Abstract
Background
The major treatment for perforated peptic ulcers (PPU) is surgery. It remains unclear which patient may not get benefit from surgery due to comorbidity. This study aimed to generate a scoring system by predicting mortality for patients with PPU who received non-operative management (NOM) and surgical treatment.
Method
We extracted the admission data of adult (≥ 18 years) patients with PPU disease from the NHIRD database. We randomly divided patients into 80% model derivation and 20% validation cohorts. Multivariate analysis with a logistic regression model was applied to generate the scoring system, PPUMS. We then apply the scoring system to the validation group.
Result
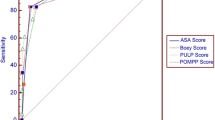
The PPUMS score ranged from 0 to 8 points, composite with age (< 45: 0 points, 45–65: 1 point, 65–80: 2 points, > 80: 3 points), and five comorbidities (congestive heart failure, severe liver disease, renal disease, history of malignancy, and obesity: 1 point each). The areas under ROC curve were 0.785 and 0.787 in the derivation and validation groups. The in-hospital mortality rates in the derivation group were 0.6% (0 points), 3.4% (1 point), 9.0% (2 points), 19.0% (3 points), 30.2% (4 points), and 45.9% when PPUMS > 4 point. Patients with PPUMS > 4 had a similar in-hospital mortality risk between the surgery group [laparotomy: odds ratio (OR) = 0.729, p = 0.320, laparoscopy: OR = 0.772, p = 0.697] and the non-surgery group. We identified similar results in the validation group.
Conclusion
PPUMS scoring system effectively predicts in-hospital mortality for perforated peptic ulcer patients. It factors in age and specific comorbidities is highly predictive and well-calibrated with a reliable AUC of 0.785–0.787. Surgery, no matter laparotomy or laparoscope, significantly reduced mortality for scores < = 4. However, patients with a score > 4 did not show this difference, calling for tailored approaches to treatment based on risk assessment. Further prospective validation is suggested.

Similar content being viewed by others
Data availability
This study is based in part on data from the National Health Insurance Research Database (NHIRD), provided by the National Health Insurance Administration of the Ministry of Health and Welfare and managed by the National Health Research Institutes (registration number NHIRD-103-246). The data utilized in this study cannot be made available in the manuscript, supplemental files, or in a public repository due to the “Personal Information Protection Act” executed by Taiwan’s government, which took effect in 2012. Requests for data can be sent as a formal proposal to the NHIRD (http://nhird.nhri.org.tw) or via email to nhird@nhri.org.tw.
References
Welch CE, Rodkey GV, von Ryll GP (1986) A thousand operations for ulcer disease. Ann Surg 204:454–467
Lau JY, Sung J, Hill C, Henderson C, Howden CW, Metz DC (2011) Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality. Digestion 84:102–113
Soreide K, Thorsen K, Harrison EM, Bingener J, Moller MH, Ohene-Yeboah M, Soreide JA (2015) Perforated peptic ulcer. Lancet 386:1288–1298
Lee CW, Sarosi GA Jr (2011) Emergency ulcer surgery. Surg Clin North Am 91:1001–1013
Moller MH, Adamsen S, Thomsen RW, Moller AM, Peptic Ulcer Perforation trial group (2011) Multicentre trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation. Br J Surg 98:802–810
Kim JM, Jeong SH, Lee YJ, Park ST, Choi SK, Hong SC, Jung EJ, Ju YT, Jeong CY, Ha WS (2012) Analysis of risk factors for postoperative morbidity in perforated peptic ulcer. J Gastric Cancer 12:26–35
Moller MH, Engebjerg MC, Adamsen S, Bendix J, Thomsen RW (2012) The peptic ulcer perforation (PULP) score: a predictor of mortality following peptic ulcer perforation A cohort study. Acta Anaesthesiol Scand 56:655–662
Crofts TJ, Park KG, Steele RJ, Chung SS, Li AK (1989) A randomized trial of non-operative treatment for perforated peptic ulcer. N Engl J Med 320:970–973
Tarasconi A, Coccolini F, Biffl WL, Tomasoni M, Ansaloni L, Picetti E, Molfino S, Shelat V, Cimbanassi S, Weber DG, Abu-Zidan FM, Campanile FC, Di Saverio S, Baiocchi GL, Casella C, Kelly MD, Kirkpatrick AW, Leppaniemi A, Moore EE, Peitzman A, Fraga GP, Ceresoli M, Maier RV, Wani I, Pattonieri V, Perrone G, Velmahos G, Sugrue M, Sartelli M, Kluger Y, Catena F (2020) Perforated and bleeding peptic ulcer: WSES guidelines. World J Emerg Surg 15:3
Oida T, Kano H, Mimatsu K, Kawasaki A, Kuboi Y, Fukino N, Kida K, Amano S (2012) Percutaneous drainage in conservative therapy for perforated gastroduodenal ulcers. Hepatogastroenterology 59:168–170
Songne B, Jean F, Foulatier O, Khalil H, Scotte M (2004) Non operative treatment for perforated peptic ulcer: results of a prospective study. Ann Chir 129:578–582
Tanaka R, Kosugi S, Sakamoto K, Yajima K, Ishikawa T, Kanda T, Wakai T (2013) Treatment for perforated gastric ulcer: a multi-institutional retrospective review. J Gastrointest Surg 17:2074–2081
Bucher P, Oulhaci W, Morel P, Ris F, Huber O (2007) Results of conservative treatment for perforated gastroduodenal ulcers in patients not eligible for surgical repair. Swiss Med Wkly 137:337–340
Lay PL, Huang HH, Chang WK, Hsieh TY, Huang TY, Lin HH (2016) Outcome of nonsurgical intervention in patients with perforated peptic ulcers. Am J Emerg Med 34:1556–1560
Alizadeh N, Buhler L, Huber O, Morel P (1997) Conservative treatment of gastroduodenal peptic ulcer perforations: indications and results. Schweiz Med Wochenschr Suppl 89:17S-19S
Bergamaschi R, Marvik R, Johnsen G, Thoresen JE, Ystgaard B, Myrvold HE (1999) Open vs laparoscopic repair of perforated peptic ulcer. Surg Endosc 13:679–682
Bertleff MJ, Lange JF (2010) Laparoscopic correction of perforated peptic ulcer: first choice? A review of literature. Surg Endosc 24:1231–1239
Leusink A, Markar SR, Wiggins T, Mackenzie H, Faiz O, Hanna GB (2018) Laparoscopic surgery for perforated peptic ulcer: an English national population-based cohort study. Surg Endosc 32:3783–3788
Lohsiriwat V, Prapasrivorakul S, Lohsiriwat D (2009) Perforated peptic ulcer: clinical presentation, surgical outcomes, and the accuracy of the Boey scoring system in predicting postoperative morbidity and mortality. World J Surg 33:80–85
Agarwal A, Jain S, Meena LN, Jain SA, Agarwal L (2015) Validation of Boey’s score in predicting morbidity and mortality in peptic perforation peritonitis in Northwestern India. Trop Gastroenterol 36:256–260
Huang KW, Luo JC, Leu HB, Lin HC, Lee FY, Chan WL, Lin SJ, Chen JW, Chang FY (2012) Chronic obstructive pulmonary disease: an independent risk factor for peptic ulcer bleeding: a nationwide population-based study. Aliment Pharmacol Ther 35:796–802
Johnston LE, Grimm JC, Magruder JT, Shah AS (2016) Development of a transplantation risk index in patients with mechanical circulatory support: a decision support tool. JACC Heart failure 4:277–286
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Austin PC, Lee DS, D’Agostino RB, Fine JP (2016) Developing points-based risk-scoring systems in the presence of competing risks. Stat Med 35:4056–4072
Lin SW, Chen CY, Su YC, Wu KT, Yu PC, Yen YC, Chen JH (2022) Mortality prediction model before surgery for acute mesenteric infarction: a population-based study. J Clin Med. https://doi.org/10.3390/jcm11195937
Bin-Taleb AK, Razzaq RA, Al-Kathiri ZO (2008) Management of perforated peptic ulcer in patients at a teaching hospital. Saudi Med J 29:245–250
Blomgren LG (1997) Perforated peptic ulcer: long-term results after simple closure in the elderly. World J Surg 21:412–414
Daniel VT, Wiseman JT, Flahive J, Santry HP (2017) Predictors of mortality in the elderly after open repair for perforated peptic ulcer disease. J Surg Res 215:108–113
Seow JG, Lim YR, Shelat VG (2017) Low serum albumin may predict the need for gastric resection in patients with perforated peptic ulcer. Eur J Trauma Emerg Surg 43:293–298
Sillakivi T, Lang A, Tein A, Peetsalu A (2000) Evaluation of risk factors for mortality in surgically treated perforated peptic ulcer. Hepatogastroenterology 47:1765–1768
Bas G, Eryilmaz R, Okan I, Sahin M (2008) Risk factors of morbidity and mortality in patients with perforated peptic ulcer. Acta Chir Belg 108:424–427
Soreide K, Thorsen K, Soreide JA (2014) Strategies to improve the outcome of emergency surgery for perforated peptic ulcer. Br J Surg 101:e51-64
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Lemeshow S, Teres D, Klar J, Avrunin JS, Gehlbach SH, Rapoport J (1993) Mortality probability models (MPM II) based on an international cohort of intensive care unit patients. JAMA 270:2478–2486
Li YT, Wang YC, Yang SF, Law YY, Shiu BH, Chen TA, Wu SC, Lu MC (2022) Risk factors and prognoses of invasive Candida infection in surgical critical ill patients with perforated peptic ulcer. J Microbiol Immunol Infect 55:740–748
Li CH, Bair MJ, Chang WH, Shih SC, Lin SC, Yeh CY (2009) Predictive model for length of hospital stay of patients surviving surgery for perforated peptic ulcer. J Formos Med Assoc 108:644–652
Copeland GP, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78:355–360
Thorsen K, Soreide JA, Soreide K (2014) What is the best predictor of mortality in perforated peptic ulcer disease? A population-based, multivariable regression analysis including three clinical scoring systems. J Gastrointest Surg 18:1261–1268
Bharadwaj S, Ginoya S, Tandon P, Gohel TD, Guirguis J, Vallabh H, Jevenn A, Hanouneh I (2016) Malnutrition: laboratory markers vs nutritional assessment. Gastroenterol Rep (Oxf) 4:272–280
Soeters PB, Wolfe RR, Shenkin A (2019) Hypoalbuminemia: pathogenesis and clinical significance. JPEN J Parenter Enteral Nutr 43:181–193
Andersen CJ, Murphy KE, Fernandez ML (2016) Impact of obesity and metabolic syndrome on immunity. Adv Nutr 7:66–75
Wang HE, Griffin R, Judd S, Shapiro NI, Safford MM (2013) Obesity and risk of sepsis: a population-based cohort study. Obesity (Silver Spring) 21:E762-769
Winfield RD, Reese S, Bochicchio K, Mazuski JE, Bochicchio GV (2016) Obesity and the risk for surgical site infection in abdominal surgery. Am Surg 82:331–336
Kaspersen KA, Pedersen OB, Petersen MS, Hjalgrim H, Rostgaard K, Moller BK, Juul-Sorensen C, Kotze S, Dinh KM, Erikstrup LT, Sorensen E, Thorner LW, Burgdorf KS, Ullum H, Erikstrup C (2015) Obesity and risk of infection: results from the Danish Blood Donor Study. Epidemiology 26:580–589
Carbone F, La Rocca C, De Candia P, Procaccini C, Colamatteo A, Micillo T, De Rosa V, Matarese G (2016) Metabolic control of immune tolerance in health and autoimmunity. Semin Immunol 28:491–504
Naylor C, Petri WA Jr (2016) Leptin regulation of immune responses. Trends Mol Med 22:88–98
Thorsen K, Glomsaker TB, von Meer A, Soreide K, Soreide JA (2011) Trends in diagnosis and surgical management of patients with perforated peptic ulcer. J Gastrointest Surg 15:1329–1335
Siow SL, Mahendran HA, Wong CM, Hardin M, Luk TL (2018) Laparoscopic versus open repair of perforated peptic ulcer: Improving outcomes utilizing a standardized technique. Asian J Surg 41:136–142
Tan S, Wu G, Zhuang Q, Xi Q, Meng Q, Jiang Y, Han Y, Yu C, Yu Z, Li N (2016) Laparoscopic versus open repair for perforated peptic ulcer: a meta analysis of randomized controlled trials. Int J Surg 33:124–132
Rahman MM, Islam MS, Flora S, Akhter SF, Hossain S, Karim F (2007) Mortality in perforated peptic ulcer patients after selective management of stratified poor risk cases. World J Surg 31:2341–2344
Gouta EL, Dougaz W, Khalfallah M, Bouasker I, Dziri C (2018) Management of perforated duodenal peptic ulcer treated by suture. Tunis Med 96:424–429
Alemrajabi M, Safari S, Tizmaghz A, Alemrajabi F, Shabestanipour G (2016) Laparoscopic repair of perforated peptic ulcer: outcome and associated morbidity and mortality. Electron Physician 8:2543–2545
Manco G, Caramaschi S, Rolando G, Malagoli M, Zanelli G, Reggiani Bonetti L, Rossi A (2020) Primary laparoscopic approach to repair perforated peptic ulcer. A retrospective cohort study. Minerva Chir. https://doi.org/10.23736/S0026-4733.20.08287-5
Zimmermann M, Hoffmann M, Laubert T, Jung C, Bruch HP, Schloericke E (2015) Conversion of laparoscopic surgery for perforated peptic ulcer: a single-center study. Surg Today 45:1421–1428
Lau H (2004) Laparoscopic repair of perforated peptic ulcer: a meta-analysis. Surg Endosc 18:1013–1021
Vaidya BB, Garg CP, Shah JB (2009) Laparoscopic repair of perforated peptic ulcer with delayed presentation. J Laparoendosc Adv Surg Tech A 19:153–156
Guadagni S, Cengeli I, Galatioto C, Furbetta N, Piero VL, Zocco G, Seccia M (2014) Laparoscopic repair of perforated peptic ulcer: single-center results. Surg Endosc 28:2302–2308
Zogovic S, Bojesen AB, Andos S, Mortensen FV (2019) Laparoscopic repair of perforated peptic ulcer is not prognostic factor for 30-day mortality (a nationwide prospective cohort study). Int J Surg 72:47–54
Smith RS, Sundaramurthy SR, Croagh D (2019) Laparoscopic versus open repair of perforated peptic ulcer: a retrospective cohort study. Asian J Endosc Surg 12:139–144
Karabulut K, Dincer M, Liman RK, Usta S (2019) Non-operative management of perforated peptic ulcer: a single-center experience. Ulus Travma Acil Cerrahi Derg 25:585–588
Acknowledgements
The authors would like to thank Dr. Yaw-Sen Chen, Division of General Surgery, E-Da Hospital, and Dr. Chao-Ming Hung, Division of General Surgery, E-Da Cancer Hospital for their assistance. We are grateful to the grant support of E-Da Hospital, Taiwan, and IRB (EDAHI-109-001, EDAHI-110-003, EDAHC-111-007, EDAHP-112-005, EDAHC-112-001).
Author information
Authors and Affiliations
Contributions
JHC, YKH, CYC, KTW: conceptualization; JHC, CYC: methodology; JHC: software; JHC, CYC: validation; JHC, YKH, KTW: formal analysis; JHC: resources; JHC: data curation; YKH, YSS: writing (original draft); JHC, YKH, KTW: preparing tables and figures and visualization; YKH, JHC: project administration.
Corresponding author
Ethics declarations
Disclosures
Yi-Kai Huang, Kun-Ta Wu, Yi-Shan Su, Chung-Yen Chen and Jian-Han Chen declare no competing interests and nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, YK., Wu, KT., Su, YS. et al. Predicting in-hospital mortality risk for perforated peptic ulcer surgery: the PPUMS scoring system and the benefit of laparoscopic surgery: a population-based study. Surg Endosc 37, 6834–6843 (2023). https://doi.org/10.1007/s00464-023-10180-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10180-0