Abstract
Background
The purposes of this study were to determine clinical presentations and surgical outcomes of perforated peptic ulcer (PPU), and to evaluate the accuracy of the Boey scoring system in predicting mortality and morbidity.
Methods
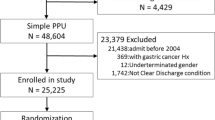
We carried out a retrospective study of patients undergoing emergency surgery for PPU between 2001 and 2006 in a university hospital. Clinical presentations and surgical outcomes were analyzed. Adjusted odds ratio (OR) of each Boey score on morbidity and mortality rate was compared with zero risk score. Receiver-operating characteristic curve analysis was used to compare the predictive ability between Boey score, American Society of Anesthesiologists (ASA) classification, and Mannheim Peritonitis Index (MPI).
Results
The study included 152 patients with average age of 52 years (range: 15–88 years), and 78% were male. The most common site of PPU was the prepyloric region (74%). Primary closure and omental graft was the most common procedure performed. Overall mortality rate was 9% and the complication rate was 30%. The mortality rate increased progressively with increasing numbers of the Boey score: 1%, 8% (OR = 2.4), 33% (OR = 3.5), and 38% (OR = 7.7) for 0, 1, 2, and 3 scores, respectively (p < 0.001). The morbidity rates for 0, 1, 2, and 3 Boey scores were 11%, 47% (OR = 2.9), 75% (OR = 4.3), and 77% (OR = 4.9), respectively (p < 0.001). Boey score and ASA classification appeared to be better than MPI for predicting the poor surgical outcomes.
Conclusions
Perforated peptic ulcer is associated with high rates of mortality and morbidity. The Boey risk score serves as a simple and precise predictor for postoperative mortality and morbidity.
Similar content being viewed by others
References
Behrman SW (2005) Management of complicated peptic ulcer disease. Arch Surg 140:201–208
Ng EK, Chung SC, Sung JJ et al (1996) High prevalence of Helicobacter pylori infection in duodenal ulcer perforations not caused by non-steroidal anti-inflammatory drugs. Br J Surg 83:1779–1781
Kate V, Ananthakrishnan N, Badrinath S (2001) Effect of Helicobacter pylori eradication on the ulcer recurrence rate after simple closure of perforated duodenal ulcer: retrospective and prospective randomized controlled studies. Br J Surg 88:1054–1058
Ng EK, Lam YH, Sung JJ et al (2000) Eradication of Helicobacter pylori prevents recurrence of ulcer after simple closure of duodenal ulcer perforation: randomized controlled trial. Ann Surg 231:153–158
Rix TE, Bates T (2007) Pre-operative risk scores for the prediction of outcome in elderly people who require emergency surgery. World J Emerg Surg 2:16
Boey J, Choi SK, Poon A et al (1987) Risk stratification in perforated duodenal ulcers. A prospective validation of predictive factors. Ann Surg 205:22–26
Lee FY, Leung KL, Lai BS et al (2001) Predicting mortality and morbidity of patients operated on for perforated peptic ulcers. Arch Surg 136:90–94
Linder MM, Wacha H, Feldmann U et al (1987) The Mannheim Peritonitis Index. An instrument for the intraoperative prognosis of peritonitis. Chirurg 58:84–92
Notash AY, Salimi J, Rahimian H et al (2005) Evaluation of Mannheim Peritonitis Index and multiple organ failure score in patients with peritonitis. Indian J Gastroenterol 24:197–200
Schein M, Gecelter G, Freinkel Z et al (1990) APACHE II in emergency operations for perforated ulcers. Am J Surg 159:309–313
Mishra A, Sharma D, Raina VK (2003) A simplified prognostic scoring system for peptic ulcer perforation in developing countries. Indian J Gastroenterol 22:49–53
Arici C, Mesci A, Dincer D et al (2007) Analysis of risk factors predicting (affecting) mortality and morbidity of peptic ulcer perforations. Int Surg 92:147–154
Makela JT, Kiviniemi H, Ohtonen P et al (2002) Factors that predict morbidity and mortality in patients with perforated peptic ulcers. Eur J Surg 168:446–451
Billing A, Frohlich D, Schildberg FW (1994) Prediction of outcome using the Mannheim peritonitis index in 2003 patients. Peritonitis Study Group. Br J Surg 81:209–213
Kocer B, Surmeli S, Solak C et al (2007) Factors affecting mortality and morbidity in patients with peptic ulcer perforation. J Gastroenterol Hepatol 22:565–570
Janik J, Chwirot P (2000) Perforated peptic ulcer–time trends and patterns over 20 years. Med Sci Monit 6:369–372
Lanas A, Serrano P, Bajador E et al (1997) Evidence of aspirin use in both upper and lower gastrointestinal perforation. Gastroenterology 112:683–689
Siu WT, Chau CH, Law BK et al (2004) Routine use of laparoscopic repair for perforated peptic ulcer. Br J Surg 91:481–484
Barczynski M, Res F, Cichon S et al (1999) Perioperative mortality for perforated duodenal and gastric ulcer—analysis of 226 patients. Przegl Lek 56:192–197
Calam J, Baron JH (2001) ABC of the upper gastrointestinal tract: pathophysiology of duodenal and gastric ulcer and gastric cancer. BMJ 323:980–982
Hojgaard L, Mertz Nielsen A et al (1996) Peptic ulcer pathophysiology: acid, bicarbonate, and mucosal function. Scand J Gastroenterol Suppl 216:10–15
Debongnie JC, Wibin E, Timmermans M et al (1995) Are perforated gastroduodenal ulcers related to Helicobacter pylori infection? Acta Gastroenterol Belg 58:208–212
Gilliam AD, Speake WJ, Lobo DN et al (2003) Current practice of emergency vagotomy and Helicobacter pylori eradication for complicated peptic ulcer in the United Kingdom. Br J Surg 90:88–90
Serejo LG, da Silva-Junior FP, Bastos JP et al (2007) Risk factors for pulmonary complications after emergency abdominal surgery. Respir Med 101:808–813
Mangram AJ, Horan TC, Pearson ML et al (1999) Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20:250–278
Arias CA, Quintero G, Vanegas BE et al (2003) Surveillance of surgical site infections: decade of experience at a Colombian tertiary care center. World J Surg 27:529–533
So JB, Yam A, Cheah WK et al (2000) Risk factors related to operative mortality and morbidity in patients undergoing emergency gastrectomy. Br J Surg 87:1702–1707
Lunevicius R, Morkevicius M (2005) Systematic review comparing laparoscopic and open repair for perforated peptic ulcer. Br J Surg 92:1195–1207
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lohsiriwat, V., Prapasrivorakul, S. & Lohsiriwat, D. Perforated Peptic Ulcer: Clinical Presentation, Surgical Outcomes, and the Accuracy of the Boey Scoring System in Predicting Postoperative Morbidity and Mortality. World J Surg 33, 80–85 (2009). https://doi.org/10.1007/s00268-008-9796-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9796-1