should not be performed in patients with significant ascites, peritoneal carcinomatosis, linitis plastica or previous gastric surgery.
It is to be considered that in the abovementioned available comparative studies, different EUS-GE techniques have been described comprising EPASS (EUS-guided balloon-occluded gastrojejunostomy bypass), direct unassisted EUS-GE with the water irrigation technique, direct puncture technique, balloon-assisted or nasobiliary catheter-assisted approach. This may have an impact on heterogeneity of results and the optimal method is yet to be confirmed.
Furthermore, being EUS-GE a technically challenging procedure even for the experienced endoscopist, it should be performed in tertiary care centers where a multidisciplinary expertise is available also to manage eventual adverse events.
Given the above and balancing risks and benefits, enteral stenting may be preferred in patients with a life expectancy less than 3 months.
CLINICAL QUESTION #12
In the setting of concomitant biliary and gastric outlet malignant obstruction, what is the best modality to achieve biliary drainage?
Statement #12a
i-EUS suggests that, in the setting of double obstruction, ERCP may be attempted whenever the papilla is reachable (especially in type 1 or 3 stenosis) or in case of previously placed duodenal stent.
(Level of evidence 4, Grade of recommendation: weak).
Statement #12b
i-EUS suggests that, in naïve patients with double obstruction, EUS-guided double bypass may be considered where adequate expertise is available.
(Level of evidence 4, Grade of recommendation: weak).
Summary of evidence
Management of combined biliary and gastric outlet obstruction is a challenging scenario. A duodenal obstruction can often impede standard ERCP or even reduce the efficacy of a technical successful biliary drainage. In this scenario, management strategies might vary according to the location of the stenosis (above, at or below the papilla) and the sequence of obstruction (biliary first, concomitant, GOO first).
In general, placement of duodenal stents (DS) has been associated with a non-negligible risk of pancreatitis and biliary obstruction, and it is also an independent predictor of dysfunction among patients with a biliary SEMS in place; it has been speculated that this depends not only on a direct interference of the meshes, but also on an increased duodenobiliary reflux due to duodenal invasion and reduced duodenal peristalsis.
On the other hand, when a DS has been already placed, obtaining biliary drainage becomes challenging, due to increased difficulties in traversing the duodenal stent, identifying or accessing the papilla or placing a stent through the meshes. Variable results have been reported regarding successful biliary drainage in retrospective series, ranging between 34 and 93%, with the variability probably reflecting the typical selection bias of retrospective evaluations [52,53,54,55]. However, what is clear is that ERCP underperforms in the setting of duodenal obstruction and indwelled duodenal SEMS, especially in type 2 stenoses involving the papilla [52,53,54,55] EUS-BD is increasingly used as a rescue in this setting, where the only other alternative would be PTBD with its morbidity and mortality [54]. ERCP might maintain optimal outcomes in type 1 or type 3 stenosis (where papilla is accessible), and when previous sphincterotomy or biliary stenting have already been performed [54]. When ERCP has proved unfeasible, EUS-BD might be very helpful. In a recent retrospective study including 39 patients, transmural drainage through EUS-BD demonstrated higher technical success (95% versus 56.0%; p < 0.01) and higher clinical success (91% versus 52.0%; p = 0.01) compared to ERCP with similar invasiveness and similar long-term patency. Moreover, when EUS-BD (EUS-HGS) has been compared to ERCP or PTBD in this setting, a trend toward lower rate of complications and reinterventions for the EUS group has been reported [56].
Series exploring the role of EUS-BD when DS was in place, tried different solutions, as for example through antegrade stenting, LAMS placement through the meshes of ES or EUS-HGS.
Limitations of this evidence are the following: (1) most studies involve retrospective evaluation of outcomes, despite prospective databases; (2) most studies include small cohorts (most EUS-BD cohorts < 10); (3) most studies are non-comparative, showing the efficacy and safety of single combination of procedures; (4) biliary and GO obstruction are often non-contemporary, with biliary management often performed times before GOO onset; (5) different demographical (cancer type), anatomical (location of the stenosis), and technical variables (extrahepatic, either gallbladder or choledochal drainage, versus intrahepatic EUS-BD; covered versus uncovered DS) are not controlled or corrected.
All these limitations emerge also from a recent systematic review on EUS-BD in the setting of double obstruction [57].
So far, literature describing GOO management with DS has been mostly published. However, given the abovementioned advantages of EUS-GE over DS, literature investigating newer procedural combination is awaited.
The first available study managing GOO with EUS-GE in the setting of double obstruction, is a retrospective study describing a series of 23 patients undergoing same session EUS-GE + EUS-HGS. Technical and clinical success were high, with 5 (21%) reported AEs (none severe or fatal) and 3 patients (14%) requiring reinterventions for recurrent or persistent jaundice [58].
A recent retrospective multicentric experience tried to compare different possible endoscopic combinations to treat patients with malignant double obstruction, focusing on recurrence-free survival9. The study included 103 procedure combinations and suggested that combinations using EUS-GE versus DS achieve better long-term outcomes and that either a transpapillary stent (via ERCP or antegrade stenting) or EUS-HGS are associated with decreased symptoms recurrence during follow-up, while EUS-CDS in this setting seems to be associated with reduced primary success and frequent dysfunction, independently from the fact that GOO has been solved by DS or EUS-GE[59].
As patients with concomitant obstruction and unresectable malignancies were historically treated by double-bypass surgery, a recent retrospective multicentric case–control study has suggested that same-session EUS-guided double bypass (EUS-GE + EUS-BD) achieves similar efficacy with reduced invasiveness than surgical double bypass (gastrojejunostomy + hepaticojejunostomy) [60]. This study reported a 94% clinical efficacy, an 11% rate of AEs (3.8% severe), no risk of dysfunction for EUS-GE, and a 7.5% of dysfunction for EUS-BD, suggesting improved outcomes of EUS-guided double bypass in more recent and high-volume experiences.
CLINICAL QUESTION #13
In the setting of Duodenal stenosis, is there any difference between the extrahepatic and intrahepatic access for EUS-guided biliary drainage?
Statement #13
Si-EUS suggests that, in the specific setting of double obstruction, EUS-guided hepaticogastrostomy (EUS-HGS) may be favored over EUS-guided choledochoduodenostomy (EUS-CDS) due to longer stent patency.
(Level of evidence 4, Grade of recommendation: weak).
Summary of evidence
The technical and clinical success rates of EUS-HGS and EUS-CDS are summarized in Supplementary Table 10, in which the results of an umbrella review, including three systematic reviews, are reported [61,62,63]. The umbrella review suggested that clinical and technical success and adverse events are similar between the two approaches. However, the populations of these systematic reviews also included patients without double obstruction, increasing the risk of bias. Some small multicenter studies [59, 64] showed that EUS-HGS may be favored over EUS-CDS due to longer stent patency.
CLINICAL QUESTION #14
Does potential surgical resectability represent a contraindication to EUS-guided biliary drainage? Which biliary drainage should be performed in patients with resectable malignant distal biliary obstruction?
Statement #14
i-EUS suggests either ERCP or EUS-guided choledochoduodenostomy (EUS-CDS) as the first-line treatment of resectable MBDO.
(Level of evidence 4, Grade of recommendation: weak).
Summary of evidence
The technical and clinical success rate of EUS-CDS with ECE-LAMS is similar to that of ERCP [5, 65,66,67]. EUS-guided drainage is associated with a lower rate of post-procedural and post-PD complications. The rate of post-procedural complications doubles if drainage follows a failed ERCP attempt, rather than being performed first [65]. A higher rate of overall complications and mild complications than EUS-guided drainage was described by Bang et al. In those cases, however, SEMS was used [5].
CLINICAL QUESTION #15
How does EUS-BD compares with other endoscopic, surgical, or percutaneous approaches in achieving biliary drainage in patients with post-surgical anatomy?
Statement 15a
In patient with MBDO and surgical altered anatomy, treatment choice depends on disease extension and type of reconstruction. i-EUS suggests to consider EUS-BD over laparoscopic-/enteroscopy-assisted ERCP and PTBD in patient with Roux-en-Y anatomy.
(Level of evidence 4, Grade of recommendation: weak).
Statement 15b
i-EUS suggests to consider EUS-BD as a rescue strategy after failed ERCP with lateral-viewing or cap-assisted frontal-viewing endoscopes in patients with Billroth II reconstruction.
(Level of evidence 4, Grade of recommendation: weak).
Summary of evidence
In patients with Billroth II reconstruction and malignant distal biliary stenosis, a lateral-viewed endoscope present similar clinical success rate to cap-assisted frontal-viewed endoscope with higher cannulation rate and lesser PEP rate [68,69,70]. After failed ERCP, EUS-BD (EUS-RV and EUS-anterograde biliary stenting) is preferable over percutaneous transhepatic biliary drainage (PTBD) due to better clinical success and lesser adverse events [71].
In patients with Billroth II or Roux-en-Y partial gastrectomy with distal malignant biliary obstruction in which papilla is not reached, EUS-HGS and or anterograde stent placement can be performed with a higher degree of clinical efficacy and shorter procedure time than enteroscopy-assisted ERCP. Whether or not this approach should be first-line therapy in this patient population is highly dependent on the indication for the procedure, the patient’s anatomy, and local practice and expertise [72,73,74].
In patients with RYGB, EUS-BD, especially Endoscopic Ultrasound-Directed transGastric ERCP (EDGE) procedure showed favorable technical and clinical success, comparable to laparoscopic ERCP, despite less invasive than the latter [75], and higher success rate than enteroscopy-assisted ERCP and PTBD [76]. Since there are no studies [77] regarding SAA and distal malignant obstruction, EDGE can be offered in expert center in Roux-en-Y bypass following multidisciplinary decision-making, according to ESGE guidelines. If EDGE procedure is not feasible, EUS-HGS can be considered. Choice of biliary drainage procedure in patients with SAA depends on surgical procedure performed, expertise, and equipment available at the center, interventional radiology, and surgical back up available.
HOW TO TAKE CARE OF AND FOLLOW UP PATIENTS?
CLINICAL QUESTION #16
Who has to take care of patients requiring biliary drainage? Is multidisciplinary management associated with better outcomes?
Statement #16
I-EUS suggests multidisciplinary discussion of patients with distal malignant obstruction in whom the biliary drainage could impact on the main outcomes, in particular patients with resectable cancer, altered anatomy and double obstruction.
(Level of evidence 5, Grade of recommendation: weak).
Summary of evidence
As concerns patients requiring biliary drainage, there are no data showing which clinician should be responsible for taking care of this specific condition and whether the management in a multidisciplinary team is associated with better outcomes. Moreover, these patients may be suffering from different pathologies, both benign and malignant. Some positive few data are available for oncological setting and especially for pancreatic cancer and cholangiocarcinoma. In this context, it has been proven that patients discussed at multidisciplinary meetings are more likely to receive more accurate diagnosis, staging, and more frequently appropriate treatment [78,79,80,81] (i.e., resectability, neoadjuvant and adjuvant chemotherapy), even if there is no evidence on the specific topic of biliary drainage. Furthermore, in case of malignant hilar biliary obstruction, multidisciplinary consultation to determine the most effective biliary drainage strategy is also recommended by ESGE [21]. Therefore, it seems reasonable to suggest a multidisciplinary discussion certainly when the biliary drainage could impact on the outcomes, as in the cases of resectable cancer, altered anatomy and double obstruction (biliary tree and duodenum). There are no defined criteria for a multidisciplinary team taking care of patients requiring biliary drainage.
CLINICAL QUESTION #17
Does endoscopic biliary drainage need to be performed in a referral setting?
Statement #17
I-EUS suggests endoscopic biliary drainage to be performed in a setting where adequate competencies in interventional bilio-pancreatic management are available.
(Level of evidence 5, Grade of recommendation: weak).
Summary of evidence
Several studies showed higher technical and clinical success rates and lower complication rates when EUS-guided biliary drainage is performed by experienced endoscopists.
A small study [82] including 31 patients showed significantly different procedure failure rate in the first three and last two years of experience (38 vs 11%, respectively). A Spanish survey [83] involving endoscopist with initial experience in biliary drainage showed lower technical success rate than previously reported in more experienced endoscopists. Moreover, a single-center study [84] on 101 patients reported a lower mortality rate among the first fifty patients during the first 5 years than in the last 51 patients during the last 2 years. The execution of at least the first twenty cases under a mentor’s supervision was suggested by Hara et al. [85]. A single operator study [86] aimed at defining the learning curve for EUS-BD showed that endoscopists experienced in EUS-BD are expected to achieve a reduction in procedural time as experience grows, with efficiency reached at 59 min and a learning rate of 32 cases. Another study [87] only focused on EUS-guided hepaticogastrostomy highlighted that the number of procedures to achieve technical proficiency was 24 for reducing and 33 to stabilize for procedural times. A very recent study [88] performed at EUS-BD beginner institutions reported that various experience-related factors (number of EUS-BD conducted by the institution and EUS screening, EUS-FNA, and EUS-guided drainage conducted by the operator, but not the operator’s experience with EUS-BD itself) may affect EUS-BD outcomes, pointing out the importance of the institution-conducted experience more than that of the single operator. However, also ESGE recommends therapeutic EUS procedures should be performed by endoscopists with adequate training and experience, at centers where interventional radiology and hepatopancreaticobiliary surgical expertise are available [21].
CLINICAL QUESTION #18
Is a special diet suggested after biliary drainage?
Statement #18
i-EUS does not suggest any specific diet after EUS-guided biliary drainage to prevent stent dysfunction.
(Level of evidence 5, Grade of recommendation: weak).
Summary of evidence
Stent dysfunction has been reported in published series up to 31%. Tumor over-in growth has been documented to be the primary cause of stent dysfunction; however, it is frequently described stent obstruction caused by food impaction, up to 40% [59, 89, 90]. Although food impaction has been reported in prospective and retrospective series as a cause of stent dysfunction, a special diet to prevent it has never been analyzed as a primary aim.
CLINICAL QUESTION #19
Is there evidence to recommend the administration of antibiotics to reduce the risk of post-procedural complications after EUS-guided biliary drainage?
Statement #19
i-EUS does not suggest the routine use of antibiotic prophylaxis, to reduce the risk of post-procedural complications after EUS-guided biliary drainage.
i-EUS suggest that antibiotic prophylaxis should be offered in selected patients (e.g., immunocompromised patients, expected incomplete biliary drainage).
(Level of evidence 5, Grade of recommendation: weak).
Summary of evidence
Infections may represent a fearful complication during EUS-guided procedures.
Despite this, the available literature does not show significant rates of infection after EUS-guided biliary drainage.
A large meta-analysis of one hundred fifty-five studies (7887 patients) showed that the pooled incidence of cholangitis after EUS-BD was 1.0% (95% CI 0.8–1.3), and the pooled incidence of major AEs (including but not limited to infections) was 0.6% (95% CI 0.3–0.9) [91].
According to another meta-analysis, the pooled rate of infection after EUS-BD was 3.8% (95% CI 2.8–5.1), without specifying, however, the rate of severe infections which are expected to be less prevalent [92].
Furthermore, there are currently no comparative studies demonstrating the efficacy of prophylaxis versus no antibiotic prophylaxis in preventing infections after EUS-BD.
However, some of these data can be translated from the setting of ERCP biliary drainage.
An old meta-analysis published in 1999 (5 RCTs, 1029 patients) found that the risk of sepsis or cholangitis following ERCP was not significantly decreased by routine antibiotic prophylaxis (OR 0.91, 95% CI 0.39 – 2.15) [93].
A recent meta-analysis of studies comparing the use of antibiotic vs non-antibiotic prophylaxis in patients undergoing elective ERCP (10 RCT, 1757 patients) confirmed the absence of significant difference in incidence of cholangitis [RD = − 0.02, 95% CI − 0.05, 0.02, p = 0.32], septicemia (RD = − 0.02, 95% CI − 0.06 to 0.01, p = 0.25), pancreatitis (RD = − 0.02, 95% CI − 0.06 to 0.01, p = 0.19), and all- cause mortality (RD = 0.00, 95% CI − 0.01 to 0.01, p = 0.71]. The antibiotic prophylaxis was associated with a 7% risk reduction in the incidence of bacteremia (RD = − 0.07, 95% CI − 0.14 to − 0.01, p = 0.03), but this has little clinical relevance [94].
Since post-procedural infections are most common in patients with expected incomplete drainage of biliary obstruction [95,96,97], current guidelines recommend antibiotic prophylaxis in patients with expected incomplete drainage of biliary obstruction [18, 98] [8, 9].
Similarly, patients with severe neutropenia and advanced hematologic malignancies are at increased risk for bacteremia and sepsis after GI endoscopy [99]. The protective effect of prophylactic antibiotics in these patients has not been studied. However, since this practice seems logical, guidelines recommend the use of antibiotic prophylaxis in immunocompromised patients with severe immunosuppression (absolute neutrophil count < 500 cells/mL, advanced hematologic malignancies, bone marrow transplantation, organ transplantation) [18, 98].
CLINICAL QUESTION #20
Is there evidence to recommend the periprocedural administration of drugs to improve endoscopic outcomes after stent placement?
Statement #20
i-EUS does not suggest the administration of medical therapy to improve endoscopic outcomes after biliary drainage for malignant distal biliary obstructions.
iEUS does not suggest the use of ursodeoxycholic acid (UDCA) since it is not effective in preventing recurrent biliary obstruction after SEMS placement and may increase the risk of stent occlusion.
(Level of evidence 5, Grade of recommendation: weak).
Summary of evidence
There are no studies in the literature investigating the potential role of drugs in improving endoscopic outcomes after LAMS placement, including stent patency. Regarding SEMS, recurrent biliary obstruction may occur primarily because of stent sludge occlusion, especially in fully covered SEMS with 7.9 to 11.1% occurrence rate and other factors [100,101,102].
A Cochrane meta-analysis (5 RCTs, 258 patients) was conducted to evaluate the effectiveness UDCA and/or antibiotics in prolonging stent patency and survival in patients with strictures of the biliary tract and endoscopically inserted stents [103]. Three trials, including 152 patients, investigated a combination of UDCA and antibiotics versus no treatment. The meta-analysis of these three trials does not show a significant treatment effect on the duration of stent patency (HR 0.58, 95% CI 0.22 to 1.54) or mortality (HR 0.99, 95% CI 0.68 to 1.43). Two trials with 106 patients compared antibiotics with no treatment. The pooled results of these two trials do not show significant effects of antibiotics on the duration of stent patency (HR 0.69 (95% CI 0.37 to 1.30)) or mortality (HR (fixed effect model) 1.23 (95% CI 0.72 to 2.08).
A recent propensity score–matched cohort analysis was conducted to assess the efficacy of ursodeoxycholic acid (UDCA) after SEMS placement for malignant distal biliary obstruction [104]. The study showed that the occlusion rate was 41.8% and 18.2% in the groups with and without UDCA, respectively (p = 0.0119). Median time to recurrent biliary obstruction was significantly longer in the control group than in the UDCA group (528 vs 154 days, p = 0.0381). Moreover, at multivariable analysis, UDCA was identified as the independent risk factor for reducing time to recurrent biliary obstruction (HR 2.28; 95% CI 1.06–4.88; p = 0.0348).
These data, therefore, do not allow to suggest the administration of medical therapy to improve endoscopic outcomes after biliary drainage for malignant distal biliary obstructions. The use of ursodeoxycholic to improve stent patency failed to demonstrate efficacy after SEMS placement, and its use is not recommended.
CLINICAL QUESTION #21
Considering the interplay between ERCP and EUS, and the possibility of same-session procedures, should we obtain a “goal-based” informed consent for endoscopic biliary drainage, overcoming the concept of “technical-based” ones?
Statement #21
i-EUS suggests obtaining a “goal-based” informed consent for endoscopic malignant biliary drainage prior to either EUS-guided drainage or conventional ERCP.
(Level of evidence: 5; Grade of recommendation: weak)
Summary of evidence
The synergy between EUS and ERCP and the potential for performing same-session EUS/ERCP procedures has raised implications that extend beyond the endoscopic room, particularly about obtaining proper informed consent (IC). Obtaining an effective IC is grounded in the fundamental human rights of autonomy and self-determination [105], and should encompass information regarding (i) the mechanisms of action, (ii) the balance between benefits and risks, and (iii) alternative treatment options.
Currently, various national and international endoscopy societies have introduced "technique-based" informed consent form templates for patients to sign before undergoing endoscopic procedures, aiming to establish a standardized approach. While these templates may be suitable for most purely diagnostic procedures, the field of interventional endoscopy has seen significant advancements in recent years, akin to developments in surgery. As a result, transitioning to a "goal-based" informed consent approach as happened in surgery may offer the most promising path to achieving our objectives within a single endoscopic session [106], thereby reducing the need for a second sedation, prolonged hospital stays, and associated costs.
Discussion
MBDO is a key event in the natural history of pancreatic cancer and cholangiocarcinoma: it may deflect patient prognosis and affect the clinical management, such as access to surgery and oncological therapy [1,2,3]. A broad work of the current literature search was done to provide evidence on which experts participating to the consensus conference found a general agreement. On a total of 23 statements discussed, experts found an agreement above 80% in 21 of them, which were presented and discussed in the current manuscript.
Of the two rejected, one clinical question that was discussed regarded how biliary drainage should be performed in non-surgical candidate patients with distal MBO when ERCP fails. It was proposed that repeated ERCP or percutaneous rendezvous-ERCP should be considered as second-line choices after ERCP failure. That statement did not reach consensus (disagreement: 25.8%), with several opinions reported for being not in favor. The main one concerned the current role of EUS-BD, which showed efficacy and safety to be considered not inferior to ERCP as an upfront technique [8, 11], thus being certainly an alternative in case of ERCP failure. Other concerns regarded the definition of repeated ERCP (vs. second look after pre-cut) and the availability of EUS-BD in non-experienced centers.
The other clinical question that did not reach consensus regarded whether or not potential surgical resectability represents a contraindication to EUS-guided biliary drainage and which biliary drainage should be performed in patients with localized malignancies candidates to neoadjuvant therapy. It was proposed to state that either ERCP or EUS-BD could be as valid in the case of potentially resectable diseases scheduled for neoadjuvant chemotherapy. Evidence considered in support of that statement were that EUS-BD might be associated with a lower complication rate as compared to ERCP, thus reducing the length of hospital stay and earlier access to neoadjuvant treatment [65, 67]. The main reasons for not agreeing with the proposed statement (disagreement 21.2%) were that evidences about EUS-BD in the specific setting of the patient candidate to neoadjuvant therapy are still very limited and that therefore EUS-BD should be considered only in centers with broad experience.
While our statements are generally align with the ESGE guidelines recommendations [18, 42], our consensus offers a deeper insight into the management of MDBO. In particular, detailed guidance is provided on how to manage specific challenges in EUS-BD, the preferred techniques, and the type of stents to use. For example, our consensus includes recommendations on managing patients with concomitant biliary and gastric outlet obstructions, including the potential use of EUS-guided double bypass techniques. We also discuss using EUS-GBD as a rescue strategy when other EUS-BD approaches are not feasible, considerations for the prevention of stent dysfunction, and the use of prophylactic measures. Additionally, a detailed comparison of different types of stents (LAMS vs. SEMS) and their respective advantages, particularly for EUS-CDS, as well as specific recommendations on stent sizes and configurations, are included in the consensus.
While the ESGE guidelines recommend EUS-BD primarily as an alternative or rescue therapy after ERCP failure, we suggest EUS-CDS as a potential first-line treatment for unresectable MDBO, reflecting a shift toward considering EUS-BD earlier in the treatment algorithm. This suggestion is based on newly available evidence (Supplementary Table 1). We also make specific statements on the use of EUS-guided gastroenterostomy, suggesting this approach not only as an alternative to duodenal stenting, but as a primary therapeutic option in patients with life expectancy greater than 3 months in the setting of experienced centers.
This manuscript has limitations that mostly pertain the fact that the techniques have been entered the clinical practice only recently. Studies taken into account dealt with different patients’ features, obstruction localization, and technical approach. Hence, studies published so far lead to low-quality evidence of many recommendations. Such a context of evidence uncertainty is what lead us to provide our scientific and clinical community of an experts’ guidance that may support the readers in understanding what might be the most appropriate decisions.
Management of MBDO is experiencing many changes, in light of the several technical innovations that have entered the clinical practice. The main limitation of this work thus is that it pertains a novel field of research, with evidences that are still not mature or validated in different settings or populations. Still, and because of that, we believe that this work may serve as a guide for clinicians to better understand which options are nowadays available and to propose the adequate opportunities to patients they care.
Abbreviations
- AE:
-
Adverse event
- CBD:
-
Common bile duct
- CDS:
-
Choledoco-duodenostomy
- CPG:
-
Clinical practice guideline
- DPPS:
-
Double pig-tail plastic Stents
- DPS:
-
Double pig-tail stent
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- ES:
-
Enteral stenting
- EDGE:
-
Endoscopic ultrasound-directed transgastric ERCP
- ESGE:
-
European society of gastrointestinal endoscopy
- EUS:
-
Endoscopic ultrasound
- EUS-AG:
-
EUS-guided antegrade
- EUS-BD:
-
EUS-guided biliary drainage
- EUS-CDS:
-
EUS-guided choledochoduodenostomy
- EUS-GBD:
-
EUS-guided gallbladder drainage
- EUS-GE:
-
EUS-guided gastroenterostomy
- EUS-HGS:
-
EUS-guided hepaticogastrostomy
- EUS-RV:
-
EUS-guided rendezvous
- GOO:
-
Gastric outlet obstruction
- HGS:
-
Hepaticogastrostomy
- IC:
-
Informed consent
- i-EUS:
-
Italian network of clinicians and scientists with a special interest in biliopancreatic endoscopy EUS
- LAMS:
-
Lumen-apposing metal stents
- MDBO:
-
Malignant distal biliary obstruction
- OCEBM:
-
Oxford centre for evidence-based medicine
- PBD:
-
Preoperative biliary drainage
- PICO:
-
Patient, intervention, comparison, outcome
- PTBD:
-
Percutaneous transhepatic biliary drainage
- RCT:
-
Randomized controlled trial
- RYGB:
-
Roux-en-Y gastric bypass
- SAA:
-
Surgically altered anatomy
- SEMS:
-
Self-expandable metal stents
- UDCA:
-
Ursodeoxycholic acid
References
Klein AP (2021) Pancreatic cancer epidemiology: understanding the role of lifestyle and inherited risk factors. Nat Rev Gastroenterol Hepatol 18:493–502
Banales JM, Marin JJG, Lamarca A, Rodrigues PM, Khan SA, Roberts LR et al (2020) Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat Rev Gastroenterol Hepatol 17:557–588
Chen YI, Sahai A, Donatelli G, Lam E, Forbes N, Mosko J et al (2023) Endoscopic ultrasound-guided biliary drainage of first intent with a lumen-apposing metal stent vs endoscopic retrograde cholangiopancreatography in malignant distal biliary obstruction: a multicenter randomized controlled study (ELEMENT trial). Gastroenterology 165(1249–1261):e1245
Cornberg M, Tacke F, Karlsen TH (2019) European Association for the Study of the L. Clinical Practice Guidelines of the European Association for the study of the Liver—Advancing methodology but preserving practicability. J Hepatol 70:5–7
Bang JY, Navaneethan U, Hasan M, Hawes R, Varadarajulu S (2018) Stent placement by EUS or ERCP for primary biliary decompression in pancreatic cancer: a randomized trial (with videos). Gastrointest Endosc 88:9–17
Paik WH, Lee TH, Park DH, Choi JH, Kim SO, Jang S et al (2018) EUS-guided biliary drainage versus ERCP for the primary palliation of malignant biliary obstruction: a multicenter randomized clinical trial. Am J Gastroenterol 113:987–997
Park JK, Woo YS, Noh DH, Yang JI, Bae SY, Yun HS et al (2018) Efficacy of EUS-guided and ERCP-guided biliary drainage for malignant biliary obstruction: prospective randomized controlled study. Gastrointest Endosc 88:277–282
Teoh AYB, Napoleon B, Kunda R, Arcidiacono PG, Kongkam P, Larghi A et al (2023) EUS-guided choledocho-duodenostomy using lumen apposing stent versus ERCP With covered metallic stents in patients with unresectable malignant distal biliary obstruction: a multicenter randomized controlled trial (DRA-MBO Trial). Gastroenterology 165(473–482):e472
Kakked G, Salameh H, Cheesman AR, Kumta NA, Nagula S, DiMaio CJ (2020) Primary EUS-guided biliary drainage versus ERCP drainage for the management of malignant biliary obstruction: a systematic review and meta-analysis. Endosc Ultrasound 9:298–307
Jin Z, Wei Y, Lin H, Huang H, Lv W, Zhang X (2019) Endoscopic ultrasound versus endoscopic retrograde cholangiopancreatography-guided biliary drainage for primary decompression of malignant biliary obstruction: protocol for a systematic review and meta-analysis of randomised controlled trials. BMJ Open 9:e028156
Chan SM, Dhir V, Chan YYY, Cheung CHN, Chow JCS, Wong IWM et al (2023) Endoscopic ultrasound-guided balloon-occluded gastrojejunostomy bypass, duodenal stent or laparoscopic gastrojejunostomy for unresectable malignant gastric outlet obstruction. Dig Endosc 35:512–519
van der Gaag NA, Rauws EA, van Eijck CH, Bruno MJ, van der Harst E, Kubben FJ et al (2010) Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med 362:129–137
Moole H, Bechtold M, Puli SR (2016) Efficacy of preoperative biliary drainage in malignant obstructive jaundice: a meta-analysis and systematic review. World J Surg Oncol 14:182
Saleh MM, Norregaard P, Jorgensen HL, Andersen PK, Matzen P (2002) Preoperative endoscopic stent placement before pancreaticoduodenectomy: a meta-analysis of the effect on morbidity and mortality. Gastrointest Endosc 56:529–534
Lee PJ, Podugu A, Wu D, Lee AC, Stevens T, Windsor JA (2018) Preoperative biliary drainage in resectable pancreatic cancer: a systematic review and network meta-analysis. HPB (Oxford) 20:477–486
Fang Y, Gurusamy KS, Wang Q, Davidson BR, Lin H, Xie X et al (2013) Meta-analysis of randomized clinical trials on safety and efficacy of biliary drainage before surgery for obstructive jaundice. Br J Surg 100:1589–1596
Sewnath ME, Karsten TM, Prins MH, Rauws EJ, Obertop H, Gouma DJ (2002) A meta-analysis on the efficacy of preoperative biliary drainage for tumors causing obstructive jaundice. Ann Surg 236:17–27
Dumonceau JM, Tringali A, Papanikolaou IS, Blero D, Mangiavillano B, Schmidt A et al (2018) Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy 50:910–930
Fugazza A, Fabbri C, Di Mitri R, Petrone MC, Colombo M, Cugia L et al (2022) EUS-guided choledochoduodenostomy for malignant distal biliary obstruction after failed ERCP: a retrospective nationwide analysis. Gastrointest Endosc 95(896–904):e891
Fabbri C, Coluccio C, Binda C, Fugazza A, Anderloni A, Tarantino I et al (2022) Lumen-apposing metal stents: how far are we from standardization? An Italian survey. Endosc Ultrasound 11:59–67
van Wanrooij RLJ, Bronswijk M, Kunda R, Everett SM, Lakhtakia S, Rimbas M et al (2022) Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy 54:310–332
Donato G, Occhipinti P, Correale L, Spadaccini M, Repici A, Anderloni A et al (2021) A prospective study on quality in endoscopic retrograde cholangiopancreatography (ERCP): trend in Italy from the REQUEST study. Endosc Int Open 9:E1563–E1571
Jeurnink SM, Steyerberg E, Kuipers E, Siersema P (2012) The burden of endoscopic retrograde cholangiopancreatography (ERCP) performed with the patient under conscious sedation. Surg Endosc 26:2213–2219
Facciorusso A, Mangiavillano B, Paduano D, Binda C, Crino SF, Gkolfakis P et al (2022) Methods for drainage of distal malignant biliary obstruction after ERCP failure: a systematic review and network meta-analysis. Cancers (Basel) 14:8
Minaga K, Ogura T, Shiomi H, Imai H, Hoki N, Takenaka M et al (2019) Comparison of the efficacy and safety of endoscopic ultrasound-guided choledochoduodenostomy and hepaticogastrostomy for malignant distal biliary obstruction: Multicenter, randomized, clinical trial. Dig Endosc 31:575–582
Artifon EL, Marson FP, Gaidhane M, Kahaleh M, Otoch JP (2015) Hepaticogastrostomy or choledochoduodenostomy for distal malignant biliary obstruction after failed ERCP: is there any difference? Gastrointest Endosc 81:950–959
Artifon EL, Aparicio D, Paione JB, Lo SK, Bordini A, Rabello C et al (2012) Biliary drainage in patients with unresectable, malignant obstruction where ERCP fails: endoscopic ultrasonography-guided choledochoduodenostomy versus percutaneous drainage. J Clin Gastroenterol 46:768–774
Lee TH, Choi JH, Park-do H, Song TJ, Kim DU, Paik WH et al (2016) Similar Efficacies of Endoscopic Ultrasound-guided Transmural and Percutaneous Drainage for Malignant Distal Biliary Obstruction. Clin Gastroenterol Hepatol 14:1011–1019
Imai H, Kitano M, Omoto S, Kadosaka K, Kamata K, Miyata T et al (2016) EUS-guided gallbladder drainage for rescue treatment of malignant distal biliary obstruction after unsuccessful ERCP. Gastrointest Endosc 84:147–151
Kamal F, Khan MA, Lee-Smith W, Sharma S, Acharya A, Farooq U et al (2023) Efficacy and safety of EUS-guided gallbladder drainage for rescue treatment of malignant biliary obstruction: A systematic review and meta-analysis. Endosc Ultrasound 12:8–15
Amato A, Sinagra E, Celsa C, Enea M, Buda A, Vieceli F et al (2021) Efficacy of lumen-apposing metal stents or self-expandable metal stents for endoscopic ultrasound-guided choledochoduodenostomy: a systematic review and meta-analysis. Endoscopy 53:1037–1047
de Benito SM, Najera-Munoz R, de la Serna-Higuera C, Fuentes-Valenzuela E, Fanjul I, Chavarria C et al (2021) Lumen apposing metal stents versus tubular self-expandable metal stents for endoscopic ultrasound-guided choledochoduodenostomy in malignant biliary obstruction. Surg Endosc 35:6754–6762
Jacques J, Privat J, Pinard F, Fumex F, Valats JC, Chaoui A et al (2019) Endoscopic ultrasound-guided choledochoduodenostomy with electrocautery-enhanced lumen-apposing stents: a retrospective analysis. Endoscopy 51:540–547
Jacques J, Privat J, Pinard F, Fumex F, Chaput U, Valats JC et al (2020) EUS-guided choledochoduodenostomy by use of electrocautery-enhanced lumen-apposing metal stents: a French multicenter study after implementation of the technique (with video). Gastrointest Endosc 92:134–141
On W, Paranandi B, Smith AM, Venkatachalapathy SV, James MW, Aithal GP et al (2022) EUS-guided choledochoduodenostomy with electrocautery-enhanced lumen-apposing metal stents in patients with malignant distal biliary obstruction: multicenter collaboration from the United Kingdom and Ireland. Gastrointest Endosc 95:432–442
El Chafic AH, Shah JN, Hamerski C, Binmoeller KF, Irani S, James TW et al (2019) EUS-guided choledochoduodenostomy for distal malignant biliary obstruction using electrocautery-enhanced lumen-apposing metal stents: first US. Multicenter Experience Dig Dis Sci 64:3321–3327
Garcia-Sumalla A, Loras C, Guarner-Argente C, Velasquez-Rodriguez JG, Andujar X, Salord S et al (2021) Is a coaxial plastic stent within a lumen-apposing metal stent useful for the management of distal malignant biliary obstruction? Surg Endosc 35:4873–4881
Nakai Y, Sato T, Hakuta R, Ishigaki K, Saito K, Saito T et al (2020) Long-term outcomes of a long, partially covered metal stent for EUS-guided hepaticogastrostomy in patients with malignant biliary obstruction (with video). Gastrointest Endosc 92(623–631):e621
Cho DH, Lee SS, Oh D, Song TJ, Park DH, Seo DW et al (2017) Long-term outcomes of a newly developed hybrid metal stent for EUS-guided biliary drainage (with videos). Gastrointest Endosc 85:1067–1075
Anderloni A, Fugazza A, Spadaccini M, Colombo M, Capogreco A, Carrara S et al (2023) Feasibility and safety of a new dedicated biliary stent for EUS-guided hepaticogastrostomy: the FIT study (with video). Endosc Ultrasound 12:59–63
Binda C, Dajti E, Giuffrida P, Trebbi M, Coluccio C, Cucchetti A, et al. (2024) Efficacy and safety of endoscopic ultrasound-guided hepaticogastrostomy: a meta-regression analysis. Endoscopy
van der Merwe SW, van Wanrooij RLJ, Bronswijk M, Everett S, Lakhtakia S, Rimbas M et al (2022) Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 54:185–205
van Hooft JE, Uitdehaag MJ, Bruno MJ, Timmer R, Siersema PD, Dijkgraaf MG et al (2009) Efficacy and safety of the new WallFlex enteral stent in palliative treatment of malignant gastric outlet obstruction (DUOFLEX study): a prospective multicenter study. Gastrointest Endosc 69:1059–1066
Sato T, Hara K, Mizuno N, Hijioka S, Imaoka H, Yogi T et al (2016) Type of combined endoscopic biliary and gastroduodenal stenting is significant for biliary route maintenance. Intern Med 55:2153–2161
Khashab M, Alawad AS, Shin EJ, Kim K, Bourdel N, Singh VK et al (2013) Enteral stenting versus gastrojejunostomy for palliation of malignant gastric outlet obstruction. Surg Endosc 27:2068–2075
Chen YI, Itoi T, Baron TH, Nieto J, Haito-Chavez Y, Grimm IS et al (2017) EUS-guided gastroenterostomy is comparable to enteral stenting with fewer re-interventions in malignant gastric outlet obstruction. Surg Endosc 31:2946–2952
Ge PS, Young JY, Dong W, Thompson CC (2019) EUS-guided gastroenterostomy versus enteral stent placement for palliation of malignant gastric outlet obstruction. Surg Endosc 33:3404–3411
Sanchez-Aldehuelo R, Subtil Inigo JC, Martinez Moreno B, Gornals J, Guarner-Argente C, Repiso Ortega A et al (2022) EUS-guided gastroenterostomy versus duodenal self-expandable metal stent for malignant gastric outlet obstruction: results from a nationwide multicenter retrospective study (with video). Gastrointest Endosc 96(1012–1020):e1013
Vanella G, Dell’Anna G, Capurso G, Maisonneuve P, Bronswijk M, Crippa S et al (2023) EUS-guided gastroenterostomy for management of malignant gastric outlet obstruction: a prospective cohort study with matched comparison with enteral stenting. Gastrointest Endosc 98(337–347):e335
Boghossian MB, Funari MP, De Moura DTH, McCarty TR, Sagae VMT, Chen YI et al (2021) EUS-guided gastroenterostomy versus duodenal stent placement and surgical gastrojejunostomy for the palliation of malignant gastric outlet obstruction: a systematic review and meta-analysis. Langenbecks Arch Surg 406:1803–1817
Krishnamoorthi R, Bomman S, Benias P, Kozarek RA, Peetermans JA, McMullen E et al (2022) Efficacy and safety of endoscopic duodenal stent versus endoscopic or surgical gastrojejunostomy to treat malignant gastric outlet obstruction: systematic review and meta-analysis. Endosc Int Open 10:E874–E897
Mutignani M, Tringali A, Shah SG, Perri V, Familiari P, Iacopini F et al (2007) Combined endoscopic stent insertion in malignant biliary and duodenal obstruction. Endoscopy 39:440–447
Khashab MA, Valeshabad AK, Leung W, Camilo J, Fukami N, Shieh F et al (2014) Multicenter experience with performance of ERCP in patients with an indwelling duodenal stent. Endoscopy 46:252–255
Simoes PK, Schattner MA, Gerdes H, Shah PM, Kurtz RC, Mendelsohn RB (2022) Endoscopic stenting for malignant biliary obstruction is technically successful in patients with preexisting duodenal stents. Endosc Int Open 10:E429–E433
Staub J, Siddiqui A, Taylor LJ, Loren D, Kowalski T, Adler DG (2018) ERCP performed through previously placed duodenal stents: a multicenter retrospective study of outcomes and adverse events. Gastrointest Endosc 87:1499–1504
Yamao K, Kitano M, Takenaka M, Minaga K, Sakurai T, Watanabe T et al (2018) Outcomes of endoscopic biliary drainage in pancreatic cancer patients with an indwelling gastroduodenal stent: a multicenter cohort study in West Japan. Gastrointest Endosc 88(66–75):e62
Rizzo GEM, Carrozza L, Quintini D, Ligresti D, Traina M, Tarantino I (2023) A systematic review of endoscopic treatments for concomitant malignant biliary obstruction and malignant gastric outlet obstruction and the outstanding role of endoscopic ultrasound-guided therapies. Cancers (Basel) 15:8
Canakis A, Hathorn KE, Irani SS, Baron TH (2022) Single session endoscopic ultrasound-guided double bypass (hepaticogastrostomy and gastrojejunostomy) for concomitant duodenal and biliary obstruction: a case series. J Hepatobiliary Pancreat Sci 29:941–949
Vanella G, Bronswijk M, van Wanrooij RL, Dell’Anna G, Laleman W, van Malenstein H et al (2023) Combined endoscopic mAnagement of BiliaRy and gastrIc OutLET obstruction (CABRIOLET Study): a multicenter retrospective analysis. DEN Open 3:e132
Bronswijk M, Vanella G, van Wanrooij RLJ, Samanta J, Lauwereys J, Perez-Cuadrado-Robles E et al (2023) Same-session double EUS-guided bypass versus surgical gastroenterostomy and hepaticojejunostomy: an international multicenter comparison. Gastrointest Endosc 98(225–236):e221
Uemura RS, Khan MA, Otoch JP, Kahaleh M, Montero EF, Artifon ELA (2018) EUS-guided choledochoduodenostomy versus hepaticogastrostomy: a systematic review and meta-analysis. J Clin Gastroenterol 52:123–130
Hedjoudje A, Sportes A, Grabar S, Zhang A, Koch S, Vuitton L et al (2019) Outcomes of endoscopic ultrasound-guided biliary drainage: a systematic review and meta-analysis. United European Gastroenterol J 7:60–68
Mao K, Hu B, Sun F, Wan K (2021) Choledochoduodenostomy versus hepaticogastrostomy in endoscopic ultrasound-guided drainage for malignant biliary obstruction: a meta-analysis and systematic review. Surg Laparosc Endosc Percutan Tech 32:124–132
Ogura T, Chiba Y, Masuda D, Kitano M, Sano T, Saori O et al (2016) Comparison of the clinical impact of endoscopic ultrasound-guided choledochoduodenostomy and hepaticogastrostomy for bile duct obstruction with duodenal obstruction. Endoscopy 48:156–163
Janet J, Albouys J, Napoleon B, Jacques J, Mathonnet M, Magne J et al (2023) Pancreatoduodenectomy following preoperative biliary drainage using endoscopic ultrasound-guided choledochoduodenostomy versus a transpapillary stent: a multicenter comparative cohort study of the ACHBT-FRENCH-SFED intergroup. Ann Surg Oncol 30:5036–5046
Gaujoux S, Jacques J, Bourdariat R, Sulpice L, Lesurtel M, Truant S et al (2021) Pancreaticoduodenectomy following endoscopic ultrasound-guided choledochoduodenostomy with electrocautery-enhanced lumen-apposing stents an ACHBT - SFED study. HPB (Oxford) 23:154–160
Fabbri C, Fugazza A, Binda C, Zerbi A, Jovine E, Cennamo V et al (2019) Beyond palliation: using EUS-guided choledochoduodenostomy with a lumen-apposing metal stent as a bridge to surgery: a case series. J Gastrointestin Liver Dis 28:125–128
Kim SB, Kim KH, Kim TN (2023) Comparison of endoscopic retrograde cholangiopancreatography outcomes between cap-fitted forward and side viewing endoscopes in patients with Billroth II anastomosis. BMC Gastroenterol 23:115
Wang F, Xu B, Li Q, Zhang X, Jiang G, Ge X et al (2016) Endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: One single center’s experience. Medicine (Baltimore) 95:e5743
Park TY, Bang CS, Choi SH, Yang YJ, Shin SP, Suk KT et al (2018) Forward-viewing endoscope for ERCP in patients with Billroth II gastrectomy: a systematic review and meta-analysis. Surg Endosc 32:4598–4613
Iwashita T, Uemura S, Mita N, Iwasa Y, Ichikawa H, Mukai T et al (2020) Endoscopic ultrasound guided-antegrade biliary stenting vs percutaneous transhepatic biliary stenting for unresectable distal malignant biliary obstruction in patients with surgically altered anatomy. J Hepatobiliary Pancreat Sci 27:968–976
Khashab MA, El Zein MH, Sharzehi K, Marson FP, Haluszka O, Small AJ et al (2016) EUS-guided biliary drainage or enteroscopy-assisted ERCP in patients with surgical anatomy and biliary obstruction: an international comparative study. Endosc Int Open 4:E1322–E1327
Minaga K, Takenaka M, Ogura T, Tamura T, Kuroda T, Kaku T et al (2020) Endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction with surgically altered anatomy: a multicenter prospective registration study. Therap Adv Gastroenterol 13:1756284820930964
Ogura T, Kitano M, Takenaka M, Okuda A, Minaga K, Yamao K et al (2018) Multicenter prospective evaluation study of endoscopic ultrasound-guided hepaticogastrostomy combined with antegrade stenting (with video). Dig Endosc 30:252–259
Deliwala SS, Mohan BP, Yarra P, Khan SR, Chandan S, Ramai D et al (2023) Efficacy & safety of EUS-directed transgastric endoscopic retrograde cholangiopancreatography (EDGE) in Roux-en-Y gastric bypass anatomy: a systematic review & meta-analysis. Surg Endosc 37:4144–4158
Connell M, Sun WYL, Mocanu V, Dang JT, Kung JY, Switzer NJ et al (2022) Management of choledocholithiasis after Roux-en-Y gastric bypass: a systematic review and pooled proportion meta-analysis. Surg Endosc 36:6868–6877
Krafft MR, Hsueh W, James TW, Runge TM, Baron TH, Khashab MA et al (2019) The EDGI new take on EDGE: EUS-directed transgastric intervention (EDGI), other than ERCP, for Roux-en-Y gastric bypass anatomy: a multicenter study. Endosc Int Open 7:E1231–E1240
Pillay B, Wootten AC, Crowe H, Corcoran N, Tran B, Bowden P et al (2016) The impact of multidisciplinary team meetings on patient assessment, management and outcomes in oncology settings: a systematic review of the literature. Cancer Treat Rev 42:56–72
Quero G, De Sio D, Fiorillo C, Menghi R, Rosa F, Massimiani G et al (2023) The role of the multidisciplinary tumor board (MDTB) in the assessment of pancreatic cancer diagnosis and resectability: a tertiary referral center experience. Front Surg 10:1119557
Basta YL, Baur OL, van Dieren S, Klinkenbijl JH, Fockens P, Tytgat KM (2016) Is there a Benefit of Multidisciplinary Cancer Team Meetings for Patients with Gastrointestinal Malignancies? Ann Surg Oncol 23:2430–2437
Tempero MA, Malafa MP, Al-Hawary M, Behrman SW, Benson AB, Cardin DB et al (2021) Pancreatic adenocarcinoma, version 22021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 19:439–457
Attasaranya S, Netinasunton N, Jongboonyanuparp T, Sottisuporn J, Witeerungrot T, Pirathvisuth T et al (2012) The spectrum of endoscopic ultrasound intervention in biliary diseases: a single center’s experience in 31 cases. Gastroenterol Res Pract 2012:680753
Vila JJ, Perez-Miranda M, Vazquez-Sequeiros E, Abadia MA, Perez-Millan A, Gonzalez-Huix F et al (2012) Initial experience with EUS-guided cholangiopancreatography for biliary and pancreatic duct drainage: a Spanish national survey. Gastrointest Endosc 76:1133–1141
Poincloux L, Rouquette O, Buc E, Privat J, Pezet D, Dapoigny M et al (2015) Endoscopic ultrasound-guided biliary drainage after failed ERCP: cumulative experience of 101 procedures at a single center. Endoscopy 47:794–801
Hara K, Yamao K, Mizuno N, Hijioka S, Imaoka H, Tajika M et al (2016) Endoscopic ultrasonography-guided biliary drainage: who, when, which, and how? World J Gastroenterol 22:1297–1303
Tyberg A, Mishra A, Cheung M, Kedia P, Gaidhane M, Craig C et al (2020) Learning curve for EUS-guided biliary drainage: what have we learned? Endosc Ultrasound 9:392–396
Oh D, Park DH, Song TJ, Lee SS, Seo DW, Lee SK et al (2017) Optimal biliary access point and learning curve for endoscopic ultrasound-guided hepaticogastrostomy with transmural stenting. Therap Adv Gastroenterol 10:42–53
Sagami R, Mizukami K, Okamoto K, Noguchi C, Sato T, Nishikiori H et al (2023) Experience-related factors in the success of beginner endoscopic ultrasound-guided biliary drainage: a multicenter study. J Clin Med 12:89
Geyl S, Redelsperger B, Yzet C, Napoleon B, Legros R, Dahan M et al (2023) Risk factors for stent dysfunction during long-term follow-up after EUS-guided biliary drainage using lumen-apposing metal stents: A prospective study. Endosc Ultrasound 12:237–244
Teoh AYB, Kongkam P, Bapaye A, Ratanachu T, Reknimitr R, Lakthakia S et al (2021) Use of a novel lumen apposing metallic stent for drainage of the bile duct and gallbladder: Long term outcomes of a prospective international trial. Dig Endosc 33:1139–1145
Giri S, Mohan BP, Jearth V, Kale A, Angadi S, Afzalpurkar S et al (2023) Adverse events with EUS-guided biliary drainage: a systematic review and meta-analysis. Gastrointest Endosc 98(515–523):e518
Dhindsa BS, Mashiana HS, Dhaliwal A, Mohan BP, Jayaraj M, Sayles H et al (2020) EUS-guided biliary drainage: a systematic review and meta-analysis. Endosc Ultrasound 9:101–109
Harris A, Chan AC, Torres-Viera C, Hammett R, Carr-Locke D (1999) Meta-analysis of antibiotic prophylaxis in endoscopic retrograde cholangiopancreatography (ERCP). Endoscopy 31:718–724
Merchan MFS, de Moura DTH, de Oliveira GHP, Proenca IM, do Monte Junior ES, Ide E, et al (2022) Antibiotic prophylaxis to prevent complications in endoscopic retrograde cholangiopancreatography: a systematic review and meta-analysis of randomized controlled trials. World J Gastrointest Endosc 14:718–730
Allison MC, Sandoe JA, Tighe R, Simpson IA, Hall RJ, Elliott TS et al (2009) Antibiotic prophylaxis in gastrointestinal endoscopy. Gut 58:869–880
Ishigaki T, Sasaki T, Serikawa M, Kobayashi K, Kamigaki M, Minami T et al (2015) Evaluation of antibiotic use to prevent post-endoscopic retrograde cholangiopancreatography pancreatitis and cholangitis. Hepatogastroenterology 62:417–424
Wobser H, Gunesch A, Klebl F (2017) Prophylaxis of post-ERC infectious complications in patients with biliary obstruction by adding antimicrobial agents into ERC contrast media- a single center retrospective study. BMC Gastroenterol 17:10
Committee ASOP, Khashab MA, Chithadi KV, Acosta RD, Bruining DH, Chandrasekhara V et al (2015) Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc 81:81–89
Bianco JA, Pepe MS, Higano C, Applebaum FR, McDonald GB, Singer JW (1990) Prevalence of clinically relevant bacteremia after upper gastrointestinal endoscopy in bone marrow transplant recipients. Am J Med 89:134–136
Hamada T, Isayama H, Nakai Y, Iwashita T, Ito Y, Mukai T et al (2019) Antireflux covered metal stent for nonresectable distal malignant biliary obstruction: Multicenter randomized controlled trial. Dig Endosc 31:566–574
Mukai T, Yasuda I, Isayama H, Iwashita T, Itoi T, Kawakami H et al (2016) Pilot study of a novel, large-bore, fully covered self-expandable metallic stent for unresectable distal biliary malignancies. Dig Endosc 28:671–679
Conio M, Mangiavillano B, Caruso A, Filiberti RA, Baron TH, De Luca L et al (2018) Covered versus uncovered self-expandable metal stent for palliation of primary malignant extrahepatic biliary strictures: a randomized multicenter study. Gastrointest Endosc 88(283–291):e283
Galandi D, Schwarzer G, Bassler D, Allgaier HP (2002) Ursodeoxycholic acid and/or antibiotics for prevention of biliary stent occlusion. Cochrane Database Syst Rev 5:03043
Okuno M, Iwata K, Mukai T, Ohashi Y, Iwata S, Iwasa Y et al (2023) Effect of ursodeoxycholic acid after self-expandable metal stent placement in malignant distal biliary obstruction: a propensity score-matched cohort analysis. Gastrointest Endosc 97(713–721):e716
Aagaard L, Kristensen K (2018) Off-label and unlicensed prescribing in Europe: implications for patients’ informed consent and liability. Int J Clin Pharm 40:509–512
Spadaccini M, Binda C, Fugazza A, Repici A, Tarantino I, Fabbri C et al (2022) Informed consent for endoscopic biliary drainage: time for a new paradigm. Medicina (Kaunas) 58:9
Funding
Open access funding provided by Università Politecnica delle Marche within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
Andrea Anderloni: Consultant for Boston Scientific, Olympus. Paolo Giorgio Arcidiacono: Consultant for AMBU, Boston Scientific, FujiFilm, MediGlobe, Pentax. Cecilia Binda: Lecturer for Q3 Medical and Boston Scientific. Carlo Fabbri: Consultant for Boston Scientific. Alessandro Fugazza: Consultant for Boston Scientific. Andrea Lisotti: Consultant for Boston Scientific. Ilaria Tarantino: Consultant for Olympus. Giuseppe Vanella: Lecturer for Boston Scientific.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Marzioni, M., Crinò, S.F., Lisotti, A. et al. Biliary drainage in patients with malignant distal biliary obstruction: results of an Italian consensus conference. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-11245-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-11245-4