Abstract
Background
Liver resection offers substantial advantages over open liver resection (OLR) for patients with hepatocellular carcinoma (HCC) in terms of reduced intraoperative blood loss and morbidity. However, there is limited evidence comparing the indications and perioperative outcomes with the open versus laparoscopic approach for resection. This study aimed to compare postoperative outcomes between patients undergoing laparoscopic liver resection (LLR) and OLR for HCC with clinically significant portal hypertension (CSPH).
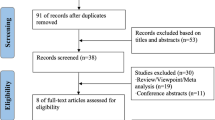
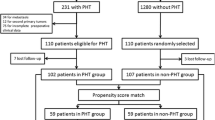
Methods
A total of 316 HCC patients with CSPH (the presence of gastroesophageal varices or platelet count < 100,000/ml and spleen diameter > 12 cm) undergoing minor liver resection at eight centers were included in this study. To adjust for confounding factors between the LLR and OLR groups, an inverse probability weighting method analysis was performed.
Results
Overall, 193 patients underwent LLR and 123 underwent OLR. After weighting, LLR was associated with a lower volume of intraoperative blood loss and the incidence of postoperative complications (including pulmonary complications, incisional surgical site infection, and paralytic ileus) compared to the OLR group. The 3-, 5-, and 7-year postoperative recurrence-free survival rates were 39%, 26%, and 22% in the LLR group and 49%, 18%, and 18% in the OLR group, respectively (p = 0.18). And, the 3-, 5-, and 7-year postoperative overall survival rates were 71%, 56%, and 44% in the LLR group and 76%, 51%, 44% in the OLR group, respectively (p = 0.87).
Conclusions
LLR for HCC patients with CSPH is clinically advantageous by lowering the volume of intraoperative blood loss and incidence of postoperative complications, thereby offering feasible long-term survival.
Graphical abstract





Similar content being viewed by others
References
Bruix J, Gores GJ, Mazzaferro V (2014) Hepatocellular carcinoma: clinical frontiers and perspectives. Gut 63:844–855
Nababan SHH, Lesmana CRA (2022) Portal hypertension in nonalcoholic fatty liver disease: from pathogenesis to clinical practice. J Clin Transl Hepatol 10:979–985
Sakiani S, Heller T (2022) Current and investigational drugs in early clinical development for portal hypertension. Front Med (Lausanne) 9:974182
European Association for the Study of the Liver (2018) EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 69:182–236
Liu J, Zhang H, Xia Y, Yang T, Gao Y, Li J et al (2019) Impact of clinically significant portal hypertension on outcomes after partial hepatectomy for hepatocellular carcinoma: a systematic review and meta-analysis. HPB (Oxford) 21:1–13
Ishizawa T, Hasegawa K, Aoki T, Takahashi M, Inoue Y, Sano K et al (2008) Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology 134:1908–1916
Oba A, Ishizawa T, Mise Y, Inoue Y, Ito H, Ono Y et al (2019) Possible underestimation of blood loss during laparoscopic hepatectomy. BJS Open 3:336–343
Takahara T, Wakabayashi G, Beppu T, Aihara A, Hasegawa K, Gotohda N et al (2015) Long-term and perioperative outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma with propensity score matching: a multi-institutional Japanese study. J Hepato-Bil Pancreat Sci 22:721–727
Ishizawa T, Hasegawa K, Kokudo N, Sano K, Imamura H, Beck Y et al (2009) Risk factors and management of ascites after liver resection to treat hepatocellular carcinoma. Arch Surg 144:46–51
Uchiyama H, Harimoto N, Itoh S, Yoshizaumi T, Ikegami T, Maehara Y (2017) Pleural effusion after hepatectomy for hepatocellular carcinoma: risk factor analyses and its impact on oncological outcomes. World J Surg 41:1089–1099
Zhao Y, Jin Y, Wu Y (2016) Postoperative infectious complications after liver resection for hepatocellular carcinoma. J Cancer Res Ther 12:C268-270
Li YR, Chen JD, Huang J, Wu FX, Jin GZ (2022) Post-hepatectomy liver failure prediction and prevention: development of a nomogram containing postoperative anticoagulants as a risk factor. Ann Hepatol 27:100744
Imai D, Maeda T, Wang H, Shimagaki T, Sanefuji K, Kayashima H et al (2021) Risk factors for and outcomes of intraoperative blood loss in liver resection for hepatocellular tumors. Am Surg 87:376–383
Molina V, Sampson-Davila J, Ferrer J, Fondevila C, Diaz Del Gobbo R, Calatayud D et al (2018) Benefits of laparoscopic liver resection in patients with hepatocellular carcinoma and portal hypertension: a case-matched study. Surg Endosc 32:2345–2354
Lim C, Osseis M, Lahat E, Doussot A, Sotirov D, Hemery F et al (2019) Safety of laparoscopic hepatectomy in patients with hepatocellular carcinoma and portal hypertension: interim analysis of an open prospective study. Surg Endosc 33:811–820
Zheng J, Feng X, Liang Y, Cai J, Shi Z, Kirih MA et al (2021) Safety and feasibility of laparoscopic liver resection for hepatocellular carcinoma with clinically significant portal hypertension: a propensity score-matched study. Surg Endosc 35:3267–3278
Casellas-Robert M, Lim C, Lopez-Ben S, Llado L, Salloum C, Codina-Font J et al (2020) Laparoscopic liver resection for hepatocellular carcinoma in Child-Pugh A patients with and without portal hypertension: a multicentre study. World J Surg 44:3915–3922
Harada N, Maeda T, Yoshizumi T, Ikeda T, Kayashima H, Ikegami T et al (2016) Laparoscopic liver resection is a feasible treatment for patients with hepatocellular carcinoma and portal hypertension. Anticancer Res 36:3489–3497
Azoulay D, Ramos E, Casellas-Robert M, Salloum C, Llado L, Nadler R et al (2021) Liver resection for hepatocellular carcinoma in patients with clinically significant portal hypertension. JHEP Rep 3:100190
Llovet JM, Bru C, Bruix J (1999) Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 19:329–338
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L (1996) Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 334:693–699
Ueno M, Hayami S, Sonomura T, Kawai M, Hirono S, Okada KI et al (2019) Concomitant use of indocyanine green fluorescence imaging and interventional radiology for detection of liver segments during laparoscopic anatomical liver resection: pilot feasibility study. Surg Laparosc Endosc Percutan Tech 29:242–246
Ishizawa T, Gumbs AA, Kokudo N, Gayet B (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256:959–964
Lim C, Ishizawa T, Miyata A, Mise Y, Sakamoto Y, Hasegawa K et al (2016) Surgical indications and procedures for resection of hepatic malignancies confined to segment VII. Ann Surg 263:529–537
Liang X, Zheng J, Xu J, Tao L, Cai J, Liang Y et al (2021) Laparoscopic anatomical portal territory hepatectomy using Glissonean pedicle approach (Takasaki approach) with indocyanine green fluorescence negative staining: how I do it. HPB (Oxford) 23:1392–1399
Hu JX, Dai WD, Miao XY, Zhong DW, Huang SF, Wen Y et al (2009) Anatomic resection of segment VIII of liver for hepatocellular carcinoma in cirrhotic patients based on an intrahepatic Glissonian approach. Surgery 146:854–860
Wada H, Eguchi H, Nagano H, Kubo S, Nakai T, Kaibori M et al (2018) Perioperative allogenic blood transfusion is a poor prognostic factor after hepatocellular carcinoma surgery: a multi-center analysis. Surg Today 48:73–79
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the international study group of liver surgery. Surgery 149:680–688
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Hospital infection control practices advisory committee. Infect Control Hosp Epidemiol 1999(20):250–278
Famularo S, Donadon M, Cipriani F, Ardito F, Iaria M, Carissimi F et al (2021) The impact of postoperative ascites on survival after surgery for hepatocellular carcinoma: a national study. J Gastrointest Surg 25:2823–2834
Kubo S, Tsukamoto T, Hirohashi K, Tanaka H, Shuto T, Takemura S et al (2004) Correlation between preoperative serum concentration of type IV collagen 7s domain and hepatic failure following resection of hepatocellular carcinoma. Ann Surg 239:186–193
Rosenbaum PR, Rubin DB (1984) Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc 79:516–524
Premkumar M, Anand AC (2022) Overview of complications in cirrhosis. J Clin Exp Hepatol 12:1150–1174
Wang J, Zhang Z, Shang D, Li J, Liu C, Yu P et al (2022) Noninvasively assessed portal hypertension grade predicts post-hepatectomy liver failure in patients with HepatocellCarcinoma: a multicenter study. Front Oncol 12:934870
Yoshino K, Yoh T, Taura K, Seo S, Ciria R, Briceno-Delgado J (2021) A systematic review of prediction models for post-hepatectomy liver failure in patients undergoing liver surgery. HPB (Oxford) 23:1311–1320
Choi SB, Kim HJ, Song TJ, Ahn HS, Choi SY (2014) Influence of clinically significant portal hypertension on surgical outcomes and survival following hepatectomy for hepatocellular carcinoma: a systematic review and meta-analysis. J Hepato-Bil Pancreat Sci 21:639–647
He W, Zeng Q, Zheng Y, Chen M, Shen J, Qiu J et al (2015) The role of clinically significant portal hypertension in hepatic resection for hepatocellular carcinoma patients: a propensity score matching analysis. BMC Cancer 15:263
Westerkamp AC, Lisman T, Porte RJ (2009) How to minimize blood loss during liver surgery in patients with cirrhosis. HPB (Oxford) 11:453–458
Hackl C, Schlitt HJ, Renner P, Lang SA (2016) Liver surgery in cirrhosis and portal hypertension. World J Gastroenterol 22:2725–2735
Miyagi S, Nakanishi C, Hara Y, Kamei T, Kawagishi N, Ohuchi N (2015) An evaluation of the safety of pure laparoscopic hepatectomy in patients with liver cirrhosis: investigations including serum albumin and ascites. Surg Laparosc Endosc Percutan Tech 25:209–211
Han HS, Shehta A, Ahn S, Yoon YS, Cho JY, Choi Y (2015) Laparoscopic versus open liver resection for hepatocellular carcinoma: case-matched study with propensity score matching. J Hepatol 63:643–650
Tanaka S, Kawaguchi Y, Kubo S, Kanazawa A, Takeda Y, Hirokawa F et al (2019) Validation of index-based IWATE criteria as an improved difficulty scoring system for laparoscopic liver resection. Surgery 165:731–740
Fuks D, Cauchy F, Fteriche S, Nomi T, Schwarz L, Dokmak S et al (2016) Laparoscopy decreases pulmonary complications in patients undergoing major liver resection: a propensity score analysis. Ann Surg 263:353–361
Scuderi V, Barkhatov L, Montalti R, Ratti F, Cipriani F, Pardo F et al (2017) Outcome after laparoscopic and open resections of posterosuperior segments of the liver. Br J Surg 104:751–759
Alukal JJ, Thuluvath PJ (2019) Gastrointestinal failure in critically ill patients with cirrhosis. Am J Gastroenterol 114:1231–1237
Xiong JJ, Nunes QM, Huang W, Tan CL, Ke NW, Xie SM et al (2013) Laparoscopic vs open total gastrectomy for gastric cancer: a meta-analysis. World J Gastroenterol 19:8114–8132
Liang W, Li J, Zhang W, Liu J, Li M, Gao Y et al (2019) Prolonged postoperative ileus in gastric surgery: is there any difference between laparoscopic and open surgery? Cancer Med 8:5515–5523
Hajibandeh S, Hajibandeh S, Bill V (2020) Meta-analysis of enhanced recovery after surgery (ERAS) protocols in emergency abdominal surgery. World J Surg 44:1336–1348
Morise Z, Kawabe N, Kawase J, Tomishige H, Nagata H, Ohshima H et al (2013) Pure laparoscopic hepatectomy for hepatocellular carcinoma with chronic liver disease. World J Hepatol 5:487–495
Tranchart H, Di Giuro G, Lainas P, Roudie J, Agostini H, Franco D et al (2010) Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc 24:1170–1176
Troisi RI, Berardi G, Morise Z, Cipriani F, Ariizumi S, Sposito C et al (2021) Laparoscopic and open liver resection for hepatocellular carcinoma with Child–Pugh B cirrhosis: multicentre propensity score-matched study. Br J Surg 108:196–204
Zhu P, Liao W, Zhang WG, Chen L, Shu C, Zhang ZW et al (2023) A Prospective Study Using propensity score matching to compare long-term survival outcomes after robotic-assisted, laparoscopic, or open liver resection for patients with BCLC stage 0-A hepatocellular carcinoma. Ann Surg 277:e103–e111
Rayman S, Sucandy I, Ross SB, Crespo K, Syblis C, Rosemurgy A (2023) A propensity score matched analysis of robotic and open hepatectomy for treatment of liver tumors. Clinical outcomes, oncological survival, and costs comparison. J Robot Surg 17:2399–407
Gumbs AA, Lorenz E, Tsai TJ, Starker L, Flanagan J, Benedetti Cacciaguerra A, Yu NJ, Bajul M, Chouillard E, Croner R, Abu Hilal M (2022) Study: international multicentric minimally invasive liver resection for colorectal liver metastases (SIMMILR-CRLM). Cancers (Basel). https://doi.org/10.3390/cancers14061379
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Hiroji Shinkawa, Masaki Kaibori, Daijiro Kabata, Takuya Nakai, Masaki Ueno, Daisuke Hokuto, Hisashi Ikoma, Hiroya Iida, Koji Komeda, Shogo Tanaka, Hisashi Kosaka, Chihoko Nobori, Shinya Hayami, Satoshi Yasuda, Ryo Morimura, Haruki Mori, Shuji Kagota, Shoji Kubo, and Takeaki Ishizawa have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
464_2023_10591_MOESM1_ESM.tif
Supplementary material 1 (TIF 801 kb) Long-term survival outcomes after liver resection in patients of hepatocellular carcinoma with clinically significant portal hypertension in the entire cohort. (A) Recurrence-free survival rates
464_2023_10591_MOESM2_ESM.tif
Supplementary material 1 (TIF 796 kb) Long-term survival outcomes after liver resection in patients of hepatocellular carcinoma with clinically significant portal hypertension in the entire cohort. (B) Overall survival rates
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shinkawa, H., Kaibori, M., Kabata, D. et al. Laparoscopic and open minor liver resection for hepatocellular carcinoma with clinically significant portal hypertension: a multicenter study using inverse probability weighting approach. Surg Endosc 38, 757–768 (2024). https://doi.org/10.1007/s00464-023-10591-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10591-z