Abstract
Background
Different techniques have been described for esophagojejunostomy (EJ) during laparoscopic total gastrectomy (LTG) for gastric cancer. Linear stapled techniques include overlap (OL) and functional end-to-end anastomosis (FEEA) while single staple technique (SST), hemi-double staple technique (HDST), and OrVil® are circular stapled approaches. Nowadays, the choice among techniques for EJ depends on operating surgeon personal preference.
Purpose
To compare short-term outcomes of different EJ techniques during LTG.
Methods
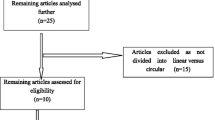
Systematic review and network meta-analysis. OL, FEEA, SST, HDST, and OrVil® were compared. Primary outcomes were anastomotic leak (AL) and stenosis (AS). Risk ratio (RR) and weighted mean difference (WMD) were used as pooled effect size measures, whereas 95% credible intervals (CrI) were used to measure relative inference.
Results
Overall, 3177 patients (20 studies) were included. The technique for EJ was SST (n = 1026; 32.9%), OL (n = 826; 26.5%), FEEA (n = 752; 24.1%), OrVil® (n = 317; 10.1%), and HDST (n = 196; 6.4%). AL was comparable for OL vs. FEEA (RR = 0.82; 95% CrI 0.47–1.49), OL vs. SST (RR = 0.55; 95% CrI 0.27–1.21), OL vs. OrVil® (RR = 0.54; 95% CrI 0.32–1.22), and OL vs. HDST (RR = 0.65; 95% CrI 0.28–1.63). Similarly, AS was similar for OL vs. FEEA (RR = 0.46; 95% CrI 0.18–1.28), OL vs. SST (RR = 0.89; 95% CrI 0.39–2.15), OL vs. OrVil® (RR = 0.36; 95% CrI 0.14–1.02), and OL vs. HDST (RR = 0.61; 95% CrI 0.31–1.21). Anastomotic bleeding, time to soft diet resumption, pulmonary complications, hospital length of stay, and mortality were comparable while operative time was reduced for FEEA.
Conclusions
This network meta-analysis shows similar postoperative AL and AS risk when comparing OL, FEEA, SST, HDST, and OrVil® techniques. Similarly, no differences were found for anastomotic bleeding, operative time, soft diet resumption, pulmonary complications, hospital length of stay and 30-day mortality.
Graphical abstract



Similar content being viewed by others
References
Van Cutsem E, Dicato M, Geva R et al (2011) The diagnosis and management of gastric cancer: expert discussion and recommendations from the 12th ESMO/World congress on gastrointestinal cancer, Barcelona, 2010. Ann Oncol 22(suppl 5):v1-9
Lutz M, Zalcberg J, Ducreux M et al (2012) Highlights of the EORTC St. Gallen international expert consensus on the primary therapy of gastric, gastroesophageal and oesophageal cancer—differential treatment strategies for subtypes of early gastroesophageal cancer. Eur J Cancer 48:2941–2953
Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N, Japanese Laparoscopic Surgery Study Group (2007) A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg 245(1):68–72. https://doi.org/10.1097/01.sla.0000225364.03133.f8
Jeong O, Ryu SY, Zhao XF, Jung MR, Kim KY, Park YK (2012) Short-term surgical outcomes and operative risks of laparoscopic total gastrectomy (LTG) for gastric carcinoma: experience at a large-volume center. Surg Endosc 26(12):3418–3425. https://doi.org/10.1007/s00464-012-2356-7
Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, Cho GS, Kim CY, Yang HK, Park DJ, Song KY, Lee SI, Ryu SY, Lee JH, Lee HJ, Korean Laparo-endoscopic Gastrointestinal Surgery Study (KLASS) Group (2016) Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes From a multicenter randomized controlled trial (KLASS-01). Ann Surg 263(1):28–35. https://doi.org/10.1097/SLA.0000000000001346
Jeong O, Jung MR, Kang JH, Ryu SY (2020) Reduced anastomotic complications with intracorporeal esophagojejunostomy using endoscopic linear staplers (overlap method) in laparoscopic total gastrectomy for gastric carcinoma. Surg Endosc 34(5):2313–2320. https://doi.org/10.1007/s00464-019-07362-0
Sozzi A, Aiolfi A, Matsushima K, Bonitta G, Lombardo F, Viti M, Russo A, Campanelli G, Bona D (2023) Linear- versus circular-stapled esophagojejunostomy during total gastrectomy: systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A 33(6):524–533. https://doi.org/10.1089/lap.2023.0004
Kim DJ, Lee JH, Kim W (2015) Comparison of the major postoperative complications between laparoscopic distal and total gastrectomies for gastric cancer using Clavien-Dindo classification. Surg Endosc 29(11):3196–3204. https://doi.org/10.1007/s00464-014-4053-1
Inokuchi M, Otsuki S, Fujimori Y, Sato Y, Nakagawa M, Kojima K (2015) Systematic review of anastomotic complications of esophagojejunostomy after laparoscopic total gastrectomy. World J Gastroenterol 21(32):9656–9665. https://doi.org/10.3748/wjg.v21.i32.9656
Brenkman HJF, Gisbertz SS, Slaman AE, Goense L, Ruurda JP, van Berge Henegouwen MI, van Hillegersberg R, Dutch Upper Gastrointestinal Cancer Audit (DUCA) group (2017) Postoperative outcomes of minimally invasive gastrectomy versus open gastrectomy during the early introduction of minimally invasive gastrectomy in the Netherlands: a population-based cohort study. Ann Surg 266(5):831–838
Umemura A, Koeda K, Sasaki A, Fujiwara H, Kimura Y, Iwaya T, Akiyama Y, Wakabayashi G (2015) Totally laparoscopic total gastrectomy for gastric cancer: literature review and comparison of the procedure of esophagojejunostomy. Asian J Surg 38(2):102–112. https://doi.org/10.1016/j.asjsur.2014.09.006
Milone M, Elmore U, Manigrasso M, Vertaldi S, Aprea G, Servillo G, Parise P, De Palma GD, Rosati R (2022) Circular versus linear stapling oesophagojejunostomy after laparoscopic total gastrectomy. A systematic review and meta-analysis. Am J Surg 223(5):884–892. https://doi.org/10.1016/j.amjsurg.2021.09.024
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Goossen K, Tenckhoff S, Probst P, Grummich K, Mihaljevic AL, Büchler MW, Diener MK (2018) Optimal literature search for systematic reviews in surgery. Langenbecks Arch Surg 403(1):119–129. https://doi.org/10.1007/s00423-017-1646-x
Sterne JA, Hernan MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. https://doi.org/10.1136/bmj.i4919
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group; Cochrane Statistical Methods Group (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 18(343):d5928. https://doi.org/10.1136/bmj.d5928
DerSimonian R, Laird N (2015) Meta-analysis in clinical trials revisited. Contemp Clin Trials 45(Pt A):139–145. https://doi.org/10.1016/j.cct.2015.09.002
Borenstein M, Hedges LV, Higgins JP, Rothstein HR (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 1(2):97–111. https://doi.org/10.1002/jrsm.12
Aiolfi A, Tornese S, Bonitta G, Rausa E, Micheletto G, Bona D (2019) Roux-en-Y gastric bypass: systematic review and Bayesian network meta-analysis comparing open, laparoscopic, and robotic approach. Surg Obes Relat Dis 15(6):985–994. https://doi.org/10.1016/j.soard.2019.03.006
Kass RE, Wasserman L (1995) A Reference Bayesian test for nested hypotheses and its relationship to the Schwarz Criterion. J Am Stat Assoc 90(431):928–934. https://doi.org/10.1080/01621459.1995.10476592
Friede T, Röver C, Wandel S, Neuenschwander B (2017) Meta-analysis of few small studies in orphan diseases. Res Synth Methods 8(1):79–91. https://doi.org/10.1002/jrsm.1217
Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JP (2012) Predicting the extent of heterogeneity in meta-analysis, using empirical data from the Cochrane database of systematic reviews. Int J Epidemiol 41(3):818–827. https://doi.org/10.1093/ije/dys041
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Smith BJ (2007) Boa: an R package for MCMC output convergence assessment and posterior inference. J Stat Softw 21:1–37. https://doi.org/10.18637/jss.v021.i11
Aiolfi A, Bona D, Riva CG, Micheletto G, Rausa E, Campanelli G, Olmo G, Bonitta G, Bonavina L (2020) Systematic review and Bayesian network Meta-analysis comparing laparoscopic Heller myotomy, pneumatic dilatation, and peroral endoscopic myotomy for esophageal achalasia. J Laparoendosc Adv Surg Tech A 30(2):147–155. https://doi.org/10.1089/lap.2019.0432
Dias S, Welton NJ, Caldwell DM, Ades AE (2010) Checking consistency in mixed treatment comparison meta-analysis. Stat Med 29(7–8):932–944. https://doi.org/10.1002/sim.3767
Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JP (2014) Evaluating the quality of evidence from a network meta-analysis. PLoS ONE 9(7):e99682. https://doi.org/10.1371/journal.pone.0099682
R Core Team. R: A language and environment for statistical computing. R foundation for statistical computing. Vienna
Cianchi F, Macrì G, Indennitate G, Mallardi B, Trallori G, Biagini MR, Badii B, Staderini F, Perigli G (2014) Laparoscopic total gastrectomy using the transorally inserted anvil (OrVil™): a preliminary, single institution experience. Springerplus 14(3):434. https://doi.org/10.1186/2193-1801-3-434
Kosuga T, Hiki N, Nunobe S, Ohashi M, Kubota T, Kamiya S, Sano T, Yamaguchi T (2015) Does the single-stapling technique for circular-stapled esophagojejunostomy reduce anastomotic complications after laparoscopic total gastrectomy? Ann Surg Oncol 22(11):3606–3612. https://doi.org/10.1245/s10434-015-4417-3
Wang H, Hao Q, Wang M, Feng M, Wang F, Kang X, Guan WX (2015) Esophagojejunostomy after laparoscopic total gastrectomy by OrVil™ or hemi-double stapling technique. World J Gastroenterol 21(29):8943–8951. https://doi.org/10.3748/wjg.v21.i29.8943
Kim EY, Choi HJ, Cho JB, Lee J (2016) Totally laparoscopic total gastrectomy versus laparoscopically assisted total gastrectomy for gastric cancer. Anticancer Res 36(4):1999–2003
Lu X, Hu Y, Liu H, Mou T, Deng Z, Wang D, Yu J, Li G (2016) Short-term outcomes of intracorporeal esophagojejunostomy using the transorally inserted anvil versus extracorporeal circular anastomosis during laparoscopic total gastrectomy for gastric cancer: a propensity score matching analysis. J Surg Res 200(2):435–443. https://doi.org/10.1016/j.jss.2015.08.013
Umemura A, Koeda K, Fujiwara H, Chiba T, Otsuka K, Sasaki A (2016) Totally laparoscopic total gastrectomy for gastric cancer at a single institutional experience and changes in technique of esophagojejunostomy. Indian J Surg 78(3):249–253. https://doi.org/10.1007/s12262-016-1471-4
Gong CS, Kim BS, Kim HS (2017) Comparison of totally laparoscopic total gastrectomy using an endoscopic linear stapler with laparoscopic-assisted total gastrectomy using a circular stapler in patients with gastric cancer: a single-center experience. World J Gastroenterol 23(48):8553–8561. https://doi.org/10.3748/wjg.v23.i48.8553
Kawamura H, Ohno Y, Ichikawa N, Yoshida T, Homma S, Takahashi M, Taketomi A (2017) Anastomotic complications after laparoscopic total gastrectomy with esophagojejunostomy constructed by circular stapler (OrVil™) versus linear stapler (overlap method). Surg Endosc 31(12):5175–5182. https://doi.org/10.1007/s00464-017-5584-z
Miura S, Kanaya S, Hosogi H, Kawada H, Akagawa S, Shimoike N, Okumura S, Okada T, Ito T, Arimoto A (2017) Esophagojejunostomy with linear staplers in laparoscopic total gastrectomy: experience with 168 cases in 5 consecutive years. Surg Laparosc Endosc Percutan Tech 27(5):e101–e107. https://doi.org/10.1097/SLE.0000000000000464
Sugiyama M, Oki E, Ogaki K, Morita M, Sakaguchi Y, Koga S, Saeki H, Maehara Y (2017) Clinical outcomes of esophagojejunostomy in totally laparoscopic total gastrectomy: a multicenter study. Surg Laparosc Endosc Percutan Tech 27(4):e87–e91. https://doi.org/10.1097/SLE.0000000000000435
Yoshikawa K, Shimada M, Higashijima J, Tokunaga T, Nishi M, Takasu C, Kashihara H, Ishikawa D (2018) Usefulness of the transoral anvil delivery system for esophagojejunostomy after laparoscopic total gastrectomy: a single-institution comparative study of transoral anvil delivery system and the overlap method. Surg Laparosc Endosc Percutan Tech 28(2):e40–e43. https://doi.org/10.1097/SLE.0000000000000495
Kang SH, Cho YS, Min SH, Park YS, Ahn SH, Park DJ, Kim HH (2019) Intracorporeal esophagojejunostomy using a circular or a linear stapler in totally laparoscopic total gastrectomy: a propensity-matched analysis. J Gastric Cancer 19(2):193–201. https://doi.org/10.5230/jgc.2019.19.e17
Park KB, Kim EY, Song KY (2019) Esophagojejunal anastomosis after laparoscopic total gastrectomy for gastric cancer: circular versus linear stapling. J Gastric Cancer 19(3):344–354. https://doi.org/10.5230/jgc.2019.19.e34
Chen XH, Hu YF, Luo J, Chen YH, Liu H, Lin T, Chen H, Li GX, Yu J (2019) The safety of esophagojejunostomy via a transorally inserted-anvil method vs extracorporeal anastomosis using a circular stapler during total gastrectomy for Siewert type 2 adenocarcinoma of the esophagogastric junction. Gastroenterol Rep (Oxf) 8(3):242–251. https://doi.org/10.1093/gastro/goz046
Lee S, Lee H, Song JH, Choi S, Cho M, Son T, Kim HI, Hyung WJ (2020) Intracorporeal esophagojejunostomy using a linear stapler in laparoscopic total gastrectomy: comparison with circular stapling technique. BMC Surg 20(1):100. https://doi.org/10.1186/s12893-020-00746-3
Wang Z, Liu X, Cheng Q, Wei Y, Li Z, Zhu G, Li Y, Wang K (2021) Digestive tract reconstruction of laparoscopic total gastrectomy for gastric cancer: a comparison of the intracorporeal overlap, intracorporeal hand-sewn anastomosis, and extracorporeal anastomosis. J Gastrointest Oncol 12(3):1031–1041. https://doi.org/10.21037/jgo-21-231
Wei M, Wang N, Yin Z, Wu T, Zhou S, Dang L, Zhang Z, Wu D, Gao P, Zhang B, Yang Y, Jia G, Wang K, Qiao Q, He X (2021) Short-term and quality of life outcomes of patients using linear or circular stapling in esophagojejunostomy after laparoscopic total gastrectomy. J Gastrointest Surg 25(7):1667–1676. https://doi.org/10.1007/s11605-020-04806-0
Yang HK, Hyung WJ, Han SU, Lee YJ, Park JM, Cho GS, Kwon OK, Kong SH, Kim HI, Lee HJ, Kim W, Ryu SW, Jin SH, Oh SJ, Ryu KW, Kim MC, Ahn HS, Park YK, Kim YH, Hwang SH, Kim JW, Kim JJ (2021) Comparison of surgical outcomes among different methods of esophagojejunostomy in laparoscopic total gastrectomy for clinical stage I proximal gastric cancer: results of a single-arm multicenter phase II clinical trial in Korea, KLASS 03. Surg Endosc 35(3):1156–1163. https://doi.org/10.1007/s00464-020-07480-0
Ebihara Y, Kurashima Y, Tanaka K, Nakanishi Y, Asano T, Noji T, Nakamura T, Murakami S, Tsuchikawa T, Okamura K, Murakami Y, Murakawa K, Nakamura F, Morita T, Okushiba S, Shichinohe T, Hirano S (2021) A multicenter retrospective study comparing surgical outcomes between the overlap method and functional method for esophagojejunostomy in laparoscopic total gastrectomy: analysis using propensity score matching. Surg Laparosc Endosc Percutan Tech 32(1):89–95. https://doi.org/10.1097/SLE.0000000000001008
Aiolfi A, Lombardo F, Matsushima K, Sozzi A, Cavalli M, Panizzo V, Bonitta G, Bona D (2021) Systematic review and updated network meta-analysis of randomized controlled trials comparing open, laparoscopic-assisted, and robotic distal gastrectomy for early and locally advanced gastric cancer. Surgery 170(3):942–951. https://doi.org/10.1016/j.surg.2021.04.014
Hiki N (2013) Present features and future vision of laparoscopy-assisted total gastrectomy (LATG). Gastric Cancer 16(4):460–461. https://doi.org/10.1007/s10120-013-0286-2
Lee SE, Ryu KW, Nam BH, Lee JH, Kim YW, Yu JS, Cho SJ, Lee JY, Kim CG, Choi IJ, Kook MC, Park SR, Kim MJ, Lee JS (2009) Technical feasibility and safety of laparoscopy-assisted total gastrectomy in gastric cancer: a comparative study with laparoscopy-assisted distal gastrectomy. J Surg Oncol 100(5):392–395. https://doi.org/10.1002/jso.21345
Inaba K, Satoh S, Ishida Y, Taniguchi K, Isogaki J, Kanaya S, Uyama I (2010) Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg 211(6):e25–e29. https://doi.org/10.1016/j.jamcollsurg.2010.09.005
Matsui H, Uyama I, Sugioka A, Fujita J, Komori Y, Ochiai M, Hasumi A (2002) Linear stapling forms improved anastomoses during esophagojejunostomy after a total gastrectomy. Am J Surg 184(1):58–60. https://doi.org/10.1016/s0002-9610(02)00893-0
Ebihara Y, Okushiba S, Kawarada Y, Kitashiro S, Katoh H (2013) Outcome of functional end-to-end esophagojejunostomy in totally laparoscopic total gastrectomy. Langenbecks Arch Surg 398(3):475–479. https://doi.org/10.1007/s00423-013-1051-z
Aiolfi A, Sozzi A, Bonitta G, Lombardo F, Cavalli M, Cirri S, Campanelli G, Danelli P, Bona D (2022) Linear- versus circular-stapled esophagogastric anastomosis during esophagectomy: systematic review and meta-analysis. Langenbecks Arch Surg 407(8):3297–3309. https://doi.org/10.1007/s00423-022-02706-2
Usui S, Nagai K, Hiranuma S, Takiguchi N, Matsumoto A, Sanada K (2008) Laparoscopy-assisted esophagoenteral anastomosis using endoscopic purse-string suture instrument “Endo-PSI (II)” and circular stapler. Gastric Cancer 11(4):233–237. https://doi.org/10.1007/s10120-008-0481-8
Jeong O, Park YK (2009) Intracorporeal circular stapling esophagojejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc 23(11):2624–2630. https://doi.org/10.1007/s00464-009-0461-z
Sakuramoto S, Kikuchi S, Futawatari N, Moriya H, Katada N, Yamashita K, Watanabe M (2010) Technique of esophagojejunostomy using transoral placement of the pretilted anvil head after laparoscopic gastrectomy for gastric cancer. Surgery 147(5):742–747. https://doi.org/10.1016/j.surg.2009.06.016
Kunisaki C, Makino H, Oshima T, Fujii S, Kimura J, Takagawa R, Kosaka T, Akiyama H, Morita S, Endo I (2011) Application of the transorally inserted anvil (OrVil) after laparoscopy-assisted total gastrectomy. Surg Endosc 25(4):1300–1305. https://doi.org/10.1007/s00464-010-1367-5
Sierzega M, Kolodziejczyk P, Kulig J, Polish Gastric Cancer Study Group (2010) Impact of anastomotic leakage on long-term survival after total gastrectomy for carcinoma of the stomach. Br J Surg 97(7):1035–1042. https://doi.org/10.1002/bjs.7038
Kamarajah SK, Navidi M, Griffin SM, Phillips AW (2020) Impact of anastomotic leak on long-term survival in patients undergoing gastrectomy for gastric cancer. Br J Surg 107(12):1648–1658. https://doi.org/10.1002/bjs.11749
Oshi M, Kunisaki C, Miyamoto H, Kosaka T, Akiyama H, Endo I (2018) Risk factors for anastomotic leakage of esophagojejunostomy after Laparoscopy-assisted total gastrectomy for gastric cancer. Dig Surg 35(1):28–34. https://doi.org/10.1159/000464357
Trapani R, Rausei S, Reddavid R, Degiuli M, ITALIAN RESEARCH GROUP FOR GASTRIC CANCER (GIRCG) Clinical Investigators (2020) Risk factors for esophago-jejunal anastomosis leakage after total gastrectomy for cancer. A multicenter retrospective study of the Italian research group for gastric cancer. Eur J Surg Oncol 46(12):2243–2247. https://doi.org/10.1016/j.ejso.2020.06.035
Zuiki T, Hosoya Y, Kaneda Y, Kurashina K, Saito S, Ui T, Haruta H, Hyodo M, Sata N, Lefor AT, Yasuda Y (2013) Stenosis after use of the double-stapling technique for reconstruction after laparoscopy-assisted total gastrectomy. Surg Endosc 27(10):3683–3689. https://doi.org/10.1007/s00464-013-2945-0
Liao GQ, Ou XW, Liu SQ, Zhang SR, Huang W (2013) Laparoscopy-assisted total gastrectomy with trans-orally inserted anvil (OrVil™): a single institution experience. World J Gastroenterol 19(5):755–760. https://doi.org/10.3748/wjg.v19.i5.755
Shimoike N, Nishigori T, Yamashita Y, Kondo M, Manaka D, Kadokawa Y, Itami A, Kanaya S, Hosogi H, Satoh S, Hata H, Kan T, Kawada H, Yamamoto M, Tanaka E, Tsunoda S, Hisamori S, Hida K, Ueno K, Tanaka S, Obama K, Kyoto Esophageal and Gastric Surgery Study Group (2022) Safety assessment of robotic gastrectomy and analysis of surgical learning process: a multicenter cohort study. Gastric Cancer 25(4):817–826
Omori T, Yamamoto K, Hara H, Shinno N, Yamamoto M, Fujita K, Kanemura T, Takeoka T, Akita H, Wada H, Yasui M, Matsuda C, Nishimura J, Fujiwara Y, Miyata H, Ohue M, Sakon M (2022) Comparison of robotic gastrectomy and laparoscopic gastrectomy for gastric cancer: a propensity score-matched analysis. Surg Endosc 36(8):6223–6234
Acknowledgments
The article has been supported by AIRES (Associazione Italiana Ricerca ESofago).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs Alberto Aiolfi, Andrea Sozzi, Gianluca Bonitta, Francesca Lombardo, Marta Cavalli, Giampiero Campanelli, Luigi Bonavina, and Davide Bona have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
464_2023_10231_MOESM1_ESM.tiff
Supplementary file1 (TIFF 112 KB)— Risk of bias for Randomized Controlled Trials (RCT) was assessed with use of the Cochrane risk-of-bias tool. Green circle: Low risk of Bias. Red circle: High Risk of Bias. Yellow circle: Unclear Risk of Bias.
464_2023_10231_MOESM2_ESM.tiff
Supplementary file2 (TIFF 53 KB)— The Ranking plot applied to the five surgical treatments illustrating the empirical probability that each treatment is ranked 1st through 5th (left to right). The abscissa axis shows the different treatments. The ordinate axis shows the probability (%) of ranking better (higher rankings associated with smaller outcomes values); A: anastomotic leak; B anastomotic stenosis
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aiolfi, A., Sozzi, A., Bonitta, G. et al. Short-term outcomes of different esophagojejunal anastomotic techniques during laparoscopic total gastrectomy: a network meta-analysis. Surg Endosc 37, 5777–5790 (2023). https://doi.org/10.1007/s00464-023-10231-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10231-6